Load FindZebra Summary
Disclaimer:
FindZebra Search conducts a search using our specialized medical search engine.
FindZebra Summary uses the text completions API
(subject to OpenAI’s API data usage policies)
to summarize and reason about the search results.
The search is conducted in publicly available information on the Internet that we present “as is”.
You should be aware that FindZebra is not supplying any of the content in the search results.
FindZebra Summary is loading...
-
Steroid Diabetes
Wikipedia
Mechanism [ edit ] Glucocorticoids oppose insulin action and stimulate gluconeogenesis , especially in the liver , resulting in a net increase in hepatic glucose output. ... Criteria [ edit ] The diagnostic criteria for steroid diabetes are those of diabetes (fasting glucoses persistently above 125 mg/dl (7 mM) or random levels above 200 mg/dl (11 mM)) occurring in the context of high-dose glucocorticoid therapy.
-
Myasthenia Gravis
Wikipedia
Relatives of people with MG have a higher percentage of other immune disorders. [22] [23] The thymus gland cells form part of the body's immune system. ... Both of these treatments have relatively short-lived benefits, typically measured in weeks, and often are associated with high costs, which make them prohibitive; they are generally reserved for when MG requires hospitalization. [49] [52] Surgery [ edit ] As thymomas are seen in 10% of all people with the MG, they are often given a chest X-ray and CT scan to evaluate their need for surgical removal of their thymus glands and any cancerous tissue that may be present. [18] [37] Even if surgery is performed to remove a thymoma, it generally does not lead to the remission of MG. [49] Surgery in the case of MG involves the removal of the thymus, although in 2013, no clear benefit was indicated except in the presence of a thymoma. [53] A 2016 randomized, controlled trial, however, found some benefits. [54] Physical measures [ edit ] People with MG should be educated regarding the fluctuating nature of their symptoms, including weakness and exercise-induced fatigue. ... Archived from the original on 8 September 2017. ^ a b c d e f g h i j Engel AG (2012). Myasthenia Gravis and Myasthenic Disorders (2nd ed.). ... Cite journal requires |journal= ( help ) ^ a b c d e f g h Nair AG, Patil-Chhablani P, Venkatramani DV, Gandhi RA (October 2014). ... Retrieved 11 July 2015 . ^ a b c d e f g h Kumar V, Kaminski HJ (February 2011).CFB, HLA-B, MUSK, HLA-DPB1, POMC, FAS, HLA-DRB1, HLA-DQA1, PTPN22, HLA-A, TNIP1, C2, IL10, NFKBIL1, ZNRD1, MUC21, SFTA2, HCG9, PSORS1C1, CTLA4, NOTCH4, MUCL3, CYP21A2, RBM45, BTNL2, GPSM3, MSH5, TSBP1, MICB, LRP4, TRIM31, POU5F1, HLA-DQA2, RNF39, GABBR1, VARS2, LINC00243, ABCF1, IFNG, MSH5-SAPCD1, HCG17, TNFRSF11A, TCF19, BCHE, ATP6V1G2, STK19, TNF, HCG18, GPANK1, SEMA5A, TTN, TSBP1-AS1, RBBP8, ACHE, PRRC2A, CXCL13, IL17A, IL2RA, IL6, ISG20, EIF3K, IL2, FOXP3, AIRE, IL4, CHRNA1, TRBV20OR9-2, HLA-DQB1, THM, LTA, IL1B, CD274, IL22, PDCD1, IL21, TLR9, CHRNE, IL1A, MIR150, AQP4, HT, TGFB1, CDR3, ECD, MIR21, DOK7, TLR4, CD40, TLR3, MBP, CCL21, CHRNA4, TAP2, CXCR4, IGHG3, IFNB1, MAPK1, PDLIM7, IL18R1, IL15, EBI3, IL4R, SMN1, CXCL10, IFNA13, TLR7, TNFRSF13C, FGFR3, MIR146A, ESR1, TSLP, CD40LG, GNAO1, DNMT3B, HLA-DQB2, CAV3, IL23A, MIR125A, ADRB2, IFNA1, IFN1@, HMGB1, C4orf3, DIPK1A, SOCS3, LGI1, MSC, SCO2, CD83, GRAP2, MIR145, MIRLET7C, NTN1, MIR155, PPP6R2, MIR143, MBTPS1, MIR15B, SCFV, LOC102723407, IFNG-AS1, LINC-ROR, C4B_2, C20orf181, TEC, CCR2, DDX39B, MIR653, MIR323B, MIR19B1, MIR338, AIMP2, FOSL1, MIR320A, USO1, TNFRSF25, MIR30E, MALAT1, TNFSF10, DDX39A, RMDN2, MYAS1, CCAR2, RNF19A, CNTNAP2, HIF3A, ROBO3, POLDIP2, IFIH1, IGAN1, B3GAT1, DPYSL5, PART1, RETN, IGHV3-52, TWNK, MSL2, KRT20, ICOS, SLC25A37, VAV1, TMEM109, PPP1R15A, PRSS16, UNC5A, CLEC4C, CDIPT, NXF1, MZB1, TRIM9, AHSA1, IL17F, IL33, TNFSF13B, DDX58, CCR9, FHDC1, LILRB1, FAM136A, SLC7A9, TBC1D9, ICOSLG, SEC14L2, VIP, RAF1, UTRN, CNTFR, CRK, MAPK14, CSF1, CCN2, CTSV, CTSS, CYP3A5, CD55, BRINP1, DCC, DNMT3A, ATN1, TYMP, CTTN, ERBB4, ESR2, FCGR2A, FLNB, FOS, FOSB, CXCR3, GRIA2, GRM2, CXCL1, GZMB, HLA-C, HLA-DOA, HLA-DPA1, HLA-DRB3, CR2, CCR7, HNMT, CCR5, ADCYAP1, AGER, ALB, APOE, APRT, ABCC6, BCL2, TNFRSF17, BDNF, C4A, C4B, C5, CA3, CACNA1S, CALCA, CALCR, CAMP, CASP1, CASP3, CD19, MS4A1, CD28, CD86, CD69, CDS1, CHRNB1, CHRND, CLC, CCR4, HLA-G, HOXD13, TYMS, NTRK1, P2RX7, PAM, PAX7, ABCB1, PMP22, MAPK3, PTPRC, PLAAT4, RELB, S100A8, S100A11, S100B, SCN4A, SCO1, CCL5, CCL17, CCL22, CXCL12, SGCA, SLAMF1, SMN2, SPP1, STAT3, STAT4, TAP1, THBS1, TNFAIP3, TNFSF4, TNFRSF4, OSM, NCAM1, HSPA5, MYOG, IRF8, IFNA2, IFNA17, IFNGR1, IGF1, IGF1R, IGFBP1, IGL, IL1RN, IL2RB, IL7R, IL9, IL12B, IL12RB2, INS, IRF4, ITGAX, JUN, JUNB, JUND, KIT, KRT5, LDLR, LGALS1, LGALS8, LIF, MEFV, MFAP1, MMP10, LOC102724971
-
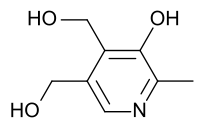
