Load FindZebra Summary
Disclaimer:
FindZebra Search conducts a search using our specialized medical search engine.
FindZebra Summary uses the text completions API
(subject to OpenAI’s API data usage policies)
to summarize and reason about the search results.
The search is conducted in publicly available information on the Internet that we present “as is”.
You should be aware that FindZebra is not supplying any of the content in the search results.
FindZebra Summary is loading...
-
Human Papillomavirus Infection
Wikipedia
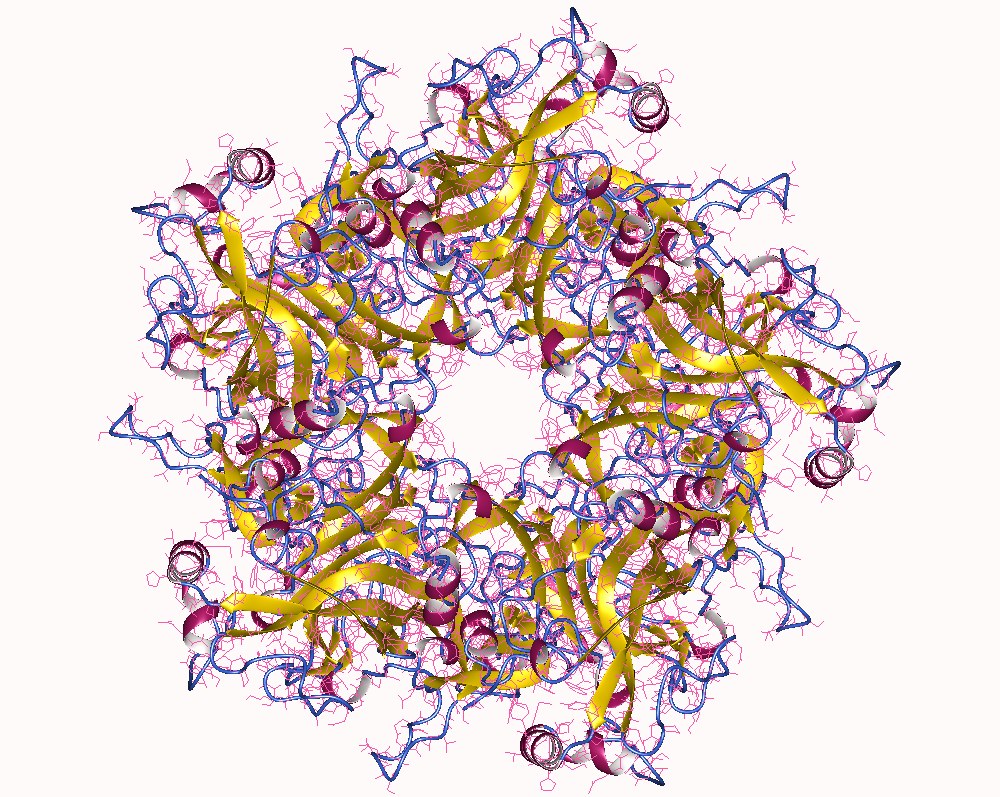
Rendered from PDB : 4GIZ . [106] The two primary oncoproteins of high risk HPV types are E6 and E7. The “E” designation indicates that these two proteins are early proteins (expressed early in the HPV life cycle), while the "L" designation indicates that they are late proteins (late expression). [46] The HPV genome is composed of six early (E1, E2, E4, E5, E6, and E7) open reading frames (ORF), two late (L1 and L2) ORFs, and a non-coding long control region (LCR). [107] After the host cell is infected viral early promoter is activated and a polycistronic primary RNA containing all six early ORFs is transcribed. This polycistronic RNA then undergoes active RNA splicing to generate multiple isoforms of mRNAs . [108] One of the spliced isoform RNAs, E6*I, serves as an E7 mRNA to translate E7 protein. [109] However, viral early transcription subjects to viral E2 regulation and high E2 levels repress the transcription. HPV genomes integrate into host genome by disruption of E2 ORF, preventing E2 repression on E6 and E7. Thus, viral genome integration into host DNA genome increases E6 and E7 expression to promote cellular proliferation and the chance of malignancy. The degree to which E6 and E7 are expressed is correlated with the type of cervical lesion that can ultimately develop. [101] Role in cancer The E6/E7 proteins inactivate two tumor suppressor proteins, p53 (inactivated by E6) and pRb (inactivated by E7). [110] The viral oncogenes E6 and E7 [111] are thought to modify the cell cycle so as to retain the differentiating host keratinocyte in a state that is favourable to the amplification of viral genome replication and consequent late gene