Load FindZebra Summary
Disclaimer:
FindZebra Search conducts a search using our specialized medical search engine.
FindZebra Summary uses the text completions API
(subject to OpenAI’s API data usage policies)
to summarize and reason about the search results.
The search is conducted in publicly available information on the Internet that we present “as is”.
You should be aware that FindZebra is not supplying any of the content in the search results.
FindZebra Summary is loading...
-
Neuroendocrine Tumor
Wikipedia
Some are asymptomatic. [ citation needed ] Animal neuroendocrine tumors include neuroendocrine cancer of the liver in dogs, and devil facial tumor disease in Tasmanian devils . [53] [54] [55] Familial syndromes [ edit ] Most pancreatic NETs are sporadic. [50] However, neuroendocrine tumors can be seen in several inherited familial syndromes, including: [29] multiple endocrine neoplasia type 1 (MEN1) multiple endocrine neoplasia type 2 (MEN2) von Hippel-Lindau (VHL) disease [29] neurofibromatosis type 1 [30] tuberous sclerosis [31] [32] Carney complex [33] [34] Given these associations, recommendations in NET include family history evaluation, evaluation for second tumors, and in selected circumstances testing for germline mutations such as for MEN1. [1] Pathophysiology [ edit ] NETs are believed to arise from various neuroendocrine cells whose normal function is to serve at the neuroendocrine interface. ... Neuron-specific enolase (NSE) is less specific . [1] [5] The nuclear neuroendocrine marker insulinoma-associated protein-1 (INSM1) has proven to be sensitive as well as highly specific for neuroendocrine differentiation. [66] NETs are often small, yellow or tan masses, often located in the submucosa or more deeply intramurally, and they can be very firm due to an accompanying intense desmoplastic reaction. ... Cryoablation has been less successful for GEP-NETs than RFA. [ citation needed ] AdVince, a type of gene therapy using a genetically modified oncolytic adenovirus [89] and supported by the crowdfunding campaign iCancer [90] was used in a Phase 1 trial against NET in 2016. [91] Epidemiology [ edit ] Although estimates vary, the annual incidence of clinically significant neuroendocrine tumors is approximately 2.5–5 per 100,000; [92] two thirds are carcinoid tumors and one third are other NETs. ... British Journal of Anaesthesia . 86 (4): 555–64. doi : 10.1093/bja/86.4.555 . ... Annals of the New York Academy of Sciences . 733 (1): 1–17. Bibcode : 1994NYASA.733....1L . doi : 10.1111/j.1749-6632.1994.tb17251.x .MEN1, CDKN1B, SSTR2, DAXX, ATRX, BRAF, TYMS, PTHLH, SSTR3, SSTR1, BAP1, MTOR, SST, GAST, SLC6A2, INSM1, CTNNB1, RET, PIK3CA, DNMT3A, POMC, EPHB1, PIK3CG, PIK3CD, CHGA, ELK3, CHEK2, PIK3CB, GRN, CD274, SMUG1, AKT1, GNA12, TP53, SYP, VEGFA, CDKN2A, ASCL1, BCL2, ENO2, NCAM1, GCG, MYCN, EGFR, MGMT, KIT, RASSF1, VHL, SCLC1, SSTR5, FOLH1, NKX2-1, KRAS, CALCA, CCND1, TAC1, PTPRF, VIP, NTS, PAX5, RHBDF2, GRP, IGF1, SDHD, GOT1, MAP2K7, CCK, ERBB2, DLL3, PPY, CXCL12, TP63, SMAD4, MUC1, INS, GCGR, CKAP4, NEUROD1, ISL1, MYC, NGF, SATB2, GLP1R, HSP90AA1, H3P10, HRAS, CHGB, CALR, NTRK1, TEK, DLK1, CDK4, CDX2, TGFA, UCHL1, RPE65, PGR, PDGFRA, CARTPT, CRH, UVRAG, SLC5A5, CXCR4, IGF1R, OTP, IL6, PHLDA3, TTF1, PAX8, TACR1, STK11, TRIM21, PLA2G15, SCG2, SQLE, SLC18A2, TERT, HDAC9, SLC2A1, PROM1, BCL2L11, NTSR1, PAX6, NAMPT, NOCT, INA, PLCB3, CD200, MKI67, PDX1, MAPK1, NES, HPSE, PTEN, STMN1, ABO, RIPK1, RORC, RAF1, IL1B, TRPV1, GATA3, ANGPT2, FOXM1, PTK2B, SDHAF2, ACCS, BDNF, EPAS1, EGF, ACSS2, MIB1, DNMT1, CCN2, TRPM8, CLDN4, CPE, CD34, CD44, FLNA, CEACAM5, B3GAT1, GH1, GIP, GHSR, GIPR, ADCY2, ALB, H3P28, TPPP2, H4C5, GGH, MIR1290, TMEM209, ELOA3, H4C13, H4C14, GPR151, SRPX, LGR5, TNFSF11, PSMG1, DCBLD2, H4-16, NRP1, MRGPRX4, SOCS1, H4C2, MIR3137, MRGPRX3, TNFRSF25, H3P12, CYYR1, AZIN2, DNER, AK6, MLIP, LMLN, NRP2, GPR68, MIR1246, H4C8, MAFK, MIR150, MIR155, MBOAT4, H4C9, MIR21, POTEKP, VN1R17P, SNORD95, GPR166P, ARID1A, EID3, SLC7A5, MIR375, H4C15, FZD4, MIRLET7C, OXER1, H4C12, HMGA2, H4C3, ARX, ELOA3B, GPRC6A, H4C11, H4C6, C17orf97, POTEM, MRGPRX1, ARMH1, H4C1, GADL1, ACTBL2, H4C4, BRI3, SQSTM1, ISYNA1, GHRL, ACOT7, KLF12, KRT20, SLC27A4, TET2, BCOR, EBNA1BP2, RALBP1, PGRMC1, LAMTOR1, FBXW7, MEG3, MAML3, TMEM127, NTNG1, ATRAID, KHDRBS1, DCTN4, SNORD61, NUP62, SNORD48, NTSR2, LPAR3, MAPK8IP2, SRRM2, BRD4, TRAM1, SPINK4, XIST, PPWD1, RBMS3, SETD1B, ZHX2, TNFSF13B, USE1, MAK16, UBE2Z, ONECUT2, FHL5, GCM2, DCLK1, ZBED1, ARHGEF2, PALB2, ALG9, SNED1, TET1, PDCD1LG2, TMPRSS13, MTA1, RPAIN, H1-10, EEF1E1, LGR6, PRMT5, NEUROD4, YAP1, SCML2, LANCL1, PAK4, RABEPK, ZNF197, CTNNBL1, PNO1, INSL5, EPB41L5, HDAC5, AKT3, CD302, GBA3, DCAF1, ATAT1, SERPINA3, VCL, CGA, ESR1, ERBB4, EPHB2, E2F1, DUSP2, DSG3, DPT, DPP4, DMBT1, DDC, DAD1, VCAN, CREB1, CRABP1, KLF6, CLU, FOXN3, CEACAM7, CEACAM3, ESR2, ETFA, EZH2