Pyridoxine-Dependent Epilepsy
Wikipedia
The disorder was first recognized in the 1950s, with the first description provided by Hunt et al. in 1954. [1] [2] [3] More recently, pathogenic variants within the ALDH7A1 gene have been identified to cause PDE. [1] [2] [3] [4] Contents 1 Genetics 2 Treatment 3 Monitoring 4 References 5 External links Genetics [ edit ] PDE is inherited in an autosomal recessive manner and is estimated to affect around 1 in 400,000 to 700,000 births, though one study conducted in Germany estimated a prevalence of 1 in 20,000 births. [1] [2] The ALDH7A1 gene encodes for the enzyme antiquitin or α -aminoadipic semialdehyde dehydrogenase, which is involved with the catabolism of lysine . [1] [2] [4] [5] Treatment [ edit ] Patients with PDE do not respond to anticonvulsant medications, but seizures rapidly cease with therapeutic intravenous doses of Vitamin B6 and remission from seizures are often maintained on daily therapeutic doses of Vitamin B6. [1] [2] [5] An optimal dose has not yet been established, but doses of 50–100 mg/day or 15–30 mg/kg/day have been proposed. [1] [2] Importantly, excessive doses of vitamin B6 can result in irreversible neurological damage, and therefore several guidelines recommend between 200 mg (neonates) and 500 mg per day as the maximal daily dose. [1] [2] Despite remission of seizure activity with vitamin B6 supplementation, intellectual disability is frequently seen in patients with PDE. [2] [6] Because the affected enzyme antiquitin is involved in the cerebral lysine degradation pathway, lysine restriction as an additional treatment modality has recently been explored. Studies have been published which demonstrate potential for improved biomarkers, development, and behavior in patients treated with lysine restriction in addition to pyridoxine supplementation. [2] [6] In trial, lysine restriction of 70–100 mg/kg/day in children less than 1 year of age, 45–80 mg/kg/day in children between 1–7 years of age, and 20–45 mg/kg/day in children older than 7 years of age were prescribed. [6] Despite the potential of additional benefit from lysine restriction, vitamin B6 supplementation remains the main-stay of treatment given lack of studies thus far demonstrating the safety and efficacy of lysine restriction for this purpose. ... Retrieved June 19, 2014 . ^ a b c d e f g h i j k l Stockler, S; Plecko, B; Gospe, SM; Coulter-Mackie, M; et, al. ... PMID 21704546 . ^ a b Shih, JJ; Kornblum, H; Shewmon, DA (September 1996). "Global brain dysfunction in an infant with pyridoxine dependency: evaluation with EEG, evoked potentials, MRI, and PET" . ... PMID 21926623 . ^ a b c d van Karnebeek, CDM; Hartmann, H; Jaggumantri, S; Bok, LA; et, al.
-
Ocular Myasthenia
Wikipedia
MG may be limited to the muscles of the eye (ocular MG), leading to abrupt onset of weakness/fatigability of the eyelids or eye movement. MG may also involve other muscle groups ( generalized MG ). ... Diagnosis [ edit ] The variable course of MG may make the diagnosis difficult. ... Treatment [ edit ] The prognosis tends to be good for patients with MG. It is often best not to treat mild cases of MG. ... The symptoms of ocular MG can also be addressed by non-medicinal means.
-
Hypoglycemia
Wikipedia
Research in healthy adults shows that mental efficiency declines slightly but measurably as blood glucose falls below 3.6 mmol/l (65 mg/dl). Hormonal defense mechanisms ( adrenaline and glucagon ) are normally activated as it drops below a threshold level (about 3.0 mmol/l (55 mg/dl) for most people), producing the typical hypoglycemic symptoms of shakiness and dysphoria . [10] : 1589 Obvious impairment may not occur until the glucose falls below 2.2 mmol/l (40 mg/dl), and many healthy people may occasionally have glucose levels below 3.6 mmol/l (65 mg/dl) in the morning without apparent effects. ... In most people, subtle reduction of mental efficiency can be observed when the glucose falls below 3.6 mmol/l (65 mg/dl). Impairment of action and judgment usually becomes obvious below 2.2 mmol/l (40 mg/dl). ... If IV access cannot be established, the person can be given 1 to 2 mg of glucagon in an intramuscular injection . ... Retrieved 28 June 2015 . ^ a b c Yanai H, Adachi H, Katsuyama H, Moriyama S, Hamasaki H, Sako A (February 2015). ... PMID 11026531 . ^ de Pasqua A, Mattock MB, Phillips R, Keen H (1984). "Errors in blood glucose