Load FindZebra Summary
Disclaimer:
FindZebra Search conducts a search using our specialized medical search engine.
FindZebra Summary uses the text completions API
(subject to OpenAI’s API data usage policies)
to summarize and reason about the search results.
The search is conducted in publicly available information on the Internet that we present “as is”.
You should be aware that FindZebra is not supplying any of the content in the search results.
FindZebra Summary is loading...
-
Ocular Myasthenia
Wikipedia
MG may be limited to the muscles of the eye (ocular MG), leading to abrupt onset of weakness/fatigability of the eyelids or eye movement. MG may also involve other muscle groups ( generalized MG ). ... Diagnosis [ edit ] The variable course of MG may make the diagnosis difficult. ... Treatment [ edit ] The prognosis tends to be good for patients with MG. It is often best not to treat mild cases of MG. ... The symptoms of ocular MG can also be addressed by non-medicinal means.
-
Androgen Deficiency
Wikipedia
The Food and Drug Administration (FDA) stated in 2015 that neither the benefits nor the safety of testosterone have been established for low testosterone levels due to aging . [6] The FDA has required that testosterone pharmaceutical labels include warning information about the possibility of an increased risk of heart attacks and stroke. [6] v t e Androgen replacement therapy formulations and dosages used in men Route Medication Major brand names Form Dosage Oral Testosterone a – Tablet 400–800 mg/day (in divided doses) Testosterone undecanoate Andriol, Jatenzo Capsule 40–80 mg/2–4x day (with meals) Methyltestosterone b Android, Metandren, Testred Tablet 10–50 mg/day Fluoxymesterone b Halotestin, Ora-Testryl, Ultandren Tablet 5–20 mg/day Metandienone b Dianabol Tablet 5–15 mg/day Mesterolone b Proviron Tablet 25–150 mg/day Buccal Testosterone Striant Tablet 30 mg 2x/day Methyltestosterone b Metandren, Oreton Methyl Tablet 5–25 mg/day Sublingual Testosterone b Testoral Tablet 5–10 mg 1–4x/day Methyltestosterone b Metandren, Oreton Methyl Tablet 10–30 mg/day Intranasal Testosterone Natesto Nasal spray 11 mg 3x/day Transdermal Testosterone AndroGel, Testim, TestoGel Gel 25–125 mg/day Androderm, AndroPatch, TestoPatch Non-scrotal patch 2.5–15 mg/day Testoderm Scrotal patch 4–6 mg/day Axiron Axillary solution 30–120 mg/day Androstanolone ( DHT ) Andractim Gel 100–250 mg/day Rectal Testosterone Rektandron, Testosteron b Suppository 40 mg 2–3x/day Injection ( IM or SC ) Testosterone Andronaq, Sterotate, Virosterone Aqueous suspension 10–50 mg 2–3x/week Testosterone propionate b Testoviron Oil solution 10–50 mg 2–3x/week Testosterone enanthate Delatestryl Oil solution 50–250 mg 1x/1–4 weeks Xyosted Auto-injector 50–100 mg 1x/week Testosterone cypionate Depo-Testosterone Oil solution 50–250 mg 1x/1–4 weeks Testosterone isobutyrate Agovirin Depot Aqueous suspension 50–100 mg 1x/1–2 weeks Testosterone phenylacetate b Perandren, Androject Oil solution 50–200 mg 1x/3–5 weeks Mixed testosterone esters Sustanon 100, Sustanon 250 Oil solution 50–250 mg 1x/2–4 weeks Testosterone undecanoate Aveed, Nebido Oil solution 750–1,000 mg 1x/10–14 weeks Testosterone buciclate a – Aqueous suspension 600–1,000 mg 1x/12–20 weeks Implant Testosterone Testopel Pellet 150–1,200 mg/3–6 months Notes: Men produce about 3 to 11 mg testosterone per day (mean 7 mg/day in young men).
-
Genetic Primary Hypomagnesemia
Orphanet
A rare mineral absorption and transport disorder characterized by a selective defect in renal or intestinal magnesium (Mg) absorption, resulting in a low Mg concentration in the blood. ... Diagnosis is also established by simultaneous evaluation of serum Mg and urinary Mg excretion. Presence of hypomagnesemia with adapted urinary Mg excretion (<1mmol/24h or fractional excretion (FE) < 1%) indicates an extra renal origin. Elevated fecal Mg levels indicate an intestinal defect. In contrast, hypomagnesemia with increased urinary Mg excretion (> 2 mmol/24h or FE >2%) indicates a renal origin. ... Management and treatment Treatment of FPH involves substitution with oral Mg. In cases of intolerance, patients may be treated with intramuscular Mg sulfate.
-
Familial Primary Hypomagnesemia With Normocalciuria And Normocalcemia
Orphanet
A form of familial primary hypomagnesemia (FPH), characterized by low serum magnesium (Mg) values but inappropriate normal urinary Mg values (i.e. renal hypomagnesemia). ... As a consequence, the renal EGF receptor (EGFR) is inadequately stimulated, resulting in insufficient activation of the epithelial Mg channel TRPM6 and thereby Mg loss. Thus, a renal Mg reabsorption defect is observed due to the inability of the kidney to reduce urinary Mg excretion under low serum Mg conditions. Diagnostic methods Diagnosis relies on laboratory findings revealing severely lowered serum Mg values in the absence of other electrolyte disturbances, normocalcemia, low to normal urinary calcium (Ca) values and normal urinary Mg values. ... Management and treatment Treatment of FPHNN is mainly symptomatic and includes the Mg substitution therapy. Prognosis Severity of the disease is variable.