, GHRH, HSPA4, AGFG1, HMOX1, HMGA1, GTF2H1, GSN, GNAS, GNA15, GFRA1, F3, GDNF, FSHR, FLT4, FLII, FLI1, FOXO1, FHIT, FGFR4, CGB3, CFL1, UQCRFS1, CDKN2C, FAS, APRT, APLP1, XIAP, APC, SLC25A6, SLC25A4, ANGPT1, ALK, AKT2, AFP, PARP1, ADCYAP1R1, ADCYAP1, ACVRL1, ACTN4, ACTG2, ACTG1, ACR, AQP4, ARF1, ATM, CASP3, CDK6, CD40LG, CD36, CD33, CCNE1, CCKBR, SERPINA6, CAV1, CA9, ATOH1, VPS51, C5, BRS3, BRCA2, DST, BAX, AVP, ATP4A, HTC2, HTR2A, TNC, IAPP, SDC1, SCT, SORT1, RNASE3, RARB, PTPRZ1, PTPRM, PTBP1, PSMD7, PSG2, PRKAR1A, PPP4C, POU4F1, PNN, PKD2, PITX2, PCYT1A, SERPINA5, PAX4, SDCBP, SDHB, SDHC, ST2, UBE2I, TPM3, TPH1, TNF, TM7SF2, TERC, TAT, STAT3, SSTR4, SEMA3F, SSR2, SOX11, SOX4, SOX2, SLPI, SLC3A2, SLC1A5, SFRP1, PAK3, PAK1, TNFRSF11B, KIF11, MDK, MAOA, LCN2, RPSA, L1CAM, KRT19, KRT7, KRT5, IL12A, MET, IL9, CXCL8, IL2, IL1A, IGFBP1, IGF2, IFNA13, IFNA1, MDM2, MFAP1, ODC1, MUTYH, NTRK2, NT5E, NRAS, NOTCH3, NPY, NOTCH1, NFKB1, NEFM, MUC4, CD99, NUDT1, COX2, MTAP, MST1R, MST1, MSMB, MMP7, MLH1, PTPRC
-
Neuroendocrine Tumor
GARD
A neuroendocrine tumor (NET) is a rare type of tumor that arises from specialized body cells called neuroendocrine cells . ... A p heochromocytoma is another, rarer type of NET that usually develops in the adrenal gland , but can also arise in other parts of the body. ... Functional NETs produce a specific set of symptoms due to the production of excess hormones, while non-functional NETs generally do not cause specific symptoms. In many cases, a person has no symptoms until the tumor spreads to the liver and/or impairs the function of an organ or system. This can make NETs very hard to diagnose. The majority of NETs are not inherited and occur sporadically in people with no family history of NETs. However, some NETs are associated with a hereditary cancer or tumor syndrome such as multiple endocrine neoplasia type 1 (most commonly), Von Hippel-Lindau disease , tuberous sclerosis , or neurofibromatosis type 1 (NF1).
-
Pancreatic Neuroendocrine Tumor
GARD
However in some cases, a pancreatic NET occurs outside of the pancreas. A NET arises from cells that produce hormones, so the tumor can also produce hormones. ... Pancreatic NETs are called either functional or nonfunctional. A functional pancreatic NET causes specific symptoms because it makes extra hormones, such as gastrin, insulin, or glucagon. ... Pancreatic NETs can be hard to diagnosis, often not identified until 5 to 10 years after they begin to grow. Most pancreatic NETs are not inherited and occur sporadically in people with no family history of NETs.MEN1, PCSK1, ATM, BRCA2, C11orf65, IGF2, SST, TP53, CDKN2A, SLC6A2, MTOR, EPHB1, POMC, GH1, GCGR, DAXX, ELK3, KRT19, SSTR2, CHGA, SSTR5, UCHL1, FZD4, GCM2, DLGAP1, DCLK1, SSTR4, INA, STK11, EIF2AK3, TFE3, THBD, CXCR4, PAX8, TSC1, TTR, TYMS, VEGFA, ABO, CNPY2, MRGPRX4, GPR166P, VN1R17P, MIR196A1, GADL1, MRGPRX1, GPRC6A, OXER1, GPR119, GPR151, MRGPRX3, SEMA3A, AZIN2, ACCS, STK33, LGR6, ACSS2, MEG3, NEUROG3, LPAR3, LILRB1, PLA2G15, RET, SLC2A3, INSM1, GRN, FFAR1, GHRH, GAST, FGFR4, F3, EGFR, DHCR24, CSF1, CRH, CHGB, CD44, CCK, CALCA, VPS51, ATRX, ASS1, ASCL1, ANGPT2, HSF1, PDX1, SLC2A2, KIT, SLC2A1, SEA, SDHB, SDHA, AKT1, PYGM, PTH, PTEN, PPY, PTPA, PGR, PCYT1A, PCNA, NFKB1, NEUROD1, MUC1, SMAD4, STMN1, KRAS, H3P10
-
Malaria
Wikipedia
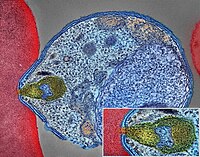
Malaria Malaria parasite connecting to a red blood cell Pronunciation / m ə ˈ l ɛər i ə / Specialty Infectious disease Symptoms Fever, vomiting, headache, yellow skin [1] Complications Seizures , coma [1] Usual onset 10–15 days post exposure [2] Causes Plasmodium spread by mosquitoes [1] Diagnostic method Examination of the blood, antigen detection tests [1] Prevention Mosquito nets , insect repellent , mosquito control , medications [1] Medication Antimalarial medication [2] Frequency 228 million (2018) [3] Deaths 405,000 in 2018 [3] Malaria is a mosquito-borne infectious disease that affects humans and other animals. [2] Malaria causes symptoms that typically include fever , tiredness , vomiting , and headaches . [1] In severe cases, it can cause yellow skin , seizures , coma , or death . [1] Symptoms usually begin ten to fifteen days after being bitten by an infected mosquito . [2] If not properly treated, people may have recurrences of the disease months later. [2] In those who have recently survived an infection , reinfection usually causes milder symptoms. [1] This partial resistance disappears over months to years if the person has no continuing exposure to malaria. [1] Malaria is caused by single-celled microorganisms of the Plasmodium group. [2] The disease is most commonly spread by an infected female Anopheles mosquito. [2] The mosquito bite introduces the parasites from the mosquito's saliva into a person's blood . [2] The parasites travel to the liver where they mature and reproduce . [1] Five species of Plasmodium can infect and be spread by humans. [1] Most deaths are caused by P. falciparum , whereas P. vivax , P. ovale , and P. malariae generally cause a milder form of malaria. [1] [2] The species P. knowlesi rarely causes disease in humans. [2] Malaria is typically diagnosed by the microscopic examination of blood using blood films , or with antigen-based rapid diagnostic tests . [1] Methods that use the polymerase chain reaction to detect the parasite's DNA have been developed, but are not widely used in areas where malaria is common due to their cost and complexity. [4] The risk of disease can be reduced by preventing mosquito bites through the use of mosquito nets and insect repellents or with mosquito-control measures such as spraying insecticides and draining standing water . [1] Several medications are available to prevent malaria in travellers to areas where the disease is common. [2] Occasional doses of the combination medication sulfadoxine/pyrimethamine are recommended in infants and after the first trimester of pregnancy in areas with high rates of malaria. [2] As of 2020, there is one vaccine which has been shown to reduce the risk of malaria by about 40% in children in Africa. [5] [6] Efforts to develop more effective vaccines are ongoing. [6] The recommended treatment for malaria is a combination of antimalarial medications that includes artemisinin . [1] [2] The second medication may be either mefloquine , lumefantrine , or sulfadoxine/pyrimethamine. [7] Quinine , along with doxycycline , may be used if artemisinin is not available. [7] It is recommended that in areas where the disease is common, malaria is confirmed if possible before treatment is started due to concerns of increasing drug resistance . [2] Resistance among the parasites has developed to several antimalarial medications; for example, chloroquine -resistant P. falciparum has spread to most malarial areas, and resistance to artemisinin has become a problem in some parts of Southeast Asia. [2] The disease is widespread in the tropical and subtropical regions that exist in a broad band around the equator . [1] This includes much of sub-Saharan Africa , Asia , and Latin America . [2] In 2018 there were 228 million cases of malaria worldwide resulting in an estimated 405,000 deaths. [3] Approximately 93% of the cases and 94% of deaths occurred in Africa. [3] Rates of disease have decreased from 2010 to 2014 but increased from 2015 to 2017, during which there were 231 million cases. [3] Malaria is commonly associated with poverty and has a significant negative effect on economic development . [8] [9] In Africa, it is estimated to result in losses of US$12 billion a year due to increased healthcare costs, lost ability to work, and adverse effects on tourism. [10] Play media Video summary ( script ) Contents 1 Signs and symptoms 1.1 Complications 2 Cause 2.1 Life cycle 2.2 Recurrent malaria 2.3 Climate change 3 Pathophysiology 3.1 Genetic resistance 3.2 Liver dysfunction 4 Diagnosis 4.1 Classification 5 Prevention 5.1 Mosquito control 5.1.1 Insecticide treated nets 5.1.2 Indoor residual spraying 5.1.3 Housing modifications 5.1.4 Other mosquito control methods 5.2 Medications 5.3 Others 6 Treatment 6.1 Uncomplicated malaria 6.2 Severe and complicated malaria 6.3 Resistance 7 Prognosis 8 Epidemiology 9 History 10 Society and culture 10.1 Economic impact 10.2 Counterfeit and substandard drugs 10.3 War 10.4 Eradication efforts 11 Research 11.1 Vaccine 11.2 Medications 11.3 New targets 11.4 Other 12 Other animals 13 References 13.1 Citations 13.2 Sources 14 Further reading 15 External links Signs and symptoms [ edit ] Main symptoms of malaria [11] The signs and symptoms of malaria typically begin 8–25 days following infection, [11] but may occur later in those who have taken antimalarial medications as prevention . [4] Initial manifestations of the disease—common to all malaria species—are similar to flu-like symptoms , [12] and can resemble other conditions such as sepsis , gastroenteritis , and viral diseases . [4] The presentation may include headache , fever , shivering , joint pain , vomiting , hemolytic anemia , jaundice , hemoglobin in the urine , retinal damage , and convulsions . [13] The classic symptom of malaria is paroxysm —a cyclical occurrence of sudden coldness followed by shivering and then fever and sweating, occurring every two days ( tertian fever ) in P. vivax and P. ovale infections, and every three days ( quartan fever ) for P. malariae . ... The mosquitoes remain on the wall until they fall down dead on the floor. Insecticide treated nets [ edit ] A mosquito net in use. Mosquito nets help keep mosquitoes away from people and reduce infection rates and transmission of malaria. Nets are not a perfect barrier and are often treated with an insecticide designed to kill the mosquito