determination".ABCC8, IGF2, SERAC1, HNF1A, INS, IL1B, TNF, SOD2, CACNA1C, GSR, SERPINA1, PPARA, CRH, PNMT, TH, GH1, GRIN2B, IGF1, G6PC, INSR, KCNJ11, HNF4A, ACADM, CPT1A, HADHA, GHSR, TANGO2, PGM1, HADH, PC, SETD2, AGL, PCK1, NR3C1, MEN1, MPI, TFAM, DBH, EIF2AK3, EIF2S3, ETFDH, NDUFS2, PTEN, FBP1, UQCRC2, GHR, SLC22A5, SLC37A4, HMGCL, UQCRB, NFKB2, PURA, GLI2, GLP1R, MPC1, NBAS, HSD17B10, NR1H4, PYGL, NDUFAF1, ROBO1, HMGCS2, TIMMDC1, HRAS, MRPS2, SEPSECS, RARB, WARS2, KCNMA1, NDUFS3, NDUFS4, NDUFS6, NDUFS8, NDUFV2, PPP2R5D, NOTCH3, OTC, OTX2, PPM1B, PCCA, PCCB, PCK2, NNT, GPR161, PHKA2, POU1F1, MLYCD, NDUFV1, NDUFS1, MRPS7, NDUFB10, CDON, PROP1, NDUFAF4, ACAD9, LRPPRC, APC2, NDUFB11, NDUFAF3, MPV17, MTO1, ND1, ND2, ND3, NDUFA1, NDUFA6, NDUFB3, NDUFB9, GPC3, GJA1, GK, PROKR2, SLC35A2, CA5A, SLC25A20, MICOS13, COG7, NDUFAF2, LHX4, COG8, NUBPL, CAMKMT, EHMT1, CYB561, NDUFAF5, DBT, CTDP1, DGUOK, DLD, NDUFA11, SGPL1, NSD1, BCS1L, ACADSB, KCNMA1-AS1, ACAT1, SUCLG1, ZGLP1, UQCC3, HESX1, ALDOB, NDUFS7, GOLGA6A, PTF1A, ACSF3, ATP5F1D, ATP7A, AUH, BCKDHA, BCKDHB, DPP4, CYP21A2, MTOR, GALT, FAH, RCBTB1, GPC4, PNPO, SLC52A1, MCCC2, PREPL, GCDH, WDR11, GCG, RNF125, GCK, SLC5A2, SAMD9, SLC3A1, DMXL2, FOXRED1, POMC, SOX3, MCCC1, ETFA, ETFB, TMEM126B, CYP2C9, ALB, SLC2A4, ACE, DSPP, FFAR1, SI, MGAM, SLC2A1, AKT2, GLUD1, HIF1A, NPY, SST, VEGFA, PRL, PIK3CA, ADRB2, TXN, KCNH2, GPR119, SLC5A1, UCP2, SLC2A2, IGFBP3, NFE2L2, SELENBP1, MAPK8, PPP1R13L, SHBG, ADIPOQ, TXNIP, SLC2A3, RNH1, PRKAA1, REN, AKT3, PIK3CG, PIK3CD, KDR, APRT, BDNF, ANTXR2, CPT2, CHPT1, GABPA, GDF1, CCHCR1, SHC3, GPT, HK1, IAPP, IL6, GIP, ARFIP2, PIK3CB, MFAP1, DNM1L, KCNH6, ARID1B, KL, MTA2, SEMA6A, SLC16A7, LPAR2, PDIA2, FTO, DHDDS, SOCS3, DAPK2, RPAIN, TIGAR, SLC52A3, SORCS1, CXCR6, CPT1C, SLC39A14, TBPL2, MIR155, MIR665, EMSLR, RIPK1, IRS2, KHSRP, TMPRSS11D, ACKR3, SOCS7, SH3BP1, GAL, ERO1A, PIAS1, HNRNPDL, CRYL1, PADI1, HGH1, FGF19, SIRT6, GLS2, KEAP1, RAPGEF5, WWOX, UQCRQ, KMT2B, DCAF1, FGF21, ROBO4, BNC2, DEPP1, VPS13C, TUBB3, H6PD, TMEM132A, MARCHF1, DENR, ACADL, MLRL, AAAS, TIMM8A, DNMT1, ARID3A, DSC3, EDNRA, EGFR, ELAVL1, ENO1, ENO2, ERBB4, ESRRA, F2R, F3, FBN1, FGF1, FGF2, FOS, NR5A1, GCGR, GHRH, GHRHR, GIPR, GLA, GCLC, GPER1, GPR42, GRIN1, GSK3B, GYS1, CYP2C8, CTNNB1, CRMP1, BID, ACADVL, ADCY5, ADRA1A, ADRA2B, AHR, AIF1, AKT1, APOE, APP, AQP4, AQP7, ARNT, AVP, BRS3, CRIP1, C3, CALD1, CCND2, CD34, CD36, CD59, LRBA, CDH15, CEBPA, CHAT, CHGA, CKB, CREM, FOXA2, HNRNPC, HNRNPL, SSTR4, PRKAR1A, PSMB9, PTHLH, RAD21, RB1, RIT2, RORC, SELP, SIAH2, ST3GAL4, SLC16A1, SLC22A1, SREBF1, STAR, PRKAA2, STAT5A, STAT5B, SYK, TAP1, TCF7L2, TGM2, TP53, TRH, UGDH, UTRN, VCAM1, CNBP, KMT2D, PRKAB1, PPY, AGFG1, MC4R, HTC2, IFNG, IGFBP6, KCNQ1, KHK, KIT, LEP, LEPR, LGALS1, LIPE, LPL, SMAD3, MAFD2, MET, PTPA, NR3C2, MTHFR, NHS, NUCB2, P4HB, PECAM1, PFKFB3, ABCB1, PIK3R2, POR, POU2F1, PPARD, PPARG, LOC102723407
-
Androgen Deficiency
Wikipedia
The Food and Drug Administration (FDA) stated in 2015 that neither the benefits nor the safety of testosterone have been established for low testosterone levels due to aging . [6] The FDA has required that testosterone pharmaceutical labels include warning information about the possibility of an increased risk of heart attacks and stroke. [6] v t e Androgen replacement therapy formulations and dosages used in men Route Medication Major brand names Form Dosage Oral Testosterone a – Tablet 400–800 mg/day (in divided doses) Testosterone undecanoate Andriol, Jatenzo Capsule 40–80 mg/2–4x day (with meals) Methyltestosterone b Android, Metandren, Testred Tablet 10–50 mg/day Fluoxymesterone b Halotestin, Ora-Testryl, Ultandren Tablet 5–20 mg/day Metandienone b Dianabol Tablet 5–15 mg/day Mesterolone b Proviron Tablet 25–150 mg/day Buccal Testosterone Striant Tablet 30 mg 2x/day Methyltestosterone b Metandren, Oreton Methyl Tablet 5–25 mg/day Sublingual Testosterone b Testoral Tablet 5–10 mg 1–4x/day Methyltestosterone b Metandren, Oreton Methyl Tablet 10–30 mg/day Intranasal Testosterone Natesto Nasal spray 11 mg 3x/day Transdermal Testosterone AndroGel, Testim, TestoGel Gel 25–125 mg/day Androderm, AndroPatch, TestoPatch Non-scrotal patch 2.5–15 mg/day Testoderm Scrotal patch 4–6 mg/day Axiron Axillary solution 30–120 mg/day Androstanolone ( DHT ) Andractim Gel 100–250 mg/day Rectal Testosterone Rektandron, Testosteron b Suppository 40 mg 2–3x/day Injection ( IM or SC ) Testosterone Andronaq, Sterotate, Virosterone Aqueous suspension 10–50 mg 2–3x/week Testosterone propionate b Testoviron Oil solution 10–50 mg 2–3x/week Testosterone enanthate Delatestryl Oil solution 50–250 mg 1x/1–4 weeks Xyosted Auto-injector 50–100 mg 1x/week Testosterone cypionate Depo-Testosterone Oil solution 50–250 mg 1x/1–4 weeks Testosterone isobutyrate Agovirin Depot Aqueous suspension 50–100 mg 1x/1–2 weeks Testosterone phenylacetate b Perandren, Androject Oil solution 50–200 mg 1x/3–5 weeks Mixed testosterone esters Sustanon 100, Sustanon 250 Oil solution 50–250 mg 1x/2–4 weeks Testosterone undecanoate Aveed, Nebido Oil solution 750–1,000 mg 1x/10–14 weeks Testosterone buciclate a – Aqueous suspension 600–1,000 mg 1x/12–20 weeks Implant Testosterone Testopel Pellet 150–1,200 mg/3–6 months Notes: Men produce about 3 to 11 mg testosterone per day (mean 7 mg/day in young men).