-
Juvenile Myasthenia Gravis
Orphanet
Juvenile myasthenia gravis (MG; see this term) is a rare form of MG, an autoimmune disorder of the neuromuscular junction resulting in ocular manifestations or generalized weakness, with onset before 18 years of age. Epidemiology The exact prevalence and incidence of juvenile MG are not known. Estimated incidence has been reported at 1/1,000,000 to 1/200,000. ... The proportion of patients having only ocular symptoms is higher than in adult MG, particularly in the prepubertal group in which half of cases are purely ocular. ... Thymoma (see this term) development is rare in juvenile MG. Etiology The exact pathogenesis is not known but MG is related to circulating antibodies to various muscle receptors, including, in most of patients, acetylcholine receptor (AChR) and, rarely, muscle-specific receptor tyrosine kinase (MuSK). ... In the prepubertal form, there is a high rate of the MG form with no antibodies detectable (30-50%).
-
Meier-Gorlin Syndrome
GARD
Meier-Gorlin syndrome (MGS) is a very rare inherited condition characterized by very small ears and ear canals, short stature, and absent or very small kneecaps (patellae). ... Females with MGS may have underdeveloped breasts. ... Most forms of MGS are inherited in an autosomal recessive pattern. The form caused by the GMNN gene is inherited in an autosomal dominant pattern. MGS is diagnosed based on the clinical signs and symptoms. ... Most people with this syndrome have normal lifespans. The exact prevalence of MGS has not been determined, but is estimated to be less than 1-9/1,000,000.ORC1, CDT1, GMNN, ORC6, CDC6, ORC4, CDC45, BMP5, DRD2, SLC6A3, CYP2D6, MAPK1, MYH9, TLR4, MTOR, RBP4, MCM5, PSEN1, COMT, PTH, MAPK3, SOD1, RELA, PRKCA, PRKACG, RGS2, ATXN2, SLC18A2, VEGFA, SYT1, TGFB1, TNF, PIK3CG, PDPN, POSTN, CHEK2, PLCB1, SIRT1, ORC3, DISC1, CLEC7A, GORASP1, WNK1, PLA2G4A, ACTG1, PIK3CA, HTR2A, ASPH, BRCA2, BSG, CD2, COL1A1, CRP, CCN2, DRD3, EPHB2, FANCD2, FASN, FOXM1, GNAS, GRIK3, IL6, SERPINE1, IL10, INSR, ITPR1, LEP, CYP4F3, LY6E, LYZ, MAOB, MCM2, ATXN3, NOS2, ACTB, APOE, PAEP, ACHE
-
Primary Hypomagnesemia With Secondary Hypocalcemia
Orphanet
Etiology Mutations in the gene TRPM6 (9q21.13), encoding the transient receptor potential cation channel subfamily M, member 6, have been found to be responsible for this disease The pathophysiological hallmark of PHSH is the impaired intestinal absorption of magnesium (Mg) accompanied by renal Mg wasting as a result of a reabsorption defect in the distal convoluted tubule. ... Diagnostic methods Diagnosis relies on laboratory findings which reveal severely reduced serum Mg levels accompanied by hypocalcemia and barely detectable PTH levels. ... Renal defects may be detected after an intravenous Mg load test. The diagnosis is confirmed by genetic screening of TRPM6 . ... Management and treatment Management is mainly symptomatic and the standard treatment consists of the exclusive and lifelong administration of Mg. During manifestations, intravenous or intramuscular administrations are preferred, whereas maintenance therapy usually consists of an oral administration of high doses of Mg. However, because of gastrointestinal side effects, some patients require additional parenteral Mg. Prognosis Prognosis of PHSH depends on the rapidity of diagnosis.
-
Myasthenia Gravis With Thymus Hyperplasia
OMIM
Myasthenia gravis (MG; see 254200) is an autoimmune disease of the neuromuscular junction that is often found in association with other autoimmune disorders. Association studies using case-control designs, i.e., comparisons of unrelated patients and control subjects, had demonstrated an increased frequency of the extended HLA haplotype A1-B8-DR3 (8.1) in Caucasian MG patients with thymus hyperplasia, in women, and in patients with an early onset of disease (Fritze et al., 1974; Vieira et al., 1993; Machens et al., 1999). To reevaluate the association of HLA with MG in 656 patients with generalized disease, and to test linkage of HLA to MG with thymus hyperplasia, Giraud et al. (2001) studied transmission of parental alleles to MG offspring with thymus hyperplasia in simplex (single-case) families using the transmission/disequilibrium test (TDT) as a test of linkage. Their results indicated linkage of HLA to MG with thymus hyperplasia, defining a locus on chromosome 6p21.3 that they designated MYAS1. They found that DR3 and DR7, or closely linked genes, had opposing effects on MG