before it has time to find a way past the net. Insecticide-treated nets are estimated to be twice as effective as untreated nets and offer greater than 70% protection compared with no net. [73] Between 2000 and 2008, the use of ITNs saved the lives of an estimated 250,000 infants in Sub-Saharan Africa. [74] About 13% of households in Sub-Saharan countries owned ITNs in 2007 [75] and 31% of African households were estimated to own at least one ITN in 2008. ... That number increased to 20.3 million (18.5%) African children using ITNs in 2007, leaving 89.6 million children unprotected [76] and to 68% African children using mosquito nets in 2015. [77] Most nets are impregnated with pyrethroids , a class of insecticides with low toxicity .ICAM1, FCGR2B, HBB, CD36, NOS2, FCGR2A, TNF, CR1, G6PD, CRP, HP, ACKR1, GYPA, SLC4A1, GYPB, NCR3, TIRAP, GYPC, LTBR, CISH, IFNG, HMOX1, PKLR, ABO, ANK1, AQP4, ATP2B4, HBG2, CYTB, ENOSF1, MSMB, MST1, ZNF536, LINC00944, SMARCB1, DHODH, PDR, TREML4, ZNF804A, OR51F1, OR51B5, CDH13, PROCR, SPATA3, OR51N1P, DHFR, DDT, RECQL4, FAM155A, IGHG3, IL4, MMP26, IL6, IL10, TLR9, HLA-DRB1, CSMD1, HBE1, DNAJC5, TMPRSS13, KLHL3, HDGFL2, TLR4, ATAD1, LMLN, TENM3-AS1, MECP2, POMGNT2, MBL2, TFRC, TGFB1, MIF, HLA-B, HAMP, DHPS, SERPINA3, TLR2, IL1B, FOXP3, FHL5, ACOT7, POTEKP, POTEM, GEM, KIR3DL1, RN7SL263P, ACTG2, ACTG1, ACTB, ACTBL2, HBA2, CYP2B6, HSPA4, LSAMP, TRAP, FCGR3B, HSP90AA1, IL1A, LAMP3, CD81, OR10A4, CCL5, ABCB1, FAS, CD40LG, TEP1, CXCL8, IARS1, HLA-G, CTLA4, HBA1, INSRR, ANGPT2, TYMS, CFH, GSTP1, IFNAR1, AGT, GYPE, FCGR3A, TXN, IL13, HSPB3, APOE, MTCO2P12, ISYNA1, FCGR2C, FYB1, VDR, HLA-A, GSTM1, GSR, ATR, MBL3P, LAIR1, PNP, IL12B, MNAT1, IL1RN, CYP2D6, IGF1, CD55, ACHE, DECR1, COX2, IL3, CCL2, MAPK1, NLRP3, FBXW7, HAVCR2, THBD, VPS51, EMP1, ITGA2B, PTGS2, ANC, IL10RA, XPO1, VNN1, PLEK, UMPS, IL2, IL2RA, TPPP, VWF, ISG20, ADAMTS13, IRF1, IL7R, AIMP2, IL12RB1, CLEC11A, METAP2, CDK5R1, ING1, IL18R1, PGD, HAP1, H6PD, PRDX5, GRAP2, CXCL9, MMP9, MPO, TAP1, CCL4L2, COX1, EBI3, ITGAX, COX3, TLR6, CXCL11, MTHFR, NFKB2, NFYA, NOS1, TBC1D9, ORC1, MCF2, AKAP13, RNF19A, TLR7, NT5C3A, IRAK4, KIR2DS1, CCL4, KIR3DL2, ICOS, COQ2, PSIP1, PECAM1, TPT1, RNASE3, ARTN, TP53, POLDIP2, PDCD1, TLR1, AHSA1, UBL4A, AQP3, AGRP, H3C9P, CYP2C8, CYP2C19, GTF2H4, CRK, RNA18SN5, ANXA2, H3P37, CASP1, NANP, CCL4L1, MAPK14, CXCR3, GNAS, GLO1, FCN2, SMIM10L2B, FKBP4, CD27, FOXO3, RBM45, HM13, IL33, HK1, CCR5, IFNA13, IFNA1, H3P42, DNAJB1, CHIT1, CYP3A4, SMIM10L2A, EGF, CHI3L1, CAT, EPHA2, NSFL1C, ADRB2, MYMX, COX8A, GAPDH, ABCB6, NR1I3, TREML1, PUM3, FMN1, TICAM2, TRIM13, BMS1, FZD4, RABEPK, LANCL1, FUT9, TNFSF13B, DCTN6, CXCR6, ARL6IP5, MRGPRX1, ZNRD2, ASPM, KAT5, RAB7B, CIB1, SEMA3C, ARMH1, STING1, CFDP1, CPQ, MYLK4, DLC1, AKR1A1, PIEZO1, TMPRSS11D, HDAC9, CARTPT, DEFB4B, TIMELESS, SPHK1, TMED7-TICAM2, PSC, VNN2, PROM1, UPK3B, H3P23, H3P28, TNFRSF11A, TNFRSF18, TP63, PDXK, CNTNAP1, DHX16, STK24, H3P19, LOH19CR1, WASHC1, WASH6P, LPAR2, MIR146A, APOBEC3B, SPAG6, CLOCK, ATG5, MIR142, AIM2, ABCG2, PCSK9, MIR155, NCF1, PPIG, MIR29A, VN1R17P, GPR166P, CD163, MIR451A, CXADRP1, ARHGEF2, CERS1, SPINK5, MASP2, GEMIN4, ACD, TLR8, MPPE1, MCPH1, HSPA14, RNF34, TMED7, ARMC9, PPP1R2C, IL22, TRAF3IP2, A1CF, PDCD1LG2, SLC44A4, SGSM3, MCAT, HPGDS, B3GAT1, ROPN1L, PHGDH, RAB14, IL23A, ABCG4, IFIH1, CFC1, BTNL2, MARCHF1, POLE4, CMC2, TMED9, ACKR3, PDXP, RHOF, AICDA, POLD4, RBM25, TOLLIP, TREM1, LGR6, ADA2, BACH2, ERAP1, GOLPH3, PARS2, KRT88P, TRIM5, IL17RE, CHP1, GPR151, NRSN1, EIF5AL1, CD160, APCDD1, ERFE, OXER1, DNAJB1P1, DSTN, GPRC6A, CCNI, ADIRF, EBNA1BP2, TMED2, EHD1, RNPS1, HPSE, SEPTIN9, SCLT1, NT5C2, SLC25A21, LEO1, NLRP12, TIMD4, CDCA5, DBA2, CARD16, PTPMT1, CGAS, RAB39B, TADA1, MRGPRX3, MRGPRX4, PGLS, PANX1, SPO11, LPAR3, CBX5, POFUT2, SPPL3, NBEAL2, LUC7L, PTPRC, FGF23, EIF5, FLT3LG, FLT1, FECH, FBN2, FBN1, FANCD2, F3, EPO, ENO2, ADGRE1, ELK4, ELF4, EIF5A, EIF4G2, CXADR, EGR3, EDNRA, EDN1, S1PR3, RCAN1, ATN1, DNMT1, DEFB4A, DHX9, ACE, DBP, CYP1A2, CYC1, GABPA, GCHFR, GDF1, GPR42, IL4R, IL1R1, IGFBP1, IFNGR1, IFNB1, IFNA2, IFI27, IDE, HTN3, HSPA9, HSD11B1, HRES1, HPRT1, HPR, HPGD, HMGB1, HLA-DOA, UBE2K, HGF, SERPIND1, HBG1, GTF3A, GSTT1, GSN, GPX1, GPT, GRK5, CYBB, CTSL, IL9, ANXA1, C3, BSG, BRS3, BRCA2, PRDM1, BCL2, BAX, ASPA, ASIP, ARR3, NUDT2, ANXA7, ANXA4, ANPEP, CSH2, AMBP, ALOX5, ALB, AHR, AFP, ADSL, ADRA2B, ADRA1A, ADORA2A, ADH1B, ADA, ACP1, ACACA, CAST, CASR, CD1B, CD1C, CSH1, CSF1R, CSF1, CS, CRYZ, CREM, CR2, CLDN4, CPB1, CNTF, CCR4, CLU, ERCC8, CTSC, CEL, CDC25C, CD69, CD68, CD40, ENTPD1, CD34, CD28, CD19, CD14, CD9, CD1E, CD1D, IL5, IL12A, FOSL1, SELE, SPTA1, SPP1, SPINK1, SPG7, SOD3, SOD1, SMN1, SLC16A1, SLC11A1, SLC6A7, SLC2A1, SGCG, SET, SEA, ABCA1, SDC1, CXCL5, CCL22, CCL18, CCL3L1, CCL3, CCL1, SAFB, SORT1, RPS19, RBP2, RANBP2, PEX19, SSR2, SSTR4, DENND2B, STAT6, DDX39B, PRRC2A, PFBI, RAB7A, CXCR4, MOGS, ZBTB16, TRPV1, VCP, USP1, TYRP1, TTR, TTPA, TRPC1, TRP-AGG2-5, TPO, TPH1, TNFRSF1B, TLR3, TGFB2, TRBV20OR9-2, TCN2, HNF1A, TADA2A, ADAM17, TAC1, STK3, PTPRH, PTHLH, IL15, KIR3DS1, MAL, MAF, LTB, LTA, LMAN1, LEPR, LDLR, LCN2, LBR, RPSA, LAG3, KRT13, KNG1, KIR2DS5, PSMD9, KIR2DL3, KIR2DL2, KDR, KCNG1, KARS1, ITPA, ITGB2, ITGAM, ITGAL, CXCL10, IDO1, ILF3, IL18, MAP2, MAP6, MEFV, MVD, PSMD7, PSMD2, PSMB9, PSEN1, PSAP, PRSS1, PROC, MAP2K1, PRKG1, PRKAR1A, PPP1R1A, PPARG, SEPTIN4, PLP1, PGM1, PGAM1, P2RX7, SLC22A18, TNFRSF11B, OMD, ODC1, NOS3, NQO2, NFE2L2, NEK2, MYD88, MYC, H3P5