-
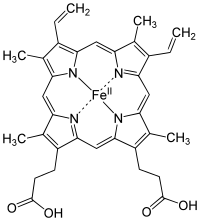
Iron Deficiency
Wikipedia
Signs and symptoms in children [ edit ] pale skin fatigue slowed growth and development poor appetite behavioral problems abnormal rapid breathing frequent infection Iron requirements in young children to teenagers [ edit ] Age group Recommended amount of iron a day [7] 7 – 12 months 11 mg 1 – 3 years 7 mg 4 – 8 years 10 mg 9 – 13 years 8 mg 14 – 18 years, girls 15 mg 14 – 18 years, boys 11 mg Causes [ edit ] blood loss ( hemoglobin contains iron) donation excessive menstrual bleeding non-menstrual bleeding bleeding from the gastrointestinal tract ( ulcers , hemorrhoids , ulcerative colitis , stomach or colon cancer , etc.) rarely, laryngological bleeding or from the respiratory tract inadequate intake (see below) substances (in diet or drugs) interfering with iron absorption Fluoroquinolone antibiotics [8] malabsorption syndromes inflammation where it is adaptive to limit bacterial growth in infection, but is also present in many other chronic diseases such as Inflammatory bowel disease and rheumatoid arthritis parasitic infection Though genetic defects causing iron deficiency have been studied in rodents, there are no known genetic disorders of human iron metabolism that directly cause iron deficiency. ... Reflecting this link between iron bioavailability and bacterial growth, the taking of oral iron supplements in excess of 200 mg/day causes a relative overabundance of iron that can alter the types of bacteria that are present within the gut. ... Arbitrarily, the guideline is set at 18 mg, which is the USDA Recommended Dietary Allowance for women aged between 19 and 50. [29] Abstract: richest foods in heme iron Food Serving size Iron % guideline clam [a] 100g 28 mg 155% pork liver 100g 18 mg 100% lamb kidney 100g 12 mg 69% cooked oyster 100g 12 mg 67% cuttlefish 100g 11 mg 60% lamb liver 100g 10 mg 57% octopus 100g 9.5 mg 53% mussel 100g 6.7 mg 37% beef liver 100g 6.5 mg 36% beef heart 100g 6.4 mg 35% Abstract: richest foods in non-heme iron Food Serving size Iron % guideline raw yellow beans 100g 7 mg 35% spirulina 15g 4.3 mg 24% falafel 140g 4.8 mg 24% soybean kernels 125ml=1/2cup 4.6 mg 23% spinach 125g 4.4 mg 22% lentil 125ml=1/2cup 3.5 mg 17.5% treacle (CSR Australia) 20ml=1Tbsp 3.4 mg 17% molasses (Bluelabel Australia) 20ml=1Tbsp 1.8 mg 9% candied ginger root 15g~3p 1.7 mg 8.5% toasted sesame seeds 10g 1.4 mg 7% cocoa (dry powder) 5g~1Tbsp .8 mg 4% Food recommendations for children [ edit ] Children at 6 months should start having solid food that contains enough iron, which could be found in both heme and non-heme iron [33] Heme iron : Red meat (for example, beef, pork, lamb, goat, or venison) Fatty fish Poultry (for example, chicken or turkey) Eggs Non-heme iron : Iron-fortified infant cereals Tofu Beans and lentils Dark green leafy vegetables Iron deficiency can have serious health consequences that diet may not be able to quickly correct; hence, an iron supplement is often necessary if the iron deficiency has become symptomatic. ... World Health Organization . 2002. ^ Wintergerst, E. S.; Maggini, S.; Hornig, D. H. (2007). "Contribution of Selected Vitamins and Trace Elements to Immune Function" (PDF) . ... PMID 26060840 . ^ Fang, Zhan-Qiang; Cheung, R. Y. H.; Wong, M. H. (January 2003). "Heavy metals in oysters, mussels and clams collected from coastal sites along the Pearl River Delta, South China".EPO, TMPRSS6, SLC11A2, HFE, TFRC, HAMP, CRP, FGF23, HBA2, CHMP2B, DMRT1, HIF1A, IL1B, SLC40A1, EPAS1, HEPH, PMCH, BDNF, HBA1, CP, AIF1, RET, IREB2, IL6, SLC39A1, ATF4, PARP3, RN7SL263P, HMOX1, TNF, ALB, IDUA, FECH, LCN2, ACAD8, FXN, ERFE, BDH2, CYBRD1, RLS1, TFR2, TDGF1P3, ACO1, RPP14, ZFP36, SUB1, PPARGC1A, AHSA1, AIMP2, KHSRP, STK16, AKR1A1, CDKL1, BCAP31, CDK2AP2, GRAP2, DNALI1, HDAC3, EIF2S2, SLC39A7, NOL3, GOSR1, XPR1, MLLT10, PSIP1, GSTO1, ABCG2, ABO, SETD2, SIRT2, SLC36A1, ZGPAT, COX19, SLC46A1, CYGB, OLIG1, HJV, IL27, XYLT2, COPD, SLC39A5, CYCSP51, NUP43, H3P8, H3P24, HHIP, NLN, JMJD6, UBE2D1, CRTC1, CDK20, RNF19A, POLDIP2, SIGLEC7, LAMTOR2, TMED5, SLC39A10, SLC25A37, NCKIPSD, SF3B6, NANS, AHI1, SMARCAD1, VHL, SST, TYS, CUX1, DNAH8, EBF1, EDN1, EIF2S1, EIF2S3, ESR1, ETV3, G6PD, GATA1, GPI, HCLS1, HP, PRMT1, IFNG, IGF1, DAPK3, CTSL, TTR, MAPK14, ACP5, APEX1, ARG1, ARSA, ATP4A, BACH1, BSG, CAT, CCK, CDKN2A, CENPF, CLN3, SLC31A1, CRK, CRYGD, IL1A, IL2RB, CXCL8, SMAD1, RPL29, S100A9, TSPAN31, SAT1, SLC2A1, SLC11A1, SOD1, ST13, STAT3, STAT5A, STAT5B, CNTN2, TCF3, TNFRSF1B, TST, REN, PRPH2, PVALB, PDE7A, SMAD7, MMP9, MPO, NGF, NUCB2, REG3A, CFP, PTH, PPARG, MAPK1, PRNP, RELN, PSMC6, PSMD10, H3P30
-
Genetic Primary Hypomagnesemia
Orphanet
