Load FindZebra Summary
Disclaimer:
FindZebra Search conducts a search using our specialized medical search engine.
FindZebra Summary uses the text completions API
(subject to OpenAI’s API data usage policies)
to summarize and reason about the search results.
The search is conducted in publicly available information on the Internet that we present “as is”.
You should be aware that FindZebra is not supplying any of the content in the search results.
FindZebra Summary is loading...
-
Combined D-2- And L-2-Hydroxyglutaric Aciduria
OMIM
Description Combined D-2- and L-2-hydroxyglutaric aciduria (D-2-HG and L-2-HG) is an autosomal recessive neurometabolic disorder characterized by neonatal-onset encephalopathy with severe muscular weakness, intractable seizures, respiratory distress, and lack of psychomotor development resulting in early death. ... Laboratory studies showed increased urinary levels of D-2-HG, L-2-HG, and 2-oxoglutaric acid. The patient's younger sister was found to have mildly increased D-2-HG during prenatal testing; L-2-HG was normal. ... Extensive laboratory studies in this patient also showed increased 2-oxoglutaric acid and variably increased D-2-HG and L-2-HG in urine, plasma, and cerebrospinal fluid. ... Organic acid studies showed combined elevation of D-2-HG, L-2-HG, and 2-oxoglutaric acid. An older brother had died of unknown causes on the first day of life. ... Inheritance The transmission pattern of combined D-2-HG and L-2-HG in the families reported by Muntau et al. (2000) was consistent with autosomal recessive inheritance.
-
Hyperemesis Gravidarum
Wikipedia
While most women will experience near-complete relief of morning sickness symptoms near the beginning of their second trimester , some sufferers of HG will experience severe symptoms until they give birth to their baby, and sometimes even after giving birth. [15] A small percentage rarely vomit, but the nausea still causes most (if not all) of the same issues that hyperemesis with vomiting does. [ citation needed ] Causes [ edit ] There are numerous theories regarding the cause of HG, but the cause remains controversial. It is thought that HG is due to a combination of factors which may vary between women and include genetics . [11] Women with family members who had HG are more likely to develop the disease. [16] One factor is an adverse reaction to the hormonal changes of pregnancy, in particular, elevated levels of beta human chorionic gonadotropin (β-hCG). [17] [18] This theory would also explain why hyperemesis gravidarum is most frequently encountered in the first trimester (often around 8–12 weeks of gestation), as β-hCG levels are highest at that time and decline afterward. ... Hematological investigations include hematocrit levels, which are usually raised in HG. [24] An ultrasound scan may be needed to know gestational status and to exclude molar or partial molar pregnancy. [25] Management [ edit ] Dry bland food and oral rehydration are first-line treatments. [26] Due to the potential for severe dehydration and other complications, HG is treated as an emergency. ... Depression and post-traumatic stress disorder [37] are common secondary complications of HG and emotional support can be beneficial. [11] Infant [ edit ] The effects of HG on the fetus are mainly due to electrolyte imbalances caused by HG in the mother. [20] Infants of women with severe hyperemesis who gain less than 7 kilograms (15 lb) during pregnancy tend to be of lower birth weight , small for gestational age , and born before 37 weeks gestation. [12] In contrast, infants of women with hyperemesis who have a pregnancy weight gain of more than 7 kilograms appear similar to infants from uncomplicated pregnancies. [38] There is no significant difference in the neonatal death rate in infants born to mothers with HG compared to infants born to mothers who do not have HG. [11] Children born to mothers with undertreated HG have a fourfold increase in neurobehavioral diagnoses. [39] Epidemiology [ edit ] Vomiting is a common condition affecting about 50% of pregnant women, with another 25% having nausea. [40] However, the incidence of HG is only 0.3–1.5%. [5] After preterm labor, hyperemesis gravidarum is the second most common reason for hospital admission during the first half of pregnancy. [11] Factors, such as infection with Helicobacter pylori , a rise in thyroid hormone production, low age, low body mass index prior to pregnancy, multiple pregnancies, molar pregnancies , and a past history of hyperemesis gravidarum have been associated with the development of HG. [11] History [ edit ] Thalidomide was prescribed for treatment of HG in Europe until it was recognized that thalidomide is teratogenic and is a cause of phocomelia in neonates. [41] Etymology [ edit ] Hyperemesis gravidarum is from the Greek hyper- , meaning excessive, and emesis , meaning vomiting , and the Latin gravidarum , the feminine genitive plural form of an adjective, here used as a noun, meaning "pregnant [woman]". ... ISBN 978-0-674-01343-8 . ^ "Do I Have Morning Sickness or HG?" . H.E.R. Foundation. Archived from the original on 30 November 2012 .