-
Familial Gastric Type 1 Neuroendocrine Tumor
Orphanet
A rare neoplastic disease characterized by occurrence of atypical and aggressive gastric type 1 neuroendocrine tumors (NET) in early adulthood. ... Patients present high serum gastrin concentrations and iron-deficiency anemia (rather than megaloblastic anemia, which is a typical feature in patients with sporadic gastric type 1 NET, where the tumor usually arises on the background of autoimmune atrophic gastritis).
-
Postural Orthostatic Tachycardia Syndrome Due To Net Deficiency
Orphanet
A rare, genetic, primary orthostatic disorder characterized by dizziness, palpitations, fatigue, blurred vision and tachycardia following postural change from a supine to an upright position, in the absence of hypotension. A syncope with transient cognitive impairment and dyspnea may also occur. The norepinephrine transporter deficiency leads to abnormal uptake and high plasma concentrations of norepinephrine.
-
Neuroendocrine Neoplasm Of Esophagus
Orphanet
A group of esophageal epithelial neoplasms characterized by neuroendocrine differentiation, comprising well-differentiated neuroendocrine tumors (NETs), poorly differentiated neuroendocrine carcinomas (NECs), and mixed neuroendocrine-non-neuroendocrine neoplasms, an umbrella category including mixed adenoneuroendocrine carcinoma. ... NECs may also arise in other parts of the esophagus. On endoscopy, NETs usually appear as small polypoid or nodular submucosal masses, while NECs are large, infiltrative, and ulcerated. Patients most commonly present with dysphagia, pain, weight loss, and sometimes melena. Metastatic NETs may be associated with carcinoid syndrome.
-
Pancreatic Neuroendocrine Tumor
Wikipedia
Pancreatic neuroendocrine tumor Specialty Oncology Treatment radiation, chemotherapy Prognosis Five year survival rate ~ 61% Pancreatic neuroendocrine tumors ( PanNETs , PETs , or PNETs ), often referred to as "islet cell tumors", [1] [2] or "pancreatic endocrine tumors" [3] [4] are neuroendocrine neoplasms that arise from cells of the endocrine ( hormonal ) and nervous system within the pancreas . ... Contents 1 Types 2 Signs and symptoms 3 Diagnosis 4 Staging 5 Treatment 6 Genetics 7 References 8 External links Types [ edit ] The majority of PanNETs are benign , while some are malignant . ... Current Treatment Options in Oncology . 13 (1): 24–34. doi : 10.1007/s11864-011-0172-2 . ... National Cancer Institute. March 7, 2014. [1] ^ a b The PanNET denomination is in line with current WHO guidelines. ... "Update on pancreatic neuroendocrine tumors" . Gland Surgery . 3 (4): 258–75. doi : 10.3978/j.issn.2227-684X.2014.06.03 .
-
Esophageal Food Bolus Obstruction
Wikipedia
"Oesophageal foreign bodies" . British Medical Journal . 1 (5957): 561–3. doi : 10.1136/bmj.1.5957.561 . ... The British Journal of Surgery . 65 (1): 5–9. doi : 10.1002/bjs.1800650103 . ... Journal of Clinical Gastroenterology . 41 (4): 356–61. doi : 10.1097/01.mcg.0000225590.08825.77 . ... Annals of the Royal College of Surgeons of England . 93 (6): 441–4. doi : 10.1308/003588411X588090 . ... Archives of Surgery . 105 (5): 790–1. doi : 10.1001/archsurg.1972.04180110107028 .
-
Clanging
Wikipedia
This is associated with the irregular thinking apparent in psychotic mental illnesses (e.g. mania and schizophrenia ). [1] Gustav Aschaffenburg found that manic individuals generated these "clang-associations" roughly 10–50 times more than non-manic individuals. [2] Aschaffenburg also found that the frequency of these associations increased for all individuals as they became more fatigued. [3] Clanging refers specifically to behavior that is situationally inappropriate. While a poet rhyming is not evidence of mental illness, disorganized speech that impedes the patient's ability to communicate is a disorder in itself, often seen in schizophrenia. [4] See also [ edit ] Thought disorder Word salad References [ edit ] ^ Peralta, Victor; Cuesta, Manuel J.; de Leon, Jose (March 1992). ... Livingstone. p. 32 . ^ Spitzer, Manfred (1999). The mind within the net: Models of learning, thinking, and acting . ... "Schizophrenia and the structure of language: the linguist's view" (PDF) . Schizophr. Res . 77 (1): 85–98. CiteSeerX 10.1.1.532.2190 . doi : 10.1016/j.schres.2005.01.016 .