expression.CASP8, VAMP7, CCNA1, TP53, IL10, PDXP, HLA-DRB1, CDKN2A, H3P10, HLA-G, EGFR, TLR9, GSTM1, TNF, RASSF1, BCL2, CCND1, MDM2, RBM45, IL6, MBL2, FHIT, TMC8, PSMA1, SLPI, PIK3CA, KRAS, SERPIND1, SULT2A1, CYCSP38, ZAP70, IL17A, REG3A, PDAP1, MIR21, FOXP3, BRAF, HLA-DQB1, ESR1, GSTT1, TERT, APOBEC3B, ASAP1, CD274, MTPAP, MKI67, HLA-C, PYCARD, ACP3, PIK3CB, PIK3CD, STIL, STS, ASAP2, MRPS30, PAPOLA, PIK3CG, PMEL, TERC, TGFB1, TUSC2, SEC14L2, SH3GL2, USO1, STAT3, TP73, MIB1, MGMT, PTEN, NXF1, PTGS2, IFNA1, MLH1, IFNA13, IL1B, PGR, PAX1, TMC6, HPGDS, MTHFR, FLNB, CXCL8, ERBB2, CDKN1A, ARHGAP24, AKT1, ANXA2, CTNNB1, MIR34A, MRC1, PCNA, CDH1, NT5E, NFKB1, GORASP1, COX2, WNK1, SMUG1, MALAT1, KRT19, CYP1A1, KIR3DL1, DAPK1, JUN, IL18, DEFB1, CCR5, CD68, IL2, PML, HSP90B1, XRCC1, MTCO2P12, TLR4, TLR3, CXCR4, SYT1, APC, RHOH, DEFB4B, HSPB3, CD163, CCL2, RELA, CCR2, CALR, PSMB8, TLR7, VEGFA, DEFB4A, FOSL2, HLA-E, HSPB2, GEM, HLA-DQB2, HLA-DQA1, GNAO1, SLC12A9, FGFR2, HRAS, HSPB1, MEG3, HGF, FGFR4, DOCK8, PDLIM7, ARTN, CD83, VTCN1, PLAA, RHBDL1, MTA1, ISG15, NCR1, AIM2, GGTLC4P, ZNF516, PPIP5K1, PDCD6IP, KIF20A, B3GNT3, YAP1, HOXB13, TCHP, CIB1, ZNRD2, LIMD1, INTS2, CEMIP, MIR944, VIM, WNT11, H3P23, LOC110806263, CLSPN, RINT1, APOBEC3G, LOC102723971, RBM25, DEK, TFPI2, THRIL, NR0B2, CIP2A, CUL2, IFNL4, TP63, ARRDC3, SOCS1, COMMD3-BMI1, BECN1, MICA, CFLAR, FCGBP, ARHGEF7, MAGI2-AS3, TMED7-TICAM2, GGT2, TNRC6C-AS1, SPINT2, RETN, GGTLC3, LYPD5, IL17RA, BRMS1, ATAD3A, PPP1R14B, HSPB6, MLH3, TICAM2, SALL3, DHDH, PGPEP1, STING1, DGCR8, EVC2, IL19, MIRLET7C, IFNL3, DEFB104A, OR2AG1, ASCC1, TMED7, RBMX2, METTL9, PLCE1, REV1, APOBEC3A, MARVELD2, UVRAG, WT1-AS, PISD, MIR122, DCTN6, MIR27A, GGTLC5P, TLR8, MIR363, RNPS1, BTG3, IL33, DEFB104B, LINC01191, MIR93, RAB40B, CKAP4, SLC52A3, MIR30C2, CHEK2, AMACR, ANTXR2, POLI, ZNF395, MIR203A, DNAJA4, MIR146A, SMG1, MYCBP2, LPIN1, RRS1, BRD4, MTREX, MIR126, MIR145, S100A10, TYMS, FUS, FOSB, FOS, FLG, FOXC2, FGFR1, FGF3, PTK2B, ERBB4, ERBB3, EP300, ENO1, E2F1, DUT, DPH1, DNMT3B, DNMT1, NQO1, MTOR, GGT1, TSG101, GHRHR, IGFBP3, IFNG, IFNB1, IFNA2, IFI27, IFI16, ID1, TNC, HSPD1, HOXB2, HMGB1, HLA-A, GSTP1, GSTM2, SFN, GNAS, CBLIF, AKR1C1, DCT, CYP2E1, CYP1B1, CA2, PTTG1IP, BUB1B, BMI1, BAX, BAG1, ATR, ATM, FAS, ANXA5, ANXA3, JAG1, AGRP, AGER, AGA, PARP1, ADH1C, CA9, SLC25A20, CAV1, CDKN2B, CTSB, CSF2, CRP, CLCN3, CHEK1, CFTR, CDKN3, CDKN1B, ENTPD1, CDK9, CDK6, CDK4, CDC25A, CDK1, CD63, CD40, IL1A, IL4, CXCL10, PTPN11, SDCBP, SDC1, CCL22, CCL20, CCL11, CCL5, SERPINB4, SERPINB3, S100B, ACTG1, S100A1, RRBP1, RPE65, RP9, RNASEL, RB1, RARA, CXCL12, SELE, SRSF2, TDO2, TPT1, TNFRSF1B, TLR2, TIMP3, TIAM1, THBS1, TFRC, TAP2, SOS2, TAP1, SYK, STK11, ST2, SPP1, SPARC, SOX2, MOK, PTPN6, ITGA6, PTHLH, MMP8, MMP2, CXCL9, MIF, MGP, MFGE8, MCL1, SMAD3, LIG4, LCN2, STMN1, KLRD1, KLRC2, KIT, CD82, JUND, JUNB, MMP9, MMP11, MMP12, SERPINB2, PTCH1, PSMD9, PSMB9, PRNP, POLD1, PEG3, PECAM1, OGG1, MPG, NFKBIA, NELL1, MYC, MUTYH, MT2A, MSH2, MRE11, H3P40