phenotypes. MG with thymus hyperplasia was positively associated with DR3 and negatively associated with DR7, based on both case-control comparisons and TDT.CFB, HLA-B, MUSK, HLA-DPB1, POMC, FAS, HLA-DRB1, HLA-DQA1, PTPN22, HLA-A, TNIP1, C2, IL10, NFKBIL1, ZNRD1, MUC21, SFTA2, HCG9, PSORS1C1, CTLA4, NOTCH4, MUCL3, CYP21A2, RBM45, BTNL2, GPSM3, MSH5, TSBP1, MICB, LRP4, TRIM31, POU5F1, HLA-DQA2, RNF39, GABBR1, VARS2, LINC00243, ABCF1, IFNG, MSH5-SAPCD1, HCG17, TNFRSF11A, TCF19, BCHE, ATP6V1G2, STK19, TNF, HCG18, GPANK1, SEMA5A, TTN, TSBP1-AS1, RBBP8, ACHE, PRRC2A, CXCL13, IL17A, IL2RA, IL6, ISG20, EIF3K, IL2, FOXP3, AIRE, IL4, CHRNA1, TRBV20OR9-2, HLA-DQB1, THM, LTA, IL1B, CD274, IL22, PDCD1, IL21, TLR9, CHRNE, IL1A, MIR150, AQP4, HT, TGFB1, CDR3, ECD, MIR21, DOK7, TLR4, CD40, TLR3, MBP, CCL21, CHRNA4, TAP2, CXCR4, IGHG3, IFNB1, MAPK1, PDLIM7, IL18R1, IL15, EBI3, IL4R, SMN1, CXCL10, IFNA13, TLR7, TNFRSF13C, FGFR3, MIR146A, ESR1, TSLP, CD40LG, GNAO1, DNMT3B, HLA-DQB2, CAV3, IL23A, MIR125A, ADRB2, IFNA1, IFN1@, HMGB1, C4orf3, DIPK1A, SOCS3, LGI1, MSC, SCO2, CD83, GRAP2, MIR145, MIRLET7C, NTN1, MIR155, PPP6R2, MIR143, MBTPS1, MIR15B, SCFV, LOC102723407, IFNG-AS1, LINC-ROR, C4B_2, C20orf181, TEC, CCR2, DDX39B, MIR653, MIR323B, MIR19B1, MIR338, AIMP2, FOSL1, MIR320A, USO1, TNFRSF25, MIR30E, MALAT1, TNFSF10, DDX39A, RMDN2, MYAS1, CCAR2, RNF19A, CNTNAP2, HIF3A, ROBO3, POLDIP2, IFIH1, IGAN1, B3GAT1, DPYSL5, PART1, RETN, IGHV3-52, TWNK, MSL2, KRT20, ICOS, SLC25A37, VAV1, TMEM109, PPP1R15A, PRSS16, UNC5A, CLEC4C, CDIPT, NXF1, MZB1, TRIM9, AHSA1, IL17F, IL33, TNFSF13B, DDX58, CCR9, FHDC1, LILRB1, FAM136A, SLC7A9, TBC1D9, ICOSLG, SEC14L2, VIP, RAF1, UTRN, CNTFR, CRK, MAPK14, CSF1, CCN2, CTSV, CTSS, CYP3A5, CD55, BRINP1, DCC, DNMT3A, ATN1, TYMP, CTTN, ERBB4, ESR2, FCGR2A, FLNB, FOS, FOSB, CXCR3, GRIA2, GRM2, CXCL1, GZMB, HLA-C, HLA-DOA, HLA-DPA1, HLA-DRB3, CR2, CCR7, HNMT, CCR5, ADCYAP1, AGER, ALB, APOE, APRT, ABCC6, BCL2, TNFRSF17, BDNF, C4A, C4B, C5, CA3, CACNA1S, CALCA, CALCR, CAMP, CASP1, CASP3, CD19, MS4A1, CD28, CD86, CD69, CDS1, CHRNB1, CHRND, CLC, CCR4, HLA-G, HOXD13, TYMS, NTRK1, P2RX7, PAM, PAX7, ABCB1, PMP22, MAPK3, PTPRC, PLAAT4, RELB, S100A8, S100A11, S100B, SCN4A, SCO1, CCL5, CCL17, CCL22, CXCL12, SGCA, SLAMF1, SMN2, SPP1, STAT3, STAT4, TAP1, THBS1, TNFAIP3, TNFSF4, TNFRSF4, OSM, NCAM1, HSPA5, MYOG, IRF8, IFNA2, IFNA17, IFNGR1, IGF1, IGF1R, IGFBP1, IGL, IL1RN, IL2RB, IL7R, IL9, IL12B, IL12RB2, INS, IRF4, ITGAX, JUN, JUNB, JUND, KIT, KRT5, LDLR, LGALS1, LGALS8, LIF, MEFV, MFAP1, MMP10, LOC102724971
-
Side Effects Of Bicalutamide
Wikipedia
4 months Interstitial pneumonitis Death Kawahara et al. (2009) 8 78 years Male 80 mg/day 8 months Interstitial pneumonitis Recovered Masago et al. (2011) 9 77 years Male ? 7 months Interstitial pneumonitis Death Song et al. (2014) 10 77 years Male >50 mg/day ~12 months Interstitial pneumonitis Death Molina Mancero et al. (2016) 11 79 years Male ? ... Interstitial pneumonitis Recovered Derichs et al. (2018) 14 86 years Male 150 mg/day 6 years Eosinophilic pneumonitis Recovered Umeojiako & James (2019) 15 75 years Male ? ... S2CID 207947815 . ^ Tyrrell CJ, Denis L, Newling D, Soloway M, Channer K, Cockshott ID (1998). "Casodex 10-200 mg daily, used as monotherapy for the treatment of patients with advanced prostate cancer. ... Testosterone (T), LH, E2 and SHBG levels increased on Bic, although only T changes on both doses and LH changes on Bic 100 mg were significantly different to controls (p<0.001).
-
Hypoascorbemia
OMIM
Seven healthy volunteers were hospitalized for 4 to 6 months and consumed a diet containing less than 5 mg of vitamin C daily. Steady-state plasma and tissue concentrations were determined at 7 daily doses of vitamin C from 30 to 2,500 mg. ... The steep portion of the curve occurred between the 30- and 100-mg daily dose, the then-current recommended daily allowance (RDA) of 60 mg was on the lower third of the curve, the first dose beyond the sigmoid portion of the curve was 200 mg daily, and complete plasma saturation occurred at 1,000 mg daily. No vitamin C was excreted in the urine of 6 of 7 volunteers until the 100-mg dose was reached. At single doses of 500 mg and higher, bioavailability declined and the absorbed amount was excreted. Oxalate and urate excretion were elevated at 1,000 mg of vitamin C daily compared to lower doses. ... Safe doses of vitamin C are less than 1,000 mg daily, and vitamin C daily doses above 400 mg have no evident value.