-
Dogger Bank Itch
Wikipedia
The sea chervil, abundant in the area, frequently came up with the fishing nets and had to be thrown back into the water. ... "Fisherman's 'Dogger Bank Itch ' ". Allergy . 1 : 40–46. doi : 10.1111/j.1398-9995.1948.tb03301.x . ^ Carle JS, Christophersen C (1980). ... Comparative Biochemistry and Physiology B . 128 (1): 27–30. doi : 10.1016/S1096-4959(00)00316-X . ... Journal of Dermatological Treatment . 12 (1): 23–24. doi : 10.1080/095466301750163536 . ... Toxicon . 20 (1): 307–10. doi : 10.1016/0041-0101(82)90232-X .
-
Retiform Parapsoriasis
Wikipedia
Retiform parapsoriasis Specialty Dermatology Retiform parapsoriasis is a cutaneous condition, considered to be a type of large-plaque parapsoriasis . [1] It is characterized by widespread, ill-defined plaques on the skin, that have a net-like or zebra-striped pattern. [2] Skin atrophy , a wasting away of the cutaneous tissue , usually occurs within the area of these plaques. [1] See also [ edit ] Parapsoriasis Poikiloderma vasculare atrophicans List of cutaneous conditions References [ edit ] ^ a b Lambert WC, Everett MA (Oct 1981). "The nosology of parapsoriasis". J. Am. Acad. Dermatol . 5 (4): 373–95. doi : 10.1016/S0190-9622(81)70100-2 . ... Dermatology: 2-Volume Set . St. Louis: Mosby. ISBN 1-4160-2999-0 . External links [ edit ] Classification D ICD - 10 : L41.5 ICD - 9-CM : 696.2 v t e Papulosquamous disorders Psoriasis Pustular Generalized pustular psoriasis ( Impetigo herpetiformis ) Acropustulosis / Pustulosis palmaris et plantaris ( Pustular bacterid ) Annular pustular psoriasis Localized pustular psoriasis Other Guttate psoriasis Psoriatic arthritis Psoriatic erythroderma Drug-induced psoriasis Inverse psoriasis Napkin psoriasis Seborrheic-like psoriasis Parapsoriasis Pityriasis lichenoides ( Pityriasis lichenoides et varioliformis acuta , Pityriasis lichenoides chronica ) Lymphomatoid papulosis Small plaque parapsoriasis ( Digitate dermatosis , Xanthoerythrodermia perstans ) Large plaque parapsoriasis ( Retiform parapsoriasis ) Other pityriasis Pityriasis rosea Pityriasis rubra pilaris Pityriasis rotunda Pityriasis amiantacea Other lichenoid Lichen planus configuration Annular Linear morphology Hypertrophic Atrophic Bullous Ulcerative Actinic Pigmented site Mucosal Nails Peno-ginival Vulvovaginal overlap synromes with lichen sclerosus with lupus erythematosis other: Hepatitis-associated lichen planus Lichen planus pemphigoides Other Lichen nitidus Lichen striatus Lichen ruber moniliformis Gianotti–Crosti syndrome Erythema dyschromicum perstans Idiopathic eruptive macular pigmentation Keratosis lichenoides chronica Kraurosis vulvae Lichen sclerosus Lichenoid dermatitis Lichenoid reaction of graft-versus-host disease This dermatology article is a stub .
-
Uric Acid Concentration, Serum, Quantitative Trait Locus 1
OMIM
Genetic Heterogeneity of Serum Uric Acid Concentration Quantitative Trait Loci See also UAQTL2 (see 612076), conferred by variation in the SLC2A9 gene (606142) on chromosome 4p; UAQTL4 (612671), conferred by variation in the SLC17A3 gene (611034) on chromosome 6p21; UAQTL5 (614746), associated with a SNP on chromosome 19q13; and UAQTL6 (614747), associated with a SNP on chromosome 1. Mapping The Pacific Austronesian population, including Taiwanese aborigines, has a remarkably high prevalence of hyperuricemia and gout, suggesting a founder effect across the Pacific region. ... The findings were replicated in the ARIC cohort of 11,024 white and 3,843 black individuals, yielding p values of 9.7 x 10(-30) and 9.8 x 10(-4), respectively. The combined p value for white individuals from all 3 cohorts was 2.5 x 10(-60), and further analysis showed that the SNP was direction-consistent with the development of gout in white participants (OR of 1.74; p = 3.3 x 10(-15)). Pathogenesis Martinon et al. (2006) showed that monosodium urate (MSU) and calcium pyrophosphate dihydrate (CPPD), both crystals found in gout, engage the caspase-1 (CASP1; 147678)-activating NALP3 (606416) inflammasome, resulting in the production of active interleukin (IL1)-1-beta (IL1B; 147720) and IL18 (IL18; 600953). ... Evidence for both an increased rate of uric acid synthesis and an impaired net elimination of uric acid by the kidney has been advanced. ... Autosomal dominant form Lab - Increased rate of uric acid synthesis - Impaired net elimination of uric acid by the kidney - Hyperuricemia Skin - Urate tophi ▲ Close
-
Afterdepolarization
Wikipedia
Abnormal depolarizations of cardiac myocytes Afterdepolarizations are abnormal depolarizations of cardiac myocytes that interrupt phase 2, phase 3, or phase 4 of the cardiac action potential in the electrical conduction system of the heart . ... Early afterdepolarizations can result in torsades de pointes , tachycardia , and other arrhythmias . [1] EADs can be potentiated by hypokalemia and drugs that prolong the QT interval , including class Ia and III antiarrhythmic agents . ... Delayed afterdepolarizations (DADs) begin during phase 4, after repolarization is completed but before another action potential would normally occur via the normal conduction systems of the heart. They are due to elevated cytosolic calcium concentrations, classically seen with digoxin toxicity. [3] [4] The overload of the sarcoplasmic reticulum may cause spontaneous Ca 2+ release after repolarization, causing the released Ca 2+ to exit the cell through the 3Na + /Ca 2+ -exchanger. This results in a net depolarizing current. The classical feature is Bidirectional ventricular tachycardia .