-
Hpv-Positive Oropharyngeal Cancer
Wikipedia
Its genome encodes the early (E) oncoproteins E5, E6 and E7 and the late (L) capsid proteins L1 and L2. ... Relative to HPV-OPC, the oncogenic molecular progression of HPV+OPC is poorly understood. [28] The two main viral oncoproteins of the high risk HPV types are E6 and E7. These are consistently expressed in malignant cell lines, and if their expression is inhibited the malignant phenotype of the cancer cells is blocked. ... Like most HPV+ cancers, HPV+OPC express p16 but the latter does not function as a tumour-suppressor, because the mechanism by which this is achieved, pRb, has been inactivated by E7. p16 is upregulated (over-expressed) due to E7-related loss of pRB with reduced negative feedback, [39] [42] whereas it is downregulated in up to 90% of HPV-OPC. [43] This diffuse over-expression in the tumour cells provides a diagnostic marker for HPV involvement. [44] [45] Although HPV E6 and E7 reduce tumour suppressor activity, they do so less than genetic and epigenetic processes do in HPV-OPC. [46] [47] [11] The tonsillar epithelia ( palatine and lingual ) share similar nonkeratinization characteristics with the cervix , where HPV infection plays the major role in cases of cervical cancer . [14] [48] Also E6 and E7 may make HPV+OPC more immunogenic than HPV-OPC, since anti-E6 and E7 antibodies may be detected in these patients. ... This implies a role for an adaptive immune system in suppressing tumour progression . [90] [91] [89] Surgery [ edit ] Historically, surgery provided the single approach to head and neck cancer. ... In early stage disease, including involvement of neck nodes, TORS produces a 2-year survival of 80–90%. [105] TLM similarly, is reported to have a five-year survival of 78% and local control rates of 85–97%. [106] [107] In addition to early disease, minimally invasive surgery has been used in advanced cases, with up to 90% local control and disease specific survival. [94] [107] Postoperative swallowing was excellent in 87%, but long term dysphagia was associated with larger (T4) cancers, especially if involving the base of the tongue. [107] [12] The details of the surgical approach depend on the location and size of the primary tumour and its N stage.
-
Purple Glove Syndrome
Wikipedia
The American Journal of Emergency Medicine . 33 (1): 123.e5–123.e6. doi : 10.1016/j.ajem.2014.05.039 .
-
Iatrogenic Calcinosis Cutis
Wikipedia
New England Journal of Medicine . 356 (6): e5. doi : 10.1056/NEJMicm055763 . PMID 17287472 .