-
Hypogonadism
Wikipedia
Clomifene at much higher doses is used to induce ovulation and has significant adverse effects in such a setting. v t e Androgen replacement therapy formulations and dosages used in men Route Medication Major brand names Form Dosage Oral Testosterone a – Tablet 400–800 mg/day (in divided doses) Testosterone undecanoate Andriol, Jatenzo Capsule 40–80 mg/2–4x day (with meals) Methyltestosterone b Android, Metandren, Testred Tablet 10–50 mg/day Fluoxymesterone b Halotestin, Ora-Testryl, Ultandren Tablet 5–20 mg/day Metandienone b Dianabol Tablet 5–15 mg/day Mesterolone b Proviron Tablet 25–150 mg/day Buccal Testosterone Striant Tablet 30 mg 2x/day Methyltestosterone b Metandren, Oreton Methyl Tablet 5–25 mg/day Sublingual Testosterone b Testoral Tablet 5–10 mg 1–4x/day Methyltestosterone b Metandren, Oreton Methyl Tablet 10–30 mg/day Intranasal Testosterone Natesto Nasal spray 11 mg 3x/day Transdermal Testosterone AndroGel, Testim, TestoGel Gel 25–125 mg/day Androderm, AndroPatch, TestoPatch Non-scrotal patch 2.5–15 mg/day Testoderm Scrotal patch 4–6 mg/day Axiron Axillary solution 30–120 mg/day Androstanolone ( DHT ) Andractim Gel 100–250 mg/day Rectal Testosterone Rektandron, Testosteron b Suppository 40 mg 2–3x/day Injection ( IM or SC ) Testosterone Andronaq, Sterotate, Virosterone Aqueous suspension 10–50 mg 2–3x/week Testosterone propionate b Testoviron Oil solution 10–50 mg 2–3x/week Testosterone enanthate Delatestryl Oil solution 50–250 mg 1x/1–4 weeks Xyosted Auto-injector 50–100 mg 1x/week Testosterone cypionate Depo-Testosterone Oil solution 50–250 mg 1x/1–4 weeks Testosterone isobutyrate Agovirin Depot Aqueous suspension 50–100 mg 1x/1–2 weeks Testosterone phenylacetate b Perandren, Androject Oil solution 50–200 mg 1x/3–5 weeks Mixed testosterone esters Sustanon 100, Sustanon 250 Oil solution 50–250 mg 1x/2–4 weeks Testosterone undecanoate Aveed, Nebido Oil solution 750–1,000 mg 1x/10–14 weeks Testosterone buciclate a – Aqueous suspension 600–1,000 mg 1x/12–20 weeks Implant Testosterone Testopel Pellet 150–1,200 mg/3–6 months Notes: Men produce about 3 to 11 mg testosterone per day (mean 7 mg/day in young men).TACR3, GNRHR, GNRH1, TAC3, NR0B1, LHB, FSHB, KISS1R, LEP, LEPR, NR5A1, KISS1, PRL, CYP19A1, SLC29A3, POLD1, CYP17A1, CGB3, CSHL1, FGFR1, GHRH, SOX2, ANOS1, POLR3A, PROKR2, FGF8, PROP1, CHD7, PROK2, POLR3B, PNPLA6, NSMF, NDN, SEMA3A, RNF216, HS6ST1, FGF17, SRY, GJB2, AXL, CCDC141, TYMP, WDR11, UBA6-AS1, TFR2, SRA1, PWAR1, SEMA3E, GTF2IRD1, NTN1, HJV, SNORD116-1, SNORD115-1, CTDP1, PWRN1, AIP, BAZ1B, HERC2, MKRN3-AS1, HESX1, PTCH2, TP63, LZTR1, MKRN3, WT1, CLIP2, FEZF1, DNAL4, ZMPSTE24, A2ML1, RBM28, IL17RD, MAGEL2, HDAC8, CDH23, DCAF17, SUFU, SOX10, SPRY4, LAS1L, DHH, RRM2B, TBL2, GPR101, RAB3GAP2, FLRT3, NPAP1, KAT6B, PLXND1, RAB3GAP1, MRAS, CBX2, LHX4, SOS1, RNU4ATAC, SOX9, OTX2, POU1F1, ELN, POLG, PMM2, PDGFB, PCSK1, GLI2, GTF2I, SIX6, PTPN11, HFE, NRAS, HSD17B3, NF2, IPW, MEN1, MAP3K1, KRAS, LMNA, PTCH1, RAD51, RAF1, SOX3, SOS2, SNRPN, ANK1, SMARCB1, BMP2, BRAF, RRAS, BRD2, RIT1, CTNNB1, DCC, RFC2, REV3L, DMRT1, DUSP6, RASA2, LIMK1, AR, GH1, ESRRB, GK, MPZ, SERPINA4, VDR, SHBG, PMP22, GGN, NRP2, BECN1, DAZ1, PDE5A, CTLA4, CBLL2, NEUROG3, S1PR1, CPE, IGSF10, S100A4, TYRO3, AMH, NRP1, POMC, CD274, SCO2, FGF2, FGF3, MUL1, FGF9, FGF10, MSTN, TUBB3, PRKN, NT5E, NGF, IGF1, STAR, MC4R, ADH5
-
Morning Glory Syndrome
GARD
Morning glory syndrome (MGS) is a birth (congenital) defect of the nerve of the eye (optic nerve) that resembles a flower known as "morning glory". ... Symptoms include very poor vision in the affected eye with poor visual acuity . MGS may occur by itself or along with other eye abnormalities, such as crossed eyes (strabismus) or lazy eye (amblyopia), or other non-ocular problems like brain disorders. Typically, individuals with non-ocular findings also have a wide head, depressed nasal bridge, and mid upper lip defect or cleft. MGS seems to be caused from failure of the optic nerve to completely form when the baby is developing. The most severe complication is retinal detachment , and can occur in about 26–38% of people with MGS. The MGS is sometimes misdiagnosed as an optic nerve coloboma .