A rare mineral absorption and transport disorder characterized by a selective defect in renal or intestinal magnesium (Mg) absorption, resulting in a low Mg concentration in the blood. ... Diagnosis is also established by simultaneous evaluation of serum Mg and urinary Mg excretion. Presence of hypomagnesemia with adapted urinary Mg excretion (<1mmol/24h or fractional excretion (FE) < 1%) indicates an extra renal origin. Elevated fecal Mg levels indicate an intestinal defect. In contrast, hypomagnesemia with increased urinary Mg excretion (> 2 mmol/24h or FE >2%) indicates a renal origin. ... Management and treatment Treatment of FPH involves substitution with oral Mg. In cases of intolerance, patients may be treated with intramuscular Mg sulfate.
-
Familial Primary Hypomagnesemia With Normocalciuria And Normocalcemia
Orphanet
A form of familial primary hypomagnesemia (FPH), characterized by low serum magnesium (Mg) values but inappropriate normal urinary Mg values (i.e. renal hypomagnesemia). ... As a consequence, the renal EGF receptor (EGFR) is inadequately stimulated, resulting in insufficient activation of the epithelial Mg channel TRPM6 and thereby Mg loss. Thus, a renal Mg reabsorption defect is observed due to the inability of the kidney to reduce urinary Mg excretion under low serum Mg conditions. Diagnostic methods Diagnosis relies on laboratory findings revealing severely lowered serum Mg values in the absence of other electrolyte disturbances, normocalcemia, low to normal urinary calcium (Ca) values and normal urinary Mg values. ... Management and treatment Treatment of FPHNN is mainly symptomatic and includes the Mg substitution therapy. Prognosis Severity of the disease is variable.
-
Albuminuria
Wikipedia
The nephrotic syndrome usually results in the excretion of about 3.0 to 3.5 grams per 24 hours. [ medical citation needed ] Nephritic syndrome results in far less albuminuria. [ medical citation needed ] Microalbuminuria (between 30 and 300 mg/24h, [2] mg/l of urine [3] or μg/mg of creatinine [4] ) can be a forerunner of diabetic nephropathy . The term albuminuria is now preferred in Nephrology since there is not a "small albumin" ( micro albuminuria) or a "big albumin" ( macro albuminuria). [5] A1 represents normal to mildly increased urinary albumin/creatinine ratio (<30 mg/g or < 3 mg/mmmol); A2 represents moderately increased urinary albumin/creatinine ratio (30–300 mg/g or 3–30 mg/mmmol, previously known as microalbuminuria ); and A3 reflects severely increased urinary albumin/creatinine ratio >300 mg/g or > 30 mg/mmol). [1] Diagnosis [ edit ] The amount of protein being lost in the urine can be quantified by collecting the urine for 24 hours, measuring a sample of the pooled urine, and extrapolating to the volume collected. ... "Albumin-to-creatinine ratio in random urine samples might replace 24-h urine collections in screening for micro- and macroalbuminuria in pregnant woman with type 1 diabetes" .ACE, INS, TNF, PTGS2, NCK1, TSLP, REN, LEPR, IL6, GNAQ, SOD2, MIR130A, GPC5, MIR145, NPHS1, NPHS2, MIR155, CP, MIR424, CD38, NCK2, CASP1, PYCARD, AGT, TRPC3, TRPC6, SPP1, SH2B3, PDPN, AGER, LRP2, CSF1, ALB, EDN1, CYP11B1, CTSL, CTSB, RAB38, CASR, BAHCC1, HOTTIP, ARL15, LINC00862, CHD7, C2orf83, FBXL20, SHROOM3, SPATA5L1, ICA1L, SBF2, LRMDA, ADO, AK5, LINC02752, MAPKBP1, CPS1, CCT2, CWC27, USP3, SNX17, NRXN1, CUBN, AHR, AQP7, COL4A4, NMU, PEX1, MYL3, GALT, FUT1, CCL2, DCN, CCL5, SELP, VEGFA, ADD1
-
Microalbuminuria
Wikipedia
Microalbuminuria can be diagnosed from a 24-hour urine collection (between 30–300 mg/24 hours) or, more commonly, from elevated concentration in a spot sample (20 to 200 mg/l). ... This is termed the albumin/creatinine ratio (ACR) [10] and microalbuminuria is defined as ACR ≥3.5 mg/mmol (female) or ≥2.5 mg/mmol (male), [11] or with both substances measured by mass, as an ACR between 30 and 300 µg albumin/mg creatinine. [12] For the diagnosis of microalbuminuria, care must be taken when collecting sample for the urine ACR. ... This is due to the variation in creatinine level which is produced by the muscle. [13] Definitions of microalbuminuria Individual Lower limit Upper limit Unit 24h urine collection 30 [9] 300 [9] mg/24h ( milligram albumin per 24 hours) Short-time urine collection 20 [9] 200 [9] µg/min ( microgram albumin per minute) Spot urine albumin sample 30 [14] 300 [14] mg/L (milligram albumin per liter of urine) Spot urine albumin/creatinine ratio Women 3.5 [15] 25 [15] or 35 [15] mg/mmol (milligram albumin per millimole creatinine) 30 [15] 400 [15] μg/mg (microgram albumin per milligram creatinine) Men 2.5 [15] or 3.5 [15] 25 [15] or 35 [15] mg/mmol 30 [15] 300 [15] μg/mg References [ edit ] Abid O, Sun Q, Sugimoto K, Mercan D, Vincent JL (2001). ... PMID 10913814 . Parving HH, Lehnert H, Bröchner-Mortensen J, Gomis R, Andersen S, Arner P (2001). ... J.; Hunt, R.; Goodwin, A.; Gross, J. L.; Keen, H.; Viberti, G. C. (1987-01-01). "Dietary composition and renal function in healthy subjects".