-
Immunodeficiency 26
Wikipedia
J Allergy Clin Immunol 135(6):1578-1588.e5. doi: 10.1016/j.jaci.2015.01.040. ^ Woodbine L, Neal JA, Sasi, N-K, Shimada M, Deem K, Coleman H, Dobyns WB, Ogi T, Meek K, Davies EG, Jeggo PA (2013) PRKDC mutations in a SCID patient with profound neurological abnormalities. J Clin Invest 123: 2969-2980 ^ van der Burg M, Ijspeert H, Verkaik NS, Turul T, Wiegant WW, Morotomi-Yano K, Mari, P-O, Tezcan I, Chen, DJ, Zdzienicka MZ, van Dongen JJM, van Gent DC (2009) A DNA-PKCS mutation in a radiosensitive T-B- SCID patient inhibits Artemis activation and nonhomologous end-joining. J Clin Invest 119: 91-98
-
Pulmonary Capillary Hemangiomatosis
Wikipedia
Pathol Res Pract . 192 (3): 290–5, discussion 296–9. doi : 10.1016/S0344-0338(96)80232-9 . PMID 8739476 . ^ El-Gabaly M, Farver CF, Budev MA, Mohammed TL (2007). ... The American Journal of Surgical Pathology . 30 (7): 850–857. doi : 10.1097/01.pas.0000209834.69972.e5 . PMID 16819327 . S2CID 25595167 . ^ Chaisson NF, Dodson MW, Elliott CG (2016) Pulmonary Capillary Hemangiomatosis and Pulmonary Veno-occlusive Disease. ... Chest 151(4):821-828 ^ Park MA, Shin SY, Kim YJ, Park MJ, Lee SH (2017) Vascular Ehlers-Danlos syndrome with cryptorchidism, recurrent pneumothorax, and pulmonary capillary hemangiomatosis-like foci: A case report.Medicine (Baltimore) 96(47):e8853 ^ Diao XL, Mu XD, Jin ML (2017) Pulmonary capillary hemangiomatosis associated with CREST syndrome: A challenge of diagnosis and treatment. ... Adv Respir Med 86(3) ^ Sposito Cavallo SL, Macias Sobrino LA, Marenco Altamar LJ, Mejía Alquichire AF (2017) Congenital pulmonary capillary hemangiomatosis in a newborn.
-
The Great Imitator
Wikipedia
The American Journal of Medicine . 123 (7): e5. doi : 10.1016/j.amjmed.2009.12.027 . PMID 20609673 . ^ Sharma, GV; Sasahara, AA; McIntyre, KM (1976). "Pulmonary embolism: The great imitator".
-
Proximal Renal Tubular Acidosis
Wikipedia
A defect in bicarbonate reabsorption with normal urinary acidification" . Pediatr. Res . 1 (2): 81–98. doi : 10.1203/00006450-196703000-00001 . ... Journal of the American Society of Nephrology . 13 (8): 2160–2170. doi : 10.1097/01.ASN.0000023430.92674.E5 . ISSN 1046-6673 . PMID 12138150 . ^ Gahl WA, Thoene JG, Schneider JA (2002). ... Nephrol . 13 (8): 2160–70. doi : 10.1097/01.ASN.0000023430.92674.E5 . PMID 12138150 . ^ McSherry E (1981).
-
Lateral Periodontal Cyst
Wikipedia
. ^ a b c d e de Carvalho LF, Lima CF, Cabral LA, Brandão AA, Almeida JD (2010-10-27). "Lateral periodontal cyst: a case report and literature review" . Journal of Oral & Maxillofacial Research . 1 (4): e5. doi : 10.5037/jomr.2010.1405 . PMC 3886068 . ... Oral Surgery, Oral Medicine, Oral Pathology, Oral Radiology, and Endodontics . 81 (2): 210–6. doi : 10.1016/S1079-2104(96)80417-3 . ... OCLC 1105713150 . ^ Baker RD, D'Onofrio ED, Corio RL, Crawford BE, Terry BC (June 1979). "Squamous-cell carcinoma arising in a lateral periodontal cyst".