-
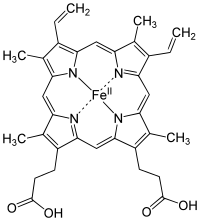
Iron Deficiency
Wikipedia
Signs and symptoms in children [ edit ] pale skin fatigue slowed growth and development poor appetite behavioral problems abnormal rapid breathing frequent infection Iron requirements in young children to teenagers [ edit ] Age group Recommended amount of iron a day [7] 7 – 12 months 11 mg 1 – 3 years 7 mg 4 – 8 years 10 mg 9 – 13 years 8 mg 14 – 18 years, girls 15 mg 14 – 18 years, boys 11 mg Causes [ edit ] blood loss ( hemoglobin contains iron) donation excessive menstrual bleeding non-menstrual bleeding bleeding from the gastrointestinal tract ( ulcers , hemorrhoids , ulcerative colitis , stomach or colon cancer , etc.) rarely, laryngological bleeding or from the respiratory tract inadequate intake (see below) substances (in diet or drugs) interfering with iron absorption Fluoroquinolone antibiotics [8] malabsorption syndromes inflammation where it is adaptive to limit bacterial growth in infection, but is also present in many other chronic diseases such as Inflammatory bowel disease and rheumatoid arthritis parasitic infection Though genetic defects causing iron deficiency have been studied in rodents, there are no known genetic disorders of human iron metabolism that directly cause iron deficiency. ... Additionally, athletes in sports that emphasize weight loss (e.g. ballet , gymnastics , marathon running , and wrestling ) as well as sports that emphasize high- carbohydrate , low- fat diets, may be at an increased risk for iron deficiency. [9] [10] Inadequate intake [ edit ] A U.S. federal survey of food consumption determined that for women and men over the age of 19, average iron consumption from foods and beverages was 13.1 and 18.0 mg/day, respectively. For women, 16% in the age range 14–50 years consumed less than the Estimated Average Requirement (EAR), for men ages 19 and up, fewer than 3%. [11] Consumption data were updated in a 2014 U.S. government survey and reported that for men and women ages 20 and older the average iron intakes were, respectively, 16.6 and 12.6 mg/day. [12] People in the U.S. usually obtain adequate amounts of iron from their diets. ... Reflecting this link between iron bioavailability and bacterial growth, the taking of oral iron supplements in excess of 200 mg/day causes a relative overabundance of iron that can alter the types of bacteria that are present within the gut. ... Recent research suggests the replacement dose of iron, at least in the elderly with iron deficiency, may be as little as 15 mg per day of elemental iron. [21] Food sources [ edit ] Mild iron deficiency can be prevented or corrected by eating iron-rich foods and by cooking in an iron skillet. ... Arbitrarily, the guideline is set at 18 mg, which is the USDA Recommended Dietary Allowance for women aged between 19 and 50. [29] Abstract: richest foods in heme iron Food Serving size Iron % guideline clam [a] 100g 28 mg 155% pork liver 100g 18 mg 100% lamb kidney 100g 12 mg 69% cooked oyster 100g 12 mg 67% cuttlefish 100g 11 mg 60% lamb liver 100g 10 mg 57% octopus 100g 9.5 mg 53% mussel 100g 6.7 mg 37% beef liver 100g 6.5 mg 36% beef heart 100g 6.4 mg 35% Abstract: richest foods in non-heme iron Food Serving size Iron % guideline raw yellow beans 100g 7 mg 35% spirulina 15g 4.3 mg 24% falafel 140g 4.8 mg 24% soybean kernels 125ml=1/2cup 4.6 mg 23% spinach 125g 4.4 mg 22% lentil 125ml=1/2cup 3.5 mg 17.5% treacle (CSR Australia) 20ml=1Tbsp 3.4 mg 17% molasses (Bluelabel Australia) 20ml=1Tbsp 1.8 mg 9% candied ginger root 15g~3p 1.7 mg 8.5% toasted sesame seeds 10g 1.4 mg 7% cocoa (dry powder) 5g~1Tbsp .8 mg 4% Food recommendations for children [ edit ] Children at 6 months should start having solid food that contains enough iron, which could be found in both heme and non-heme iron [33] Heme iron : Red meat (for example, beef, pork, lamb, goat, or venison) Fatty fish Poultry (for example, chicken or turkey) Eggs Non-heme iron : Iron-fortified infant cereals Tofu Beans and lentils Dark green leafy vegetables Iron deficiency can have serious health consequences that diet may not be able to quickly correct; hence, an iron supplement is often necessary if the iron deficiency has become