-
Juvenile Myasthenia Gravis
Orphanet
Juvenile myasthenia gravis (MG; see this term) is a rare form of MG, an autoimmune disorder of the neuromuscular junction resulting in ocular manifestations or generalized weakness, with onset before 18 years of age. Epidemiology The exact prevalence and incidence of juvenile MG are not known. Estimated incidence has been reported at 1/1,000,000 to 1/200,000. ... The proportion of patients having only ocular symptoms is higher than in adult MG, particularly in the prepubertal group in which half of cases are purely ocular. ... Thymoma (see this term) development is rare in juvenile MG. Etiology The exact pathogenesis is not known but MG is related to circulating antibodies to various muscle receptors, including, in most of patients, acetylcholine receptor (AChR) and, rarely, muscle-specific receptor tyrosine kinase (MuSK). ... In the prepubertal form, there is a high rate of the MG form with no antibodies detectable (30-50%).
-
Meier-Gorlin Syndrome
GARD
Meier-Gorlin syndrome (MGS) is a very rare inherited condition characterized by very small ears and ear canals, short stature, and absent or very small kneecaps (patellae). ... Females with MGS may have underdeveloped breasts. ... Most forms of MGS are inherited in an autosomal recessive pattern. The form caused by the GMNN gene is inherited in an autosomal dominant pattern. MGS is diagnosed based on the clinical signs and symptoms. ... Most people with this syndrome have normal lifespans. The exact prevalence of MGS has not been determined, but is estimated to be less than 1-9/1,000,000.ORC1, CDT1, GMNN, ORC6, CDC6, ORC4, CDC45, BMP5, DRD2, SLC6A3, CYP2D6, MAPK1, MYH9, TLR4, MTOR, RBP4, MCM5, PSEN1, COMT, PTH, MAPK3, SOD1, RELA, PRKCA, PRKACG, RGS2, ATXN2, SLC18A2, VEGFA, SYT1, TGFB1, TNF, PIK3CG, PDPN, POSTN, CHEK2, PLCB1, SIRT1, ORC3, DISC1, CLEC7A, GORASP1, WNK1, PLA2G4A, ACTG1, PIK3CA, HTR2A, ASPH, BRCA2, BSG, CD2, COL1A1, CRP, CCN2, DRD3, EPHB2, FANCD2, FASN, FOXM1, GNAS, GRIK3, IL6, SERPINE1, IL10, INSR, ITPR1, LEP, CYP4F3, LY6E, LYZ, MAOB, MCM2, ATXN3, NOS2, ACTB, APOE, PAEP, ACHE
-
Hypogonadism
Wikipedia
Clomifene at much higher doses is used to induce ovulation and has significant adverse effects in such a setting. v t e Androgen replacement therapy formulations and dosages used in men Route Medication Major brand names Form Dosage Oral Testosterone a – Tablet 400–800 mg/day (in divided doses) Testosterone undecanoate Andriol, Jatenzo Capsule 40–80 mg/2–4x day (with meals) Methyltestosterone b Android, Metandren, Testred Tablet 10–50 mg/day Fluoxymesterone b Halotestin, Ora-Testryl, Ultandren Tablet 5–20 mg/day Metandienone b Dianabol Tablet 5–15 mg/day Mesterolone b Proviron Tablet 25–150 mg/day Buccal Testosterone Striant Tablet 30 mg 2x/day Methyltestosterone b Metandren, Oreton Methyl Tablet 5–25 mg/day Sublingual Testosterone b Testoral Tablet 5–10 mg 1–4x/day Methyltestosterone b Metandren, Oreton Methyl Tablet 10–30 mg/day Intranasal Testosterone Natesto Nasal spray 11 mg 3x/day Transdermal Testosterone AndroGel, Testim, TestoGel Gel 25–125 mg/day Androderm, AndroPatch, TestoPatch Non-scrotal patch 2.5–15 mg/day Testoderm Scrotal patch 4–6 mg/day Axiron Axillary solution 30–120 mg/day Androstanolone ( DHT ) Andractim Gel 100–250 mg/day Rectal Testosterone Rektandron, Testosteron b Suppository 40 mg 2–3x/day Injection ( IM or SC ) Testosterone Andronaq, Sterotate, Virosterone Aqueous suspension 10–50 mg 2–3x/week Testosterone propionate b Testoviron Oil solution 10–50 mg 2–3x/week Testosterone enanthate Delatestryl Oil solution 50–250 mg 1x/1–4 weeks Xyosted Auto-injector 50–100 mg 1x/week Testosterone cypionate Depo-Testosterone Oil solution 50–250 mg 1x/1–4 weeks Testosterone isobutyrate Agovirin Depot Aqueous suspension 50–100 mg 1x/1–2 weeks Testosterone phenylacetate b Perandren, Androject Oil solution 50–200 mg 1x/3–5 weeks Mixed testosterone esters Sustanon 100, Sustanon 250 Oil solution 50–250 mg 1x/2–4 weeks Testosterone undecanoate Aveed, Nebido Oil solution 750–1,000 mg 1x/10–14 weeks Testosterone buciclate a – Aqueous suspension 600–1,000 mg 1x/12–20 weeks Implant Testosterone Testopel Pellet 150–1,200 mg/3–6 months Notes: Men produce about 3 to 11 mg testosterone per day (mean 7 mg/day in young men). ... ISBN 978-1609611019 . ^ a b Rosner W, Auchus RJ, Azziz R, Sluss PM, Raff H (February 2007). "Position statement: Utility, limitations, and pitfalls in measuring testosterone: an Endocrine Society position statement" .TACR3, GNRHR, GNRH1, TAC3, NR0B1, LHB, FSHB, KISS1R, LEP, LEPR, NR5A1, KISS1, PRL, CYP19A1, SLC29A3, POLD1, CYP17A1, CGB3, CSHL1, FGFR1, GHRH, SOX2, ANOS1, POLR3A, PROKR2, FGF8, PROP1, CHD7, PROK2, POLR3B, PNPLA6, NSMF, NDN, SEMA3A, RNF216, HS6ST1, FGF17, SRY, GJB2, AXL, CCDC141, TYMP, WDR11, UBA6-AS1, TFR2, SRA1, PWAR1, SEMA3E, GTF2IRD1, NTN1, HJV, SNORD116-1, SNORD115-1, CTDP1, PWRN1, AIP, BAZ1B, HERC2, MKRN3-AS1, HESX1, PTCH2, TP63, LZTR1, MKRN3, WT1, CLIP2, FEZF1, DNAL4, ZMPSTE24, A2ML1, RBM28, IL17RD, MAGEL2, HDAC8, CDH23, DCAF17, SUFU, SOX10, SPRY4, LAS1L, DHH, RRM2B, TBL2, GPR101, RAB3GAP2, FLRT3, NPAP1, KAT6B, PLXND1, RAB3GAP1, MRAS, CBX2, LHX4, SOS1, RNU4ATAC, SOX9, OTX2, POU1F1, ELN, POLG, PMM2, PDGFB, PCSK1, GLI2, GTF2I, SIX6, PTPN11, HFE, NRAS, HSD17B3, NF2, IPW, MEN1, MAP3K1, KRAS, LMNA, PTCH1, RAD51, RAF1, SOX3, SOS2, SNRPN, ANK1, SMARCB1, BMP2, BRAF, RRAS, BRD2, RIT1, CTNNB1, DCC, RFC2, REV3L, DMRT1, DUSP6, RASA2, LIMK1, AR, GH1, ESRRB, GK, MPZ, SERPINA4, VDR, SHBG, PMP22, GGN, NRP2, BECN1, DAZ1, PDE5A, CTLA4, CBLL2, NEUROG3, S1PR1, CPE, IGSF10, S100A4, TYRO3, AMH, NRP1, POMC, CD274, SCO2, FGF2, FGF3, MUL1, FGF9, FGF10, MSTN, TUBB3, PRKN, NT5E, NGF, IGF1, STAR, MC4R, ADH5