-
Insulinoma
GARD
Insulinoma is a type of pancreatic neuroendocrine tumor (pancreatic NET), which refers to a group of rare tumors that form in the hormone-making cells of the pancreas. ... However, people with specific genetic syndromes such as multiple endocrine neoplasia type I , Von Hippel-Lindau syndrome , Neurofibromatosis type 1 , and tuberous sclerosis are at risk of insulinomas and other endocrine tumors .MEN1, RPS15, CDKN2B, CDKN2C, IAPP, GCG, CDKN1B, CDKN1A, SST, FOXM1, GLP1R, PDX1, INS, IL1B, RIT2, PTPRN2, GAD1, EHMT1, IGF2, ZGLP1, CDKN2A, SLC30A8, SLC30A10, GCK, SSTR2, FFAR1, YY1, LEP, DPP4, INSM1, MNX1, HSPD1, GAD2, SLC2A2, CASR, RALBP1, RIPK1, PDHX, BTC, UQCRFS1, TP53, TGM2, SSTR5, CDKN1C, INSR, ABCC8, SLC6A2, SSTR4, SSTR3, WFS1, NIT1, SERPINA1, PTPRN, GIP, GCKR, CORO1A, H3P47, PRL, H3P10, ERBB2, GAST, EGR1, ELK3, CALCA, CASP3, EPHB1, G6PC, DLK1, CCN5, SQSTM1, PTTG1, GCM2, LHX2, KL, MAPK8IP1, INSL5, IRS2, ZNRD2, KHDRBS1, DCTN6, LILRB1, FASTK, CCND1, PDIA5, FAS, ATF6, KDM1A, PDZD2, BCL2, BRCA1, TNKS, PLA2G6, HNF1A, TCF19, TGFA, TGFB1, CASP8, THBD, TKT, TSPAN7, TPD52, TRP-AGG2-5, TRPC1, EIPR1, TXN, TYRP1, UCP2, VDR, CACNA1D, BRAF, STAB1, ERP44, NUP62, KCNH4, CAT, KCNH8, GPR119, STOML3, AKT1, HCAR2, GOLGA6A, TICAM2, HES3, MIR107, MIR144, MIR155, MIR204, MIR21, MIR375, INS-IGF2, ADSS2, TMED7-TICAM2, ECT, LINC02210-CRHR1, H3P23, ADM, SLC22A12, TXNDC5, TRABD, RCBTB1, FGF21, MCAT, MCTS1, TMED7, ADIPOR1, DCTN4, CDKAL1, SLC25A38, BANK1, MEG3, ZC3H12A, APOC2, SOX6, SELENOS, IGSF9, SEMA6A, HAMP, G6PC2, PDIA2, ANGPT2, SYP, STAT5A, STC1, STAT5B, KCNJ1, KCNJ6, KRT8, KRT16, KRT19, DECR1, LEPR, LGALS3, LMO2, EPCAM, SMAD2, SMAD3, SMAD4, MAPT, MC2R, MDK, RAB8A, CUX1, MET, CIITA, MLH1, EGF, EGFR, INPPL1, HK1, MTOR, FGF13, GNA12, GPD2, FBN1, GRN, GSK3B, GSR, GTF2H1, ESR2, ELK1, HLA-DQB1, HMGN2, HNF4A, EPHB2, IFI27, IGFBP1, IGFBP2, IL4, IL10, MRC1, NCAM1, NEDD4, SLC2A1, RAP1A, REG1A, CPE, CMA1, S100A8, SCT, CCL2, CXCL12, SDHD, CHGA, RAB3A, CDKN2D, SLC16A1, SNX1, CDC42, CDK1, CCND3, CCNC, CCK, STAT1, RANBP2, CR2, NF1, PIK3CG, NFE2L1, CTSB, NME1, OPA1, PAX4, PAX6, PCSK1, ENPP1, CTNNB1, PKD1, CRHR1, POLD1, MAPK1, MAPK3, MAPK8, ADCYAP1, PRSS1, PSEN2, PSMD9, PTEN, ACO2
-
West Nile Fever
Wikipedia
West Nile fever West Nile virus Specialty Infectious disease Symptoms None, fever , headache, vomiting or diarrhea and muscle aches rash [1] Complications Encephalitis , meningitis [1] Usual onset 2 to 14 days after exposure [1] Duration Weeks to months [1] Causes West Nile virus spread by mosquito [1] Diagnostic method Based on symptoms and blood tests [1] Prevention Reducing mosquitoes, preventing mosquito bites [1] Treatment Supportive care (pain medication) [1] Prognosis 10% risk of death among those seriously affected [1] West Nile fever is an infection by the West Nile virus , which is typically spread by mosquitoes . [1] In about 80% of infections people have few or no symptoms . [2] About 20% of people develop a fever , headache, vomiting, or a rash. [1] In less than 1% of people, encephalitis or meningitis occurs, with associated neck stiffness, confusion, or seizures. [1] Recovery may take weeks to months. [1] The risk of death among those in whom the nervous system is affected is about 10%. [1] West Nile virus (WNV) is usually spread by mosquitoes that become infected when they feed on infected birds, which often carry the disease . [1] Rarely the virus is spread through blood transfusions, organ transplants, or from mother to baby during pregnancy, delivery, or breastfeeding, [1] but it otherwise does not spread directly between people. [3] Risks for severe disease include being over 60 years old and having other health problems. [1] Diagnosis is typically based on symptoms and blood tests. [1] There is no human vaccine . [1] The best way to reduce the risk of infection is to avoid mosquito bites. [1] Mosquito populations may be reduced by eliminating standing pools of water, such as in old tires, buckets, gutters, and swimming pools. [1] When mosquitoes cannot be avoided, mosquito repellent , window screens , and mosquito nets reduce the likelihood of being bitten. [1] [3] There is no specific treatment for the disease; pain medications may reduce symptoms. [1] The virus was discovered in Uganda in 1937, and was first detected in North America in 1999. [1] [3] WNV has occurred in Europe, Africa, Asia, Australia, and North America. [1] In the United States thousands of cases are reported a year, with most occurring in August and September. [4] It can occur in outbreaks of disease. [3] Severe disease may also occur in horses, for which a vaccine is available. [3] A surveillance system in birds is useful for early detection of a potential human outbreak. [3] Contents 1 Signs and symptoms 2 Cause 2.1 Virology 2.2 Transmission 2.2.1 Vertical transmission 2.3 Risk factors 3 Diagnosis 3.1 Differential diagnosis 4 Prevention 4.1 Monitoring and control 5 Treatment 6 Prognosis 7 Epidemiology 7.1 Weather 8 Research 9 References 10 External links Signs and symptoms [ edit ] About 80% of those infected with West Nile virus (WNV) show no symptoms and go unreported. [5] About 20% of infected people develop symptoms. ... Case Reports in Infectious Diseases . 2012 : 1–4. doi : 10.1155/2012/839458 . PMC 3433121 . ... Journal of Experimental Medicine . 203 (1): 35–40. doi : 10.1084/jem.20051970 . ... Vector-Borne and Zoonotic Diseases . 7 (1): 76–85. doi : 10.1089/vbz.2006.0562 . ... "West Nile virus in the New World: appearance, persistence, and adaptation to a new econiche—an opportunity taken". Viral Immunol . 13 (4): 411–4. doi : 10.1089/vim.2000.13.411 .CCR5, ERVK-32, ROBO3, MAVS, DDX58, PLAAT4, IFIT2, ERVK-6, STAT1, SPP1, OAS1, IL1B, IFNB1, RNASEL, CASP8, HLA-DRB1, PELI1, SELENBP1, ARHGEF2, LRRFIP1, NAMPT, TRAIP, RIPK3, SEC14L2, CSF1R, LAMP3, ERVW-1, FOXP3, ZMYND10, DDX56, CCR7, VCP, CDKN2A, IFIH1, DHX58, ZBP1, HAVCR2, PIK3IP1, NLRP3, TNFRSF13C, TRIM6, RBM45, CCR2, ERVK-20, ERVK-18, VAMP8, TNFRSF1A, IFNA1, TNF, IFNA13, HLA-DQA1, IL1A, HLA-C, IL10, IL17A, IL18, IRF3, IRF5, KIR2DL2, KIR3DL1, KIR3DS1, LSAMP, CD180, SMAD4, MMP9, HLA-A, PIK3CA, PIK3CB, PIK3CD, PIK3CG, PZP, GLS, CASP1, SNCA, GEM, DDX3X, TAP1, TLR3, ATF4