symptomatic.EPO, TMPRSS6, SLC11A2, HFE, TFRC, HAMP, CRP, FGF23, HBA2, CHMP2B, DMRT1, HIF1A, IL1B, SLC40A1, EPAS1, HEPH, PMCH, BDNF, HBA1, CP, AIF1, RET, IREB2, IL6, SLC39A1, ATF4, PARP3, RN7SL263P, HMOX1, TNF, ALB, IDUA, FECH, LCN2, ACAD8, FXN, ERFE, BDH2, CYBRD1, RLS1, TFR2, TDGF1P3, ACO1, RPP14, ZFP36, SUB1, PPARGC1A, AHSA1, AIMP2, KHSRP, STK16, AKR1A1, CDKL1, BCAP31, CDK2AP2, GRAP2, DNALI1, HDAC3, EIF2S2, SLC39A7, NOL3, GOSR1, XPR1, MLLT10, PSIP1, GSTO1, ABCG2, ABO, SETD2, SIRT2, SLC36A1, ZGPAT, COX19, SLC46A1, CYGB, OLIG1, HJV, IL27, XYLT2, COPD, SLC39A5, CYCSP51, NUP43, H3P8, H3P24, HHIP, NLN, JMJD6, UBE2D1, CRTC1, CDK20, RNF19A, POLDIP2, SIGLEC7, LAMTOR2, TMED5, SLC39A10, SLC25A37, NCKIPSD, SF3B6, NANS, AHI1, SMARCAD1, VHL, SST, TYS, CUX1, DNAH8, EBF1, EDN1, EIF2S1, EIF2S3, ESR1, ETV3, G6PD, GATA1, GPI, HCLS1, HP, PRMT1, IFNG, IGF1, DAPK3, CTSL, TTR, MAPK14, ACP5, APEX1, ARG1, ARSA, ATP4A, BACH1, BSG, CAT, CCK, CDKN2A, CENPF, CLN3, SLC31A1, CRK, CRYGD, IL1A, IL2RB, CXCL8, SMAD1, RPL29, S100A9, TSPAN31, SAT1, SLC2A1, SLC11A1, SOD1, ST13, STAT3, STAT5A, STAT5B, CNTN2, TCF3, TNFRSF1B, TST, REN, PRPH2, PVALB, PDE7A, SMAD7, MMP9, MPO, NGF, NUCB2, REG3A, CFP, PTH, PPARG, MAPK1, PRNP, RELN, PSMC6, PSMD10, H3P30
-
Hypomagnesemia 6, Renal
OMIM
In both families, the index patients had severely lowered serum Mg(2+) levels in the absence of other electrolyte disturbances, and affected individuals showed an inappropriately normal urinary Mg(2+) excretion, demonstrating a defect in tubular reabsorption. Stuiver et al. (2011) noted that although serum Mg(2+) levels in both probands and their affected parents were in the same decreased range, there was remarkable variability in the age of clinical (symptomatic) onset of disease: in the Dutch proband, onset of clinical disease was at 2 years of age, whereas in her father it was at 15 years of age, and in the Czech family, the affected mother was asymptomatic. ... INHERITANCE - Autosomal dominant GENITOURINARY Kidneys - Defect in renal tubular reabsorption of Mg(2+) MUSCLE, SOFT TISSUES - Muscle weakness NEUROLOGIC Central Nervous System - Headaches - Vertigo LABORATORY ABNORMALITIES - Low levels of serum Mg(2+) in the absence of other electrolyte disturbances MISCELLANEOUS - Variable presentation of clinical features - Some people with a CNNM2 mutation are asymptomatic MOLECULAR BASIS - Caused by mutation in the cyclin M2 gene (CNNM2, 607803.0001 ) ▲ Close
-
Hypoglycemia
Wikipedia
Research in healthy adults shows that mental efficiency declines slightly but measurably as blood glucose falls below 3.6 mmol/l (65 mg/dl). Hormonal defense mechanisms ( adrenaline and glucagon ) are normally activated as it drops below a threshold level (about 3.0 mmol/l (55 mg/dl) for most people), producing the typical hypoglycemic symptoms of shakiness and dysphoria . [10] : 1589 Obvious impairment may not occur until the glucose falls below 2.2 mmol/l (40 mg/dl), and many healthy people may occasionally have glucose levels below 3.6 mmol/l (65 mg/dl) in the morning without apparent effects. ... In most people, subtle reduction of mental efficiency can be observed when the glucose falls below 3.6 mmol/l (65 mg/dl). Impairment of action and judgment usually becomes obvious below 2.2 mmol/l (40 mg/dl). ... As blood glucose levels fall below 0.55 mmol/l (10 mg/dl), most neurons become electrically silent and nonfunctional, resulting in coma . ... Throughout a 24‑hour period, blood plasma glucose levels are generally maintained between 4 and 8 mmol/l (72 and 144 mg/dl). [17] : 11 Although 3.3 or 3.9 mmol/l (60 or 70 mg/dl) is commonly cited as the lower limit of normal glucose, symptoms of hypoglycemia usually do not occur until 2.8 to 3.0 mmol/l (50 to 54 mg/dl). [18] In cases of recurrent hypoglycemia with severe symptoms, the best method of excluding dangerous conditions is often a diagnostic fast. ... If IV access cannot be established, the person can be given 1 to 2 mg of glucagon in an intramuscular injection .ABCC8, IGF2, SERAC1, HNF1A, INS, IL1B, TNF, SOD2, CACNA1C, GSR, SERPINA1, PPARA, CRH, PNMT, TH, GH1, GRIN2B, IGF1, G6PC, INSR, KCNJ11, HNF4A, ACADM, CPT1A, HADHA, GHSR, TANGO2, PGM1, HADH, PC, SETD2, AGL, PCK1, NR3C1, MEN1, MPI, TFAM, DBH, EIF2AK3, EIF2S3, ETFDH, NDUFS2, PTEN, FBP1, UQCRC2, GHR, SLC22A5, SLC37A4, HMGCL, UQCRB, NFKB2, PURA, GLI2, GLP1R, MPC1, NBAS, HSD17B10, NR1H4, PYGL, NDUFAF1, ROBO1, HMGCS2, TIMMDC1, HRAS, MRPS2, SEPSECS, RARB, WARS2, KCNMA1, NDUFS3, NDUFS4, NDUFS6, NDUFS8, NDUFV2, PPP2R5D, NOTCH3, OTC, OTX2, PPM1B, PCCA, PCCB, PCK2, NNT, GPR161, PHKA2, POU1F1, MLYCD, NDUFV1, NDUFS1, MRPS7, NDUFB10, CDON, PROP1, NDUFAF4, ACAD9, LRPPRC, APC2, NDUFB11, NDUFAF3, MPV17, MTO1, ND1, ND2, ND3, NDUFA1, NDUFA6, NDUFB3, NDUFB9, GPC3, GJA1, GK, PROKR2, SLC35A2, CA5A, SLC25A20, MICOS13, COG7, NDUFAF2, LHX4, COG8, NUBPL, CAMKMT, EHMT1, CYB561, NDUFAF5, DBT, CTDP1, DGUOK, DLD, NDUFA11, SGPL1, NSD1, BCS1L, ACADSB, KCNMA1-AS1, ACAT1, SUCLG1, ZGLP1, UQCC3, HESX1, ALDOB, NDUFS7, GOLGA6A, PTF1A, ACSF3, ATP5F1D, ATP7A, AUH, BCKDHA, BCKDHB, DPP4, CYP21A2, MTOR, GALT, FAH, RCBTB1, GPC4, PNPO, SLC52A1, MCCC2, PREPL, GCDH, WDR11, GCG, RNF125, GCK, SLC5A2, SAMD9, SLC3A1, DMXL2, FOXRED1, POMC, SOX3, MCCC1, ETFA, ETFB, TMEM126B, CYP2C9, ALB, SLC2A4, ACE, DSPP, FFAR1, SI, MGAM, SLC2A1, AKT2, GLUD1, HIF1A, NPY, SST, VEGFA, PRL, PIK3CA, ADRB2, TXN, KCNH2, GPR119, SLC5A1, UCP2, SLC2A2, IGFBP3, NFE2L2, SELENBP1, MAPK8, PPP1R13L, SHBG, ADIPOQ, TXNIP, SLC2A3, RNH1, PRKAA1, REN, AKT3, PIK3CG, PIK3CD, KDR, APRT, BDNF, ANTXR2, CPT2, CHPT1, GABPA, GDF1, CCHCR1, SHC3, GPT, HK1, IAPP, IL6, GIP, ARFIP2, PIK3CB, MFAP1, DNM1L, KCNH6, ARID1B, KL, MTA2, SEMA6A, SLC16A7, LPAR2, PDIA2, FTO, DHDDS, SOCS3, DAPK2, RPAIN, TIGAR, SLC52A3, SORCS1, CXCR6, CPT1C, SLC39A14, TBPL2, MIR155, MIR665, EMSLR, RIPK1, IRS2, KHSRP, TMPRSS11D, ACKR3, SOCS7, SH3BP1, GAL, ERO1A, PIAS1, HNRNPDL, CRYL1, PADI1, HGH1, FGF19, SIRT6, GLS2, KEAP1, RAPGEF5, WWOX, UQCRQ, KMT2B, DCAF1, FGF21, ROBO4, BNC2, DEPP1, VPS13C, TUBB3, H6PD, TMEM132A, MARCHF1, DENR, ACADL, MLRL, AAAS, TIMM8A, DNMT1, ARID3A, DSC3, EDNRA, EGFR, ELAVL1, ENO1, ENO2, ERBB4, ESRRA, F2R, F3, FBN1, FGF1, FGF2, FOS, NR5A1, GCGR, GHRH, GHRHR, GIPR, GLA, GCLC, GPER1, GPR42, GRIN1, GSK3B, GYS1, CYP2C8, CTNNB1, CRMP1, BID, ACADVL, ADCY5, ADRA1A, ADRA2B, AHR, AIF1, AKT1, APOE, APP, AQP4, AQP7, ARNT, AVP, BRS3, CRIP1, C3, CALD1, CCND2, CD34, CD36, CD59, LRBA, CDH15, CEBPA, CHAT, CHGA, CKB, CREM, FOXA2, HNRNPC, HNRNPL, SSTR4, PRKAR1A, PSMB9, PTHLH, RAD21, RB1, RIT2, RORC, SELP, SIAH2, ST3GAL4, SLC16A1, SLC22A1, SREBF1, STAR, PRKAA2, STAT5A, STAT5B, SYK, TAP1, TCF7L2, TGM2, TP53, TRH, UGDH, UTRN, VCAM1, CNBP, KMT2D, PRKAB1, PPY, AGFG1, MC4R, HTC2, IFNG, IGFBP6, KCNQ1, KHK, KIT, LEP, LEPR, LGALS1, LIPE, LPL, SMAD3, MAFD2, MET, PTPA, NR3C2, MTHFR, NHS, NUCB2, P4HB, PECAM1, PFKFB3, ABCB1, PIK3R2, POR, POU2F1, PPARD, PPARG, LOC102723407
-
Albuminuria
Wikipedia
The nephrotic syndrome usually results in the excretion of about 3.0 to 3.5 grams per 24 hours. [ medical citation needed ] Nephritic syndrome results in far less albuminuria. [ medical citation needed ] Microalbuminuria (between 30 and 300 mg/24h, [2] mg/l of urine [3] or μg/mg of creatinine [4] ) can be a forerunner of diabetic nephropathy . The term albuminuria is now preferred in Nephrology since there is not a "small albumin" ( micro albuminuria) or a "big albumin" ( macro albuminuria). [5] A1 represents normal to mildly increased urinary albumin/creatinine ratio (<30 mg/g or < 3 mg/mmmol); A2 represents moderately increased urinary albumin/creatinine ratio (30–300 mg/g or 3–30 mg/mmmol, previously known as microalbuminuria ); and A3 reflects severely increased urinary albumin/creatinine ratio >300 mg/g or > 30 mg/mmol). [1] Diagnosis [ edit ] The amount of protein being lost in the urine can be quantified by collecting the urine for 24 hours, measuring a sample of the pooled urine, and extrapolating to the volume collected.ACE, INS, TNF, PTGS2, NCK1, TSLP, REN, LEPR, IL6, GNAQ, SOD2, MIR130A, GPC5, MIR145, NPHS1, NPHS2, MIR155, CP, MIR424, CD38, NCK2, CASP1, PYCARD, AGT, TRPC3, TRPC6, SPP1, SH2B3, PDPN, AGER, LRP2, CSF1, ALB, EDN1, CYP11B1, CTSL, CTSB, RAB38, CASR, BAHCC1, HOTTIP, ARL15, LINC00862, CHD7, C2orf83, FBXL20, SHROOM3, SPATA5L1, ICA1L, SBF2, LRMDA, ADO, AK5, LINC02752, MAPKBP1, CPS1, CCT2, CWC27, USP3, SNX17, NRXN1, CUBN, AHR, AQP7, COL4A4, NMU, PEX1, MYL3, GALT, FUT1, CCL2, DCN, CCL5, SELP, VEGFA, ADD1
-
High Cholesterol
Mayo Clinic
These conversions are based on U.S. guidelines. Below 200 mg/dL Below 5.2 mmol/L Desirable 200-239 mg/dL 5.2-6.2 mmol/L Borderline high 240 mg/dL and above Above 6.2 mmol/L High LDL cholesterol (U.S. and some other countries) LDL cholesterol* (Canada and most of Europe) Results *Canadian and European guidelines differ slightly from U.S. guidelines. ... Below 100 mg/dL Below 2.6 mmol/L Optimal for people at risk of coronary artery disease or who have diabetes. ... High if there is coronary artery disease. 160-189 mg/dL 4.1-4.9 mmol/L High if there is no coronary artery disease. ... These conversions are based on U.S. guidelines. Below 40 mg/dL (men) Below 1.0 mmol/L (men) Poor Below 50 mg/dL (women) Below 1.3 mmol/L (women) 40-59 mg/dL (men) 1.0-1.5 mmol/L (men) Better 50-59 mg/dL (women) 1.3-1.5 mmol/L (women) 60 mg/dL and above Above 1.5 mmol/L Best Triglycerides (U.S. and some other countries) Triglycerides* (Canada and most of Europe) Results *Canadian and European guidelines differ slightly from U.S. guidelines. These conversions are based on U.S. guidelines. Below 150 mg/dL Below 1.7 mmol/L Desirable 150-199 mg/dL 1.7-2.2 mmol/L Borderline high 200-499 mg/dL 2.3-5.6 mmol/L High 500 mg/dL and above Above 5.6 mmol/L Very high Children and cholesterol testing For most children, the National Heart, Lung, and Blood Institute recommends one cholesterol screening test between the ages of 9 and 11, and then be repeated every five years after that.
-
Hyperlipoproteinemia, Type Id
OMIM
The hyperlipidemia was partially responsive to diet; fasting plasma triglyceride levels fell from as high as 3,366 mg/dL to as low as 744 mg/dL when the patient adhered to a fat-free diet. ... Gonzaga-Jauregui et al. (2014) reported a 5-week-old Hispanic girl who presented with severe hypertriglyceridemia (triglycerides, 12,031 mg/dL) and a combination of lower gastrointestinal bleeding and chylomicronemia. Initial colonoscopy was consistent with colitis, which resolved with reduction of triglycerides. She had a low HDL of 11 mg/dL and reduced LPL activity. Plengpanich et al. (2014) reported 3 sibs with chylomicronemia. Their plasma triglycerides ranged from 673 to 3,164 mg/dL, and HDL cholesterol was lowered to 16, 32, and 13, respectively. The proband was identified at 40 years of age after presenting with epigastric discomfort and a plasma triglyceride level of 2,050 mg/dL. Her BMI was normal, and her fasting plasma triglyceride level at 46 years of age was 3,164 mg/dL.
-
Scrub Typhus
Orphanet
Doxycycline is administered for a short time (3-7 days) in adults (200 mg/day) and children (2.2 mg/kg, twice daily). ... Patients with poor response to doxycycline and chloramphenicol, as well as pregnant women, can be treated with rifampicin (600-900 mg/day) or azithromycin (500 mg on the first day, then 250 mg/day).PRDX2, IFNG, TLR4, TNF, IL6, HSPD1, ALB, MAPK1, RELA, CCL2, SYT1, TLR2, VWF, XPO1, AIMP2, COPB2, GRAP2, GNLY, AHSA1, GPR182, RNF19A, POLDIP2, HAVCR1, HSPA14, ATG3, GORASP1, WNK1, NLRC5, LRSAM1, HTRA1, LAMC2, LCN2, GPT, CRP, MAPK14, CSF2, SLC25A10, HBEGF, EMD, F2, FOS, FOSB, GAPDH, GCY, CXCL2, CRK, HLA-A, HLA-C, HMGB1, IFNA1, IFNA13, IFNB1, IL1B, IL10, JUN, JUNB, JUND, PPP1R42
-
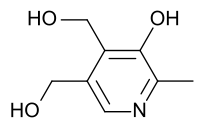
Pyridoxine-Dependent Epilepsy
Wikipedia
The disorder was first recognized in the 1950s, with the first description provided by Hunt et al. in 1954. [1] [2] [3] More recently, pathogenic variants within the ALDH7A1 gene have been identified to cause PDE. [1] [2] [3] [4] Contents 1 Genetics 2 Treatment 3 Monitoring 4 References 5 External links Genetics [ edit ] PDE is inherited in an autosomal recessive manner and is estimated to affect around 1 in 400,000 to 700,000 births, though one study conducted in Germany estimated a prevalence of 1 in 20,000 births. [1] [2] The ALDH7A1 gene encodes for the enzyme antiquitin or α -aminoadipic semialdehyde dehydrogenase, which is involved with the catabolism of lysine . [1] [2] [4] [5] Treatment [ edit ] Patients with PDE do not respond to anticonvulsant medications, but seizures rapidly cease with therapeutic intravenous doses of Vitamin B6 and remission from seizures are often maintained on daily therapeutic doses of Vitamin B6. [1] [2] [5] An optimal dose has not yet been established, but doses of 50–100 mg/day or 15–30 mg/kg/day have been proposed. [1] [2] Importantly, excessive doses of vitamin B6 can result in irreversible neurological damage, and therefore several guidelines recommend between 200 mg (neonates) and 500 mg per day as the maximal daily dose. [1] [2] Despite remission of seizure activity with vitamin B6 supplementation, intellectual disability is frequently seen in patients with PDE. [2] [6] Because the affected enzyme antiquitin is involved in the cerebral lysine degradation pathway, lysine restriction as an additional treatment modality has recently been explored. Studies have been published which demonstrate potential for improved biomarkers, development, and behavior in patients treated with lysine restriction in addition to pyridoxine supplementation. [2] [6] In trial, lysine restriction of 70–100 mg/kg/day in children less than 1 year of age, 45–80 mg/kg/day in children between 1–7 years of age, and 20–45 mg/kg/day in children older than 7 years of age were prescribed. [6] Despite the potential of additional benefit from lysine restriction, vitamin B6 supplementation remains the main-stay of treatment given lack of studies thus far demonstrating the safety and efficacy of lysine restriction for this purpose.