-
Primary Hypomagnesemia With Secondary Hypocalcemia
Orphanet
Etiology Mutations in the gene TRPM6 (9q21.13), encoding the transient receptor potential cation channel subfamily M, member 6, have been found to be responsible for this disease The pathophysiological hallmark of PHSH is the impaired intestinal absorption of magnesium (Mg) accompanied by renal Mg wasting as a result of a reabsorption defect in the distal convoluted tubule. ... Diagnostic methods Diagnosis relies on laboratory findings which reveal severely reduced serum Mg levels accompanied by hypocalcemia and barely detectable PTH levels. ... Renal defects may be detected after an intravenous Mg load test. The diagnosis is confirmed by genetic screening of TRPM6 . ... Management and treatment Management is mainly symptomatic and the standard treatment consists of the exclusive and lifelong administration of Mg. During manifestations, intravenous or intramuscular administrations are preferred, whereas maintenance therapy usually consists of an oral administration of high doses of Mg. However, because of gastrointestinal side effects, some patients require additional parenteral Mg. Prognosis Prognosis of PHSH depends on the rapidity of diagnosis.
-
Side Effects Of Bicalutamide
Wikipedia
4 months Interstitial pneumonitis Death Kawahara et al. (2009) 8 78 years Male 80 mg/day 8 months Interstitial pneumonitis Recovered Masago et al. (2011) 9 77 years Male ? 7 months Interstitial pneumonitis Death Song et al. (2014) 10 77 years Male >50 mg/day ~12 months Interstitial pneumonitis Death Molina Mancero et al. (2016) 11 79 years Male ? ... Interstitial pneumonitis Recovered Derichs et al. (2018) 14 86 years Male 150 mg/day 6 years Eosinophilic pneumonitis Recovered Umeojiako & James (2019) 15 75 years Male ? ... PMID 12603397 . S2CID 8639102 . ^ a b c d e f g h i j k l Wellington K, Keam SJ (2006). ... Testosterone (T), LH, E2 and SHBG levels increased on Bic, although only T changes on both doses and LH changes on Bic 100 mg were significantly different to controls (p<0.001).
-
Urethritis
Wikipedia
Non-gonococcal urethritis (caused by Chlamydia trachomatis ) : The CDC recommends administering an oral single dose of azithromycin 1g or a 7-day course of doxycycline 100 mg orally twice daily.' [6] Alternative treatments can also be used when the above options are not available: [6] Erythromycin base 500 mg orally four times daily for 7 days Erythromycin ethylsuccinate 800 mg orally four times daily for 7 days Levofloxacin 500 mg orally once daily for 7 days Ofloxacin 300 mg orally twice daily for 7 days Treatment for both gonococcal and non-gonococcal urethritis is suggested to be given under direct observation in a clinic or healthcare facility in order to maximize compliance and effectiveness. ... Additionally, recurrent urethritis is defined as urethritis reappearing within 6 weeks after a previous episode of non-gonococcal urethritis. [22] If recurrent symptoms are supported by microscopic evidence of urethritis, then re-treatment is appropriate. [4] The following treatment recommendations are limited and based on clinical experience, expert opinions and guidelines for recurrent or persistent non-gonococcal urethritis : [4] If doxycycline was prescribed as initial therapy, give azithromycin 500 mg or 1 gram for the first day, then give azithromycin 250 mg once daily for 4 days plus metronidazole 400 – 500 mg twice daily for 5 days If azithromycin was prescribed as initial therapy, then give doxycycline 100 mg twice daily for 7 days plus metronidazole 400 – 500 mg twice daily for 5 – 7 days Moxifloxacin 400 mg orally once daily for 7 – 14 days can be given with use of caution, if macrolide-resistant M. genitalium infection is demonstrated [4] Appropriate treatment for these individuals may require further referral to a urologist if symptoms persist after initial treatment. [6] Epidemiology [ edit ] Urethritis is one of the most common sexually transmitted infections found in men. ... Sexually Transmitted Diseases . 40 (3): 271–4. doi : 10.1097/OLQ.0b013e31827c9e42 . PMID 23407472 . ^ a b c d Moi H, Blee K, Horner PJ (July 2015). "Management of non-gonococcal urethritis" . ... Retrieved 4 August 2020 . ^ a b c d e "Diseases Characterized by Urethritis and Cervicitis - 2015 STD Treatment Guidelines" . www.cdc.gov . Retrieved 2017-12-08 . ^ Territo H, Ashurst JV (2020). "Nongonococcal Urethritis (NGU)" . ... PMC 1046272 . PMID 6365237 . ^ a b c d e f g h Young A, Wray AA (2020). "Urethritis" .
-
Salicylate Poisoning
Wikipedia
This phase may begin 4–6 hours after ingestion in a young infant [10] or 24 hours or more after ingestion in an adolescent or adult. [9] Diagnosis [ edit ] The acutely toxic dose of aspirin is generally considered greater than 150 mg per kg of body mass. [11] Moderate toxicity occurs at doses up to 300 mg/kg, severe toxicity occurs between 300 and 500 mg/kg, and a potentially lethal dose is greater than 500 mg/kg. [12] Chronic toxicity may occur following doses of 100 mg/kg per day for two or more days. [12] Monitoring of biochemical parameters such as electrolytes and solutes, liver and kidney function, urinalysis , and complete blood count is undertaken along with frequent checking of salicylate and blood sugar levels. ... Plasma salicylate levels generally range from 30–100 mg/l (3–10 mg/dl) after usual therapeutic doses, 50–300 mg/l in patients taking high doses, and 700–1400 mg/l following acute overdose. [13] Patients may undergo repeated testing until their peak plasma salicylate level can be estimated. [14] Optimally, plasma levels should be assessed four hours after ingestion and then every two hours after that to allow calculation of the maximum level, which can then be used as a guide to the degree of toxicity expected. [15] Patients may also be treated according to their individual symptoms. ... Examples of severe poisoning include people with high salicylate blood levels: 7.25 mmol/l (100 mg/dl) in acute ingestions or 40 mg/dl in chronic ingestions, [18] significant neurotoxicity (agitation, coma, convulsions), kidney failure , pulmonary edema, or cardiovascular instability. [14] Hemodialysis also has the advantage of restoring electrolyte and acid-base abnormalities while removing salicylate. [19] Salicylic acid has a small size (low molecular mass), has a low volume of distribution (is more water soluble), has low tissue binding and is largely free (and not protein bound) at toxic levels in the body; all of which make it easily removable from the body by hemodialysis. [8] Indication for dialysis: Salicylate level higher than 90 mg/dL [8] Severe acid base imbalance Severe cardiac toxicity Acute respiratory distress syndrome [8] Cerebral involvement/ neurological signs and symptoms Rising serum salicylate level despite alkalinization/multidose activated charcoal, or people in which standard approaches to treatment ave failed [8] Unable to tolerate fluids with fluid overload Epidemiology [ edit ] Acute salicylate toxicity usually occurs after an intentional ingestion by younger adults, often with a history of psychiatric disease or previous overdose, whereas chronic toxicity usually occurs in older adults who experience inadvertent overdose while ingesting salicylates therapeutically over longer periods of time. [8] During the latter part of the 20th century, the number of poisonings from salicylates declined, mainly because of the increased popularity of other over-the-counter analgesics such as paracetamol (acetaminophen). Fifty-two deaths involving single-ingredient aspirin were reported in the United States in 2000; however, in all but three of these cases, the reason for the ingestion of lethal doses was intentional—predominantly suicidal. [20] History [ edit ] Aspirin poisoning has controversially been cited as a possible cause of the high mortality rate during the 1918 flu pandemic , which killed 50 to 100 million people. [21] See also [ edit ] NSAID hypersensitivity reactions Reye syndrome Salicylate sensitivity References [ edit ] ^ a b c d e f g h i j k l m n o p q r O'Malley, GF (May 2007). ... PMID 3591255 . S2CID 21769646 . ^ a b c d e f g h i j k l m n o p q r s t u v w x Palmer, Biff F.; Clegg, Deborah J. (25 June 2020).
-
Hypoascorbemia
OMIM
Seven healthy volunteers were hospitalized for 4 to 6 months and consumed a diet containing less than 5 mg of vitamin C daily. Steady-state plasma and tissue concentrations were determined at 7 daily doses of vitamin C from 30 to 2,500 mg. ... The steep portion of the curve occurred between the 30- and 100-mg daily dose, the then-current recommended daily allowance (RDA) of 60 mg was on the lower third of the curve, the first dose beyond the sigmoid portion of the curve was 200 mg daily, and complete plasma saturation occurred at 1,000 mg daily. No vitamin C was excreted in the urine of 6 of 7 volunteers until the 100-mg dose was reached. At single doses of 500 mg and higher, bioavailability declined and the absorbed amount was excreted. Oxalate and urate excretion were elevated at 1,000 mg of vitamin C daily compared to lower doses. ... Safe doses of vitamin C are less than 1,000 mg daily, and vitamin C daily doses above 400 mg have no evident value.
-
Hyperosmolar Hyperglycemic State
Wikipedia
A relative insulin deficiency leads to a serum glucose that is usually higher than 33 mmol/L (600 mg/dL), and a resulting serum osmolarity that is greater than 320 mOsm. ... Diagnosis [ edit ] Criteria [ edit ] According to the American Diabetes Association , diagnostic features include: [7] [8] Plasma glucose level >30 mmol/L (>600 mg/dL) Serum osmolality >320 mOsm/kg Profound dehydration, up to an average of 9L (and therefore substantial thirst ( polydipsia )) Serum pH >7.30 [8] Bicarbonate >15 mEq/L Small ketonuria (~+ on dipstick) and absent-to-low ketonemia (<3 mmol/L) Some alteration in consciousness BUN > 30 mg/dL (increased) [5] Creatinine > 1.5 mg/dL (increased) [5] Imaging [ edit ] Cranial imaging is not used for diagnosis of this condition. ... Retrieved 6 July 2012 . ^ a b c d e f g h i Stoner, GD (1 May 2005). "Hyperosmolar hyperglycemic state". American Family Physician . 71 (9): 1723–30. PMID 15887451 . ^ a b c d e f g h i j k l m Frank, LA; Solomon, A (2 September 2016). ... PMC 4207202 . PMID 25342831 . ^ a b c d e f g h i j k l m n o p q r s t u v w x Henry, McMichael (2016).