-
Mosquito-Borne Disease
Wikipedia
Emergency Medicine Practice . 16 (5): 1–23, quiz 23–4. PMID 25207355 . ^ a b "Diseases that can be Transmitted by Mosquitoes - Minnesota Dept. of Health" . www.health.state.mn.us . ... Clinical Microbiology Reviews . 25 (4): 635–648. doi : 10.1128/CMR.00045-12 . ... "Emerging arboviruses: Why today?" . One Health . 4 : 1–13. doi : 10.1016/j.onehlt.2017.06.001 . ... The Journal of Spinal Cord Medicine . 35 (1): 9–21. doi : 10.1179/2045772311Y.0000000042 . ... Transactions of the Royal Society of Tropical Medicine and Hygiene . 87 (1): 103–105. doi : 10.1016/0035-9203(93)90444-u .
-
Steroid Diabetes
Wikipedia
It is usually, but not always, a transient condition. Contents 1 Cause 2 Mechanism 3 Diagnosis 3.1 Criteria 4 Treatment 5 References Cause [ edit ] The most common glucocorticoids which cause steroid diabetes are prednisolone and dexamethasone given systemically in "pharmacologic doses" for days or weeks. ... Mechanism [ edit ] Glucocorticoids oppose insulin action and stimulate gluconeogenesis , especially in the liver , resulting in a net increase in hepatic glucose output. ... Because it is not unusual for steroid treatment to precipitate type 1 or type 2 diabetes in a person who is already in the process of developing it, it is not always possible to determine whether apparent steroid diabetes will be permanent or will go away when the steroids are finished.
-
Rahman Syndrome
OMIM
Three patients were hypotonic in the neonatal period and 1 was hypertonic. They had similar facial features, including full cheeks, high hairline, and telecanthus. Additional features, each found only in 1 or 2 patients, included kyphoscoliosis, camptodactyly, talipes equinovarus, advanced bone age, dental anomalies, skin nevi, strabismus, astigmatism, and amblyopia. ... The mutations, which were found by whole-exome sequencing and confirmed by Sanger sequencing, occurred de novo in 4 families; parental DNA from the fifth family was not available. ... The truncated proteins were predicted to have a reduced net charge compared to the wildtype protein, rendering them likely to be less effective in neutralizing negatively charged linker DNA. ... INHERITANCE - Autosomal dominant GROWTH Height - Increased birth length - Increased height Weight - Increased birth weight - Increased weight HEAD & NECK Head - Large head circumference Face - Full cheeks Eyes - Telecanthus - Strabismus - Amblyopia - Astigmatism ABDOMEN Gastrointestinal - Poor feeding in the neonatal period SKELETAL - Advanced bone age Spine - Kyphoscoliosis Hands - Camptodactyly Feet - Talipes equinovarus SKIN, NAILS, & HAIR Skin - Nevi MUSCLE, SOFT TISSUES - Hypotonia, neonatal - Hypertonia, neonatal NEUROLOGIC Central Nervous System - Delayed development - Intellectual disability, mild to severe MISCELLANEOUS - Highly variable features - De novo mutation MOLECULAR BASIS - Caused by mutation in the histone gene cluster 1, H1 histone family, member E gene (HIST1H1E, 142220.0001 ) ▲ Close
-
Mutyh Polyposis
GeneReviews
More detailed information for clinicians ordering genetic tests can be found here. Table 1. Germline Molecular Genetic Testing Used in MUTYH Polyposis View in own window Gene 1 Method Proportion of Pathogenic Variants 2 Detectable by Method MUTYH Sequence analysis 3 ~99% 4 Gene-targeted deletion/duplication analysis 5 See footnote 6 1. ... Cancer Risks in Individuals with MUTYH Polyposis Compared to the General Population View in own window Cancer Type General Population Risk 1 Risk Associated with MAP 2 Median Age of Onset Colorectal 5.5% 43%-63% by age 60 yrs; 80%-90% lifetime risk w/out surveillance 48 yrs Duodenal <0.3% 4% 61 yrs Ovarian 1.3% 6%-14% 51 yrs Bladder 1%-4% 6%-8% in females; 6%-25% in males 61 yrs Breast 12% 12%-25% 53 yrs Endometrial 2.9% ~3% 51 yrs Gastric <0.7%-1% 1% 38 yrs Pancreatic 1.6% See footnote 3 Skin ~20% 4 See footnote 3 Thyroid 0.6%-1.8% See footnote 3 1. ... It is unclear if a heterozygous MUTYH pathogenic variant is a risk factor for NET or ACC, as the risk of NET or ACC in individuals with biallelic MUTYH pathogenic variants appears to be quite low. ... Using these figures, the prevalence of 1:20,000 to 1:60,000 for persons with biallelic germline MUTYH pathogenic variants can be derived. ... Recommended Surveillance for Individuals with MUTYH Polyposis View in own window System/Concern Evaluation Frequency Colon Colonoscopy w/polypectomy Every 1-2 yrs beginning at age 25-30 yrs 1, 2 Duodenum/Stomach Upper endoscopy & side viewing duodenoscopy 3 Every 3 mos to 4 yrs beginning at age 30-35 yrs 1, 4 Extraintestinal malignancies Consider annual physical examination 5 ; may consider thyroid ultrasound 5 Annually May consider skin exam by dermatologist 5 One time or annually 1.