-
Spigelian Hernia
Wikipedia
"Spigelian Hernias: Repair and Outcome for 81 Patients". World Journal of Surgery . 26 (10): 1277–1281. doi : 10.1007/s00268-002-6605-0 . ... "An Unexpected Cause of Acute Abdomen" . Gastroenterology . 153 (4): e4–e5. doi : 10.1053/j.gastro.2017.01.057 . ... "Incidence and outcome of surgical repair of spigelian hernia". The British Journal of Surgery . 91 (5): 640–4. doi : 10.1002/bjs.4524 . ... "Congenital Spigelian hernia with cryptorchidism: probably a new syndrome". Hernia . 9 (4): 378–80. doi : 10.1007/s10029-005-0316-z .
- Pinealoblastoma Wikipedia
-
High Ankle Sprain
Wikipedia
Since the talus is wider anteriorly (in the front) than posteriorly (at the back), as the front of the foot is raised (dorsiflexed) reducing the angle between the foot and lower leg to less than 90°, then the mortise is confronted with an increasingly wider talus. ... In some cases, the diagnosis is only made after treatment for the more common, lateral, ankle sprain fails. [2] Diagnosis may also be delayed because swelling is usually minor or nonexistent and the true nature of the injury unappreciated. [3] A variety of diagnostic tests have been described such as the 'squeeze' (compressing the tibia and fibula above the midpoint of the calf), 'dorsiflexion with compression' (patient dorsiflexes the foot while the examiner compresses the internal and external malleolus), and 'external rotation' (patient sits with leg dangling and ankle at 90° and external rotation then applied to the foot) etc. ... "Diagnosis and treatment of acute ankle injuries: development of an evidence-based algorithm" . Orthop Rev (Pavia) . 4 (1): e5. doi : 10.4081/or.2012.e5 . PMC 3348693 .
-
Roemheld Syndrome
Wikipedia
The American Journal of Emergency Medicine . 36 (8): 1525.e5–1525.e7. doi : 10.1016/j.ajem.2018.05.002 . ... International Journal of Cardiology . 54 (3): 231–6. doi : 10.1016/0167-5273(96)02601-0 . PMID 8818746 . ^ Sharma, Shekhar.
-
Facial Infiltrating Lipomatosis
Wikipedia
"Congenital Infiltrating Lipomatosis of the Face" . Annals of Plastic Surgery . 80 (1): 83–89. doi : 10.1097/SAP.0000000000001213 . ... Plastic and Reconstructive Surgery . 136 : 72–73. doi : 10.1097/01.prs.0000472371.96995.e5 . ^ Clinical trial number NCT03094832 for "Study of ARQ 092 in Subjects With PIK3CA-related Overgrowth Spectrum and Proteus Syndrome (MOSAIC)" at ClinicalTrials.gov ^ Clinical trial number NCT04085653 for "Managed Access Program (MAP) to Provide Alpelisib (BYL719) for Patients With PIK3CA-Related Overgrowth Spectrum (PROS)" at ClinicalTrials.gov
- Teratospermia Wikipedia
-
Superior Mesenteric Artery Syndrome
Wikipedia
Superior mesenteric artery ( SMA ) syndrome is a gastro - vascular disorder in which the third and final portion of the duodenum is compressed between the abdominal aorta (AA) and the overlying superior mesenteric artery . This rare , potentially life-threatening syndrome is typically caused by an angle of 6°–25° between the AA and the SMA, in comparison to the normal range of 38°–56°, due to a lack of retroperitoneal and visceral fat ( mesenteric fat). ... "Nutcracker and SMA syndromes: What is the normal SMA angle in children?". European Journal of Radiology . 81 (8): e854-61. doi : 10.1016/j.ejrad.2012.04.010 . ... "Late superior mesenteric artery syndrome in paraplegia: case report and review" . Spinal Cord . 40 (2): 88–91. doi : 10.1038/sj.sc.3101255 . ... Journal of Pediatric Surgery . 42 (10): e5–e8. doi : 10.1016/j.jpedsurg.2007.07.002 .