-
High Blood Pressure (Hypertension)
Mayo Clinic
The top number ranges from 120 to 129 mm Hg and the bottom number is below, not above, 80 mm Hg. ... The top number ranges from 130 to 139 mm Hg or the bottom number is between 80 and 89 mm Hg. Stage 2 hypertension. The top number is 140 mm Hg or higher or the bottom number is 90 mm Hg or higher. ... The top number ranges from 120 to 129 mm Hg and the bottom number is below, not above, 80 mm Hg . ... The top number ranges from 130 to 139 mm Hg or the bottom number is between 80 and 89 mm Hg .
-
Iminoglycinuria
OMIM
Early studies of families with iminoglycinuria suggested genetic complexity, with homozygotes developing IG and heterozygotes manifesting only hyperglycinuria (HG; 138500) (summary by Broer et al., 2008). ... These authors, as well as Whelan and Scriver (1968), concluded that iminoglycinuria is the homozygous form of the trait that presents as hyperglycinuria (HG; 138500) in the heterozygote. Genetic heterogeneity in iminoglycinuria was suggested by the facts that only some apparent homozygotes show a defect in intestinal absorption of L-proline (Goodman et al., 1967; Scriver, 1968), and that only some obligate heterozygotes show hyperglycinuria with glycine loading (Scriver, 1968). ... IG was reconfirmed in all but 2 of the probands: in 2 of the Australian families, the probands had only persistent hyperglycinuria (HG; 138500). Broer et al. (2008) sequenced 5 known imino acid and glycine transporter candidates and found that the main contribution to IG and HG arose from defects in the gene encoding the proton amino acid transporter SLC36A2 (608331.0001-608331.0002), with a classic semidominant inheritance pattern in which 2 nonfunctional alleles conferred the IG phenotype whereas 1 nonfunctional allele was sufficient to confer the HG phenotype. ... Broer et al. (2008) noted that additional polymorphisms and mutations were identified in the gene encoding the putative glycine transporter SLC6A18 (610300) in these affected individuals, and suggested that variation in SLC6A18 might also contribute to these phenotypes. Thus, IG and HG exhibit complex molecular explanations depending on a major gene and accompanying modifier genes.
-
Hyperglycinuria
OMIM
Early studies of families with iminoglycinuria suggested genetic complexity, with homozygotes developing IG and heterozygotes manifesting only hyperglycinuria (HG) (summary by Broer et al., 2008). ... IG was reconfirmed in all but 2 of the probands: in 2 of the Australian families, the probands had only persistent hyperglycinuria (HG). Broer et al. (2008) sequenced 5 known imino acid and glycine transporter candidates and found that the main contribution to IG and HG arose from defects in the gene encoding the proton amino acid transporter SLC36A2 (608331.0001 and 608331.0002), with a classic semidominant inheritance pattern in which 2 nonfunctional alleles conferred the IG phenotype whereas 1 nonfunctional allele was sufficient to confer the HG phenotype. Broer et al. (2008) noted that additional polymorphisms and mutations were identified in the affected individuals in the genes encoding the imino acid transporter SLC6A20 (605616), the putative glycine transporter SLC6A18 (610300), and the neutral amino acid transporter SLC6A19 (608893), and suggested that variation in these genes might also contribute to these phenotypes. Thus, IG and HG exhibit complex molecular explanations depending on a major gene and accompanying modifier genes.
-
Elevated Blood Pressure
Mayo Clinic
Blood pressure is 120/80 millimeters of mercury (mm Hg) or lower. Elevated blood pressure. The top number ranges from 120 to 129 mm Hg and the bottom number is below (not above) 80 mm Hg . ... The top number ranges from 130 to 139 mm Hg or the bottom number is between 80 to 89 mm Hg . Stage 2 hypertension. The top number is 140 mm Hg or higher or the bottom number is 90 mm Hg or higher. ... Elevated blood pressure is a measurement of 120 to 129 millimeters of mercury (mm Hg) and a bottom number below (not above) 80 mm Hg .
-
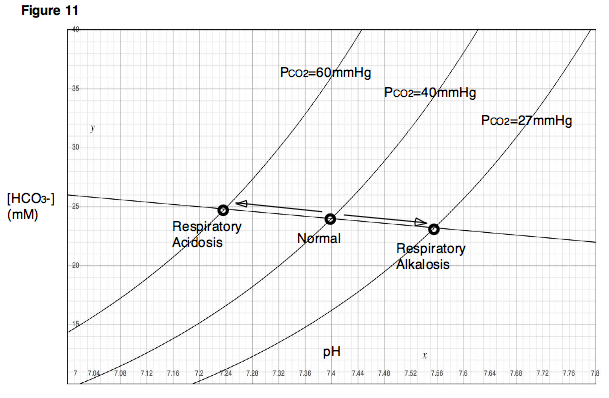
Respiratory Acidosis
Wikipedia
In acute respiratory acidosis , the Pa CO 2 is elevated above the upper limit of the reference range (over 6.3 kPa or 45 mm Hg) with an accompanying acidemia (pH <7.36). ... The Pa CO 2 is maintained within a range of 35–45 mm Hg in normal states. Alveolar ventilation is under the control of the respiratory center , which is located in the pons and the medulla . ... Cellular buffering elevates plasma bicarbonate (HCO 3 − ) only slightly, approximately 1 mEq/L for each 10-mm Hg increase in Pa CO 2 . The second step is renal compensation that occurs over 3–5 days. ... For instance, PEPCK is upregulated in renal proximal tubule brush border cells , in order to secrete more NH 3 and thus to produce more HCO 3 − . [1] Estimated changes [ edit ] In renal compensation, plasma bicarbonate rises 3.5 mEq/L for each increase of 10 mm Hg in Pa CO 2 . The expected change in serum bicarbonate concentration in respiratory acidosis can be estimated as follows: Acute respiratory acidosis: HCO 3 − increases 1 mEq/L for each 10 mm Hg rise in Pa CO 2 . Chronic respiratory acidosis: HCO 3 − rises 3.5 mEq/L for each 10 mm Hg rise in Pa CO 2 . The expected change in pH with respiratory acidosis can be estimated with the following equations: Acute respiratory acidosis: Change in pH = 0.08 X ((40 − Pa CO 2 )/10) Chronic respiratory acidosis: Change in pH = 0.03 X ((40 − Pa CO 2 )/10) Respiratory acidosis does not have a great effect on electrolyte levels.
-
Ischiopatellar Dysplasia
Wikipedia
. ^ Bongers EM, Duijf PH, van Beersum SE, Schoots J, Van Kampen A, Burckhardt A, Hamel BC, Losan F, Hoefsloot LH, Yntema HG, Knoers NV, van Bokhoven H. Mutations in the human TBX4 gene cause small patella syndrome. ... J Bone Joint Surg Br. 1979;61:172–175. ^ Bongers EM, Duijf PH, van Beersum SE, Schoots J, Van Kampen A, Burckhardt A, Hamel BC, Losan F, Hoefsloot LH, Yntema HG, Knoers NV, van Bokhoven H. Mutations in the human TBX4 gene cause small patella syndrome. ... Am J Med Genet. 1995;57:558–561. ^ Bongers EM, Duijf PH, van Beersum SE, Schoots J, Van Kampen A, Burckhardt A, Hamel BC, Losan F, Hoefsloot LH, Yntema HG, Knoers NV, van Bokhoven H. Mutations in the human TBX4 gene cause small patella syndrome. ... Z Orthop 1988;126:22–29. ^ Bongers EM, Duijf PH, van Beersum SE, Schoots J, Van Kampen A, Burckhardt A, Hamel BC, Losan F, Hoefsloot LH, Yntema HG, Knoers NV, van Bokhoven H. Mutations in the human TBX4 gene cause small patella syndrome. ... J Bone Joint Surg Br. 1979;61:172–175. ^ Bongers EM, Duijf PH, van Beersum SE, Schoots J, Van Kampen A, Burckhardt A, Hamel BC, Losan F, Hoefsloot LH, Yntema HG, Knoers NV, van Bokhoven H. Mutations in the human TBX4 gene cause small patella syndrome.
-
D-2-Hydroxyglutaric Aciduria
Orphanet
D-2-hydroxyglutaric aciduria (D-2-HGA) is a rare clinically variable neurological form of 2-hydroxyglutaric aciduria (see this term) characterized biochemically by elevated D-2-hydroxyglutaric acid (D-2-HG) in the urine, plasma and cerebrospinal fluid. ... Developmental delay and hypotonia are the most common findings. No correlation between D-2-HG levels and clinical symptoms has been found. Some patients with elevated D-2-HG levels are asymptomatic. In general, D-2-hydroxygluratic aciduria caused by heterozygous IDH2 mutations, has a more severe clinical course than D-2-hydroxygluratic aciduria caused by mutations in the D2HGDH gene.
-
Glaucoma 1, Open Angle, H
OMIM
The maximum intraocular pressure values varied from moderate (24 mm Hg) to high (60 mm Hg). Those affected had optic nerve damage varying from early to late stages, with cup-disc ratios of up to 0.9 and significant glaucomatous visual field loss.
-
Glaucoma 1, Open Angle, P
OMIM
POAG that occurs with an IOP below an arbitrary threshold of 21 mm Hg is often termed 'normal tension glaucoma' (summary by Fingert et al., 2011). ... Five of the 6 affected family members with extensive ophthalmologic records had a maximum IOP of 21 mm Hg or less and met criteria for a diagnosis of normal tension glaucoma, whereas 1 patient had a maximum IOP of 22 mm Hg. ... One was a sporadic NTG patient with a maximum IOP of 20 mm Hg and a 300-kb duplication. The other patient, who had a 650-kb duplication, came from an NTG family previously described by Bennett et al. (1989); DNA was available from 3 additional affected members, who all carried the duplication, whereas it was not found in 3 unaffected family members. ... Using quantitative PCR, Kawase et al. (2012) analyzed 252 unrelated Japanese NTG patients who had open angle glaucoma and maximum untreated IOPs of 21 mm Hg or less, 202 Japanese controls, 29 NTG patients from North Carolina, and 28 NTG patients from New York.
-
Pulmonic Stenosis
Wikipedia
Treatment [ edit ] The treatment of choice is percutaneous balloon valvuloplasty and is done when a resting peak gradient is seen to be >60mm Hg or a mean >40mm Hg is observed. References [ edit ] Ren (Jul. 15, 2009).PTPN11, JAG1, SOS1, NF1, BRAF, ELN, IGFBP7, TAB2, MRAS, B4GALT7, POLR3A, PRDM5, SEMA3E, FBLN5, SCO2, WASHC5, ZEB2, CHST3, GTF2IRD1, NRXN1, SMC3, PIGQ, BAZ1B, DCHS1, CDK13, USP9X, LZTR1, SHOC2, NDUFAF3, TBL2, CNTNAP2, FAT4, NEK8, KANSL1, B3GLCT, ZNF526, G6PC3, NEK9, ZNF469, RNF135, TRAF7, ADAMTS10, STRA6, CLIP2, ARHGAP31, CHD7, BCOR, TMCO1, WNT4, RAB23, MLXIPL, EFEMP2, CCDC22, ACAD8, ZIC3, MAP3K7, NDUFS2, GDF1, NDUFB8, MGP, SMAD3, LTBP2, LIMK1, KRAS, HRAS, GTF2I, GPC3, GATA6, NOTCH1, GPC4, FKTN, FBN1, BPTF, SARDH, DHCR7, CYP24A1, CDC42, BMP2, TTN, TTN-AS1, NOTCH2, SOS2, RIT1, RFC2, STIM1, NRAS, RAF1, RAD21, ALDH18A1, PSMD12, MAP2K2, MAP2K1, PPP1CB, PMM2, ENPP1, SURF1, TBX2, RPL27, GATA4, EPHA2, STAT3, GALNT1, PDK1, ARSD, ROR2, VWF
-
Systolic Hypertension
Wikipedia
Clinical trials have also documented the beneficial effects of weight loss, increased physical activity, and limiting alcohol consumption. [3] In addition to lifestyle changes, medication can also be used to reduce systolic hypertension to safe levels. [4] [5] Goal [ edit ] Based on these studies, treating to a systolic blood pressure of 140, as long as the diastolic blood pressure is 68 or more, seems safe. [ citation needed ] Corroborating this, a reanalysis of the SHEP data suggests allowing the diastolic to go below 70 may increase adverse effects. [6] A meta-analysis of individual patient data from randomized controlled trials found the lowest diastolic blood pressure for which cardiovascular outcomes improve is 85 mm Hg for untreated hypertensives and 80 mm Hg for treated hypertensives. [7] The authors concluded "poor health conditions leading to low blood pressure and an increased risk for death probably explain the J-shaped curve". [7] Interpreting the meta-analysis is difficult, but avoiding a diastolic blood pressure below 68–70 mm Hg seems reasonable because: The low value of 85 mm Hg for treated hypertensives in the meta-analysis is higher than the value of 68–70 mm Hg that is suggested by the two major randomized controlled trials of isolated systolic hypertension The two largest trials in the meta-analysis, Hypertension Detection and Follow-up Program (HDFP) [8] and Medical Research Council trial in mild hypertension (MRC1) [9] were predominantly middle-aged subjects, all of whom had diastolic hypertension before treatment.
-
Complicated Grief Disorder
Wikipedia
PMID 16477190 . S2CID 8995920 . ^ Prigerson HG, Shear MK, Bierhals AJ, Pilkonis PA, Wolfson L, Hall M, Zonarich DL, Reynolds III CF (1997). ... Retrieved 2017-09-23 . ^ Prigerson HG, Bierhals AJ, Kasl SV, Reynolds CF, Shear MK, Day N, Beery LC, Newsom JT, Jacobs S (May 1997). ... PMID 9137115 . ^ Chen JH, Bierhals AJ, Prigerson HG, Kasl SV, Mazure CM, Jacobs S (March 1999). ... S2CID 23836831 . ^ Lannen PK, Wolfe J, Prigerson HG, Onelov E, Kreicbergs UC (December 2008). ... J Trauma Stress 2010, in press. ^ Mitchell AM, Kim Y, Prigerson HG, Mortimer-Stephens M. Complicated grief in survivors of suicide.
-
Hypertension, Diastolic, Resistance To
OMIM
The age- and sex-adjusted ORs for K carriers with diastolic blood pressures greater than or equal to 105 mm Hg and 110 mm Hg were 0.39 (95% CI, 0.17-0.93, p = 0.034) and 0.12 (95% CI, 0.02-0.90, p = 0.039), respectively.
-
Muscle Dysmorphia
Wikipedia
. ^ a b American Psychiatric Association, "Body dysmorphic disorder" , Diagnostic and Statistical Manual of Mental Disorders , Fifth Edition (Arlington, VA: American Psychiatric Association, 2013). ^ a b c d e Pope HG Jr, Gruber AJ, Choi P, Olivardia R & Phillips KA (1997), "Muscle dysmorphia: An underrecognized form of body dysmorphic disorder", Psychosomatics: Journal of Consultation and Liaison Psychiatry 38 (6):548–557. ^ Mosley PE (2009). ... PMID 18759381 . ^ a b Cafri G, Olivardia R & Thompson JK (2008), "Symptom characteristics and psychiatric comorbidity among males with muscle dysmorphia", Comprehensive Psychiatry 49 (4):374–379. ^ a b Pope CG, Pope HG, Menard W, Fay C, Olivardia R, & Phillips KA (2005), "Clinical features of muscle dysmorphia among males with body dysmorphic disorder: Body Image 2 (4):395–400. ^ a b Hitzeroth V, Wessels C, Zungu-Dirwayi N, Oosthuizen P, & Stein DJ (2001), "Muscle dysmorphia: A South African sample", Psychiatry and Clinical Neurosciences 55 (5):521–523. ^ a b c Gruber AJ & Pope HG (1999), "Compulsive weight lifting and anabolic drug abuse among women rape victims", Comprehensive Psychiatry 40 (4):273–277. ^ Edwards C, Molnar G & Tod D (2017), "Searching for masculine capital: Experiences leading to high drive for muscularity in men" , Psychology of Men & Masculinity 18 (4)"361–371.' ^ a b Olivardia R (2001), "Mirror, mirror on the wall, who's the largest of them all? the features and phenomenology of muscle dysmorphia", Harvard Review of Psychiatry 9 (5):254–259. ^ a b c d e Grieve FG (2007), "A conceptual model of factors contributing to the development of muscle dysmorphia", Eating Disorders: The Journal of Treatment & Prevention 15 (1):63–80. ^ a b Cohane GH, & Pope HG Jr (2001), "Body image in boys: A review of the literature", International Journal of Eating Disorders 29 (4):373–379. ^ Mangweth B, Pope HGJ, Kemmler G, Ebenbichler C, Hausmann A, et al. (2001), "Body image and psychopathology in male bodybuilders", Psychotherapy and Psychosomatics 70 (1):38–43. ^ Pope HG Jr, Olivardia R, Borowiecki JJ 3rd & Cohane GH (2001), "The growing commercial value of the male body: A longitudinal survey of advertising in women's magazines" , Psychotherapy and Psychosomatics 70 (4):189–192. ^ Leit RA, Pope HG Jr, & Gray JJ (2001), "Cultural expectations of muscularity in men: The evolution of playgirl centerfolds", International Journal of Eating Disorders 29 (1):90–93. ^ Leit RA, Gray JJ, & Pope HG Jr (2002), "The media's representation of the ideal male body: A cause for muscle dysmorphia?", International Journal of Eating Disorders 31 (3):334–338. ^ Daniel S & Bridges SK (2010)m The drive for muscularity in men: Media influences and objectification theory, Body Image 7 (1):32–38. ^ Parent MC & Moradi B (2011), "His biceps become him: A test of objectification theory's application to drive for muscularity and propensity for steroid use in college men", Journal of Counseling Psychology 58 (2):246–256. ^ Davis C & Cowles M (1991), "Body image and exercise: A study of relationships and comparisons between physically active men and women", Sex Roles 25 (1–2):33–44. ^ Chung B (2001), "Muscle dysmorphia: A critical review of the proposed criteria" , Perspect Biol Med 44 (4):565–574. ^ a b dos Santos Filho CA, Tirico PP, Stefano SC, Touyz SW & Claudino AM (2016), "Systematic review of the diagnostic category muscle dysmorphia", Australian and New Zealand Journal of Psychiatry 50 (4):322–333. ^ Ung EK, Fones CS, & Ang AW (2000), Muscle dysmorphia in a young Chinese male, Annals of the Academy of Medicine (Singapore) 29 (1):135–137. ^ Soler PT, Fernandes HM, Damasceno VO, et al. (2013), "Vigorexy and levels of exercise dependence in gym goers and bodybuilders", Revista Brasileira de Medicina do Esporte 19 (5):343–348. ^ Rutsztein G, Casguet A, Leonardelli E, López P, Macchi M, Marola ME & Redondo G (2004), "Imagen corporal en hombres y su relación con la dismorfia muscular", Revista Argentina De Clínica Psicológica 13 (2):119–131. ^ a b Behar R & Molinari D (2010), "Muscle dysmorphia, body image and eating behaviors in two male populations", Revista Médica de Chile 138 (11):1386–1394. ^ Yang CJ, Gray P, & Pope HG Jr, (2005), "Male body image in Taiwan versus the west: Yanggang Ahiqi meets the Adonis complex", The American Journal of Psychiatry 162 (2):263–269. ^ a b Pope HG, Katz DL & Hudson JI (1993), "Anorexia nervosa and 'reverse anorexia' among 108 male bodybuilders", Comprehensive Psychiatry 34 (6):406–409. ^ a b Griffiths S, Mond JM, Murray SB & Touyz S (2015), "Positive beliefs about anorexia nervosa and muscle dysmorphia are associated with eating disorder symptomatology", Australian and New Zealand Journal of Psychiatry 49 (9):812–820. ^ a b c Murray SB & Touyz SW (2013), "Muscle dysmorphia: Towards a diagnostic consensus", Australian and New Zealand Journal of Psychiatry 47 (3):206–207. ^ a b Russell J (2013), Commentary on: "Muscle Dysmorphia: Towards a diagnostic consensus".
-
Low Blood Pressure (Hypotension)
Mayo Clinic
Overview Low blood pressure is generally considered a blood pressure reading lower than 90 millimeters of mercury (mm Hg) for the top number (systolic) or 60 mm Hg for the bottom number (diastolic). ... A sudden fall in blood pressure can be dangerous. A change of just 20 mm Hg — a drop from 110 mm Hg systolic to 90 mm Hg systolic, for example — can cause dizziness and fainting. ... A blood pressure measurement is given in millimeters of mercury (mm Hg). It has two numbers: Systolic pressure. ... An ideal blood pressure is usually lower than 120/80 mm Hg . Blood pressure varies throughout the day, depending on: Body position Breathing Food and drink Medications Physical condition Stress Time of day Blood pressure is usually lowest at night and rises sharply on waking.
-
Nutcracker Esophagus
Wikipedia
The Castell criteria include one major criterion: a mean peristaltic amplitude in the distal esophagus of more than 180 mm Hg. The minor criterion is the presence of repetitive contractions (meaning two or more) that are greater than six seconds in duration. Castell also noted that the lower esophageal sphincter relaxes normally in nutcracker esophagus, but has an elevated pressure of greater than 40 mm Hg at baseline. [2] [9] [10] [11] Three other criteria for definition of the nutcracker esophagus have been defined. The Gothenburg criterion consists of the presence of peristaltic contractions, with an amplitude of 180 mm Hg at any place in the esophagus. [7] [11] The Richter criterion involves the presence of peristaltic contractions with an amplitude of greater than 180 mm Hg from an average of measurements taken 3 and 8 cm above the lower esophageal sphincter. It has been incorporated into a number of clinical guidelines for the evaluation of dysphagia. [11] The Achem criteria are more stringent, and are an extension of the study of 93 patients used by Richter and Castell in the development of their criteria, and require amplitudes of greater than 199 mm Hg at 3 cm above the lower esophageal sphincter (LES), greater than 172 mm Hg at 8 cm above the LES, or greater than 102 mm Hg at 13 cm above the LES. [11] [12] Pathophysiology [ edit ] Pathology specimens of the esophagus in patients with nutcracker esophagus show no significant abnormality, unlike patients with achalasia , where destruction of the Auerbach's plexus is seen.
-
Hypomagnesemia, Hypertension, And Hypercholesterolemia, Mitochondrial
OMIM
Including the index case, 38 members had hypertension (blood pressure greater than 140/90 mm Hg or on treatment for hypertension), 33 had hypercholesterolemia (with total cholesterol greater than 200 mg/dl or on treatment for hypercholesterolemia), and 32 had clinically significant hypomagnesemia (range 0.8 to 1.7 mg/dl, normal 1.8 to 2.5 mg/dl). ... Among adults age 18 to 60, maternal lineage increased systolic blood pressure by an average of 13 mm Hg and diastolic blood pressure by 5 mm Hg.
-
Normal Tension Glaucoma
Wikipedia
Contents 1 Clinical relevance 2 Risk factors 3 Diagnosis 4 Treatment 5 References Clinical relevance [ edit ] Over many years, glaucoma has been defined by an intraocular pressure of more than 20 mm Hg. Incompatible with this (now obsolete) definition of glaucoma was the ever larger number of cases that have been reported in medical literature in the 1980s and 1990s who had the typical signs of glaucomatous damage, like optic nerve head excavation and thinning of the retinal nerve fiber layer, while these patients had an IOP that would generally have been regarded as "normal". ... Among Americans of Japanese descent , for instance, the prevalence of NTG is about four times as high as the prevalence of the "classical glaucoma" with an IOP of 22 mm Hg and higher. The pillar of the current understanding of normal tension glaucoma is a reduced IOP tolerance of the retinal ganglion cells and the cells in the optic nerve head - an IOP of, for example, 17 or 19 mm Hg that would not affect a healthy eye leads to damage in the eye of an NTG patient. [1] Risk factors [ edit ] In many patients, normal tension glaucoma is common in individuals with a generalized reduced perfusion of organs and certain body tissues.SLC1A1, SLC1A3, HSPD1, SOD1, CDKN2B-AS1, TBK1, OPA1, OPTN, ZFPM2, TMEM263, MYOC, TLR4, CDKN2B, MTHFR, NCK2, SIX1, ATOH7, WDR36, NOS3, APOE, SRBD1, EDNRA, EDN1, ELOVL5, PLXNA2, SIX6, TANK, SHBG, TNF, SELENBP1, LOXL1, CCHCR1, ASB10, MMP9, GLC1P, LAMC2, CSF2, HK2, CAV2, ARHGEF12, DOCK3, OPTC, CYP1B1, AZI2, TRMO, CYBA, XPOT, PARL, MFN1, RPGRIP1, CHEK2, HSPA14, FNDC3B, VAV3, AGBL2, NAA25, PLXDC2, MVB12B, CAV1, OPN4, GLCCI1, AKR1B1, AKT1, TMTC2, AGTR2, TAB3, RASSF3, ADRB1, NCKAP1, EDNRB, CXCL8, GNS, MMP14, IL6, IL1B, NAP1L1, ICA1, HSPA1B, HSPA1A, HLA-DRB1, PTEN, PTPRJ, REN, CCL2, HLA-DQB1, ABO, GLC1B, EPO, SOD2, TLR2, GALC, MTOR, TP53, FDXR, GAS7, SQSTM1, ESR2, DCLK1, NAPSA, TBKBP1, MFN2, ACOT8, ABCA1