-
Bird Fancier's Lung
Wikipedia
See also [ edit ] Hypersensitivity pneumonitis Farmer's lung References [ edit ] ^ Hashisako, Mikiko; Fukuoka, Junya; Smith, Maxwell L. (2018), "Chronic Diffuse Lung Diseases", Practical Pulmonary Pathology: A Diagnostic Approach , Elsevier, pp. 227–298.e5, doi : 10.1016/b978-0-323-44284-8.00008-9 , ISBN 9780323442848 ^ King, Thomas C. (2007), "Respiratory Tract and Pleura", Elsevier's Integrated Pathology , Elsevier, pp. 197–216, doi : 10.1016/b978-0-323-04328-1.50014-0 , ISBN 9780323043281 ^ King, Thomas C. (2007), "Respiratory Tract and Pleura", Elsevier's Integrated Pathology , Elsevier, pp. 197–216, doi : 10.1016/b978-0-323-04328-1.50014-0 , ISBN 9780323043281 ^ King, Thomas C. (2007), "Respiratory Tract and Pleura", Elsevier's Integrated Pathology , Elsevier, pp. 197–216, doi : 10.1016/b978-0-323-04328-1.50014-0 , ISBN 9780323043281 Hargreave FE, Pepys J, Longbottom JL, Wraith DG (1966).
-
Septic Arthritis
Wikipedia
Synovial fluid cultures will be positive in 80% of the cases. However, acid fast smears are not useful. ... PMID 21961455 . ^ a b c d e f g h i j k l m n o p q r s t u v w x y z aa ab ac ad ae af ag ah ai aj ak al am an ao ap aq ar as at au av aw ax ay az ba bb bc bd be bf bg bh bi bj bk bl bm bn bo bp bq br bs bt bu bv bw bx Horowitz, DL; Katzap, E; Horowitz, S; Barilla-LaBarca, ML (15 September 2011). ... Academic Emergency Medicine . 18 (8): 781–96. doi : 10.1111/j.1553-2712.2011.01121.x . ... PMID 17405973 . ^ a b c d e f g h i j k l m n o p q r s t u v w x y z aa ab ac ad ae af ag ah ai aj ak al am an ao ap Goldberg, D.L.; Sexton, D.J. (2017). ... Implications for treatment". J. Bone Joint Surg. Br . 80 (3): 471–3. doi : 10.1302/0301-620X.80B3.8296 .
-
Neonatal Hypoglycemia
Wikipedia
One way of screening includes a heel stick to test the blood glucose level at the bedside. [1] Diagnosing hypoglycemia in neonates requires two consecutive blood glucose readings of less than 40 mg/dl to properly diagnose hypoglycemia. [1] Bedside glucose monitoring is only effective if the equipment is accurate, rapid, and reliable. [1] This form of testing is often faster and more cost effective. [1] Laboratory serum glucose testing is the most accurate way of testing blood glucose levels. [1] These specimens are either taken from the heel, arterial, or venous punctures and must be store immediately on ice in order to prevent glycolysis, further altering the results. [1] USA guidelines recommended that the hypoglycemic neonate should have a glucose test every 2–4 hours for the first 24 hours of life. [1] Guidelines in the UK, however, recommend pre-feed screening of at-risk infants at 2–4 hours of age (to avoid false positives when blood glucose is, ordinarily, at its lowest at 2–3 hours of age) and at the subsequent feed until a blood glucose level of >2.0 mmol/l (36 mg/dl) on at least two consecutive occasions and is feeding well. [ citation needed ] Management [ edit ] Some infants are treated with 40% dextrose (a form of sugar) gel applied directly to the infant's mouth. [10] There are two main ways that neonatal hypoglycemia is treated. [1] The first way includes intravenous infusion of glucose. [1] For less severe, borderline, asymptomatic hypoglycemic neonates early introduction of breast milk can be effective for raising glucose levels to a healthy level. [1] Any infant at risk of hypoglycemia should have their blood sugar taken again one hour after birth. [1] Oral glucose is another option to restore normal glucose levels if the newborn is having difficulty latching to the breast or breastfeeding is not an option, however, breast milk is proven to be a better source as it includes glucose and carbohydrates. [1] It is recommended by The American Academy of Pediatrics that infants feed within the first hour of life with the glucose reading being 30 minutes after this feeding for an accurate result. [1] If the initial feeding does not raise the newborn's blood glucose above 40 mg/dl then the newborn must receive an IV infusion of 10% dextrose in water as a mini bolus as 2 ml/kg over 1 minute. [1] Following the mini bolus a continuous infusion of 10% dextrose in water at 80-100 ml/kg/day in order to maintain a healthy serum glucose level between 40–50 mg/dl. [1] Maintaining newborn thermoregulation is a large part in preventing further hypoglycemia as well. [1] Nursing care management [ edit ] The biggest nursing concern for a neonate experiencing hypoglycemia is the physical assessment to potentially find the cause. [1] It is also essential to prevent environmental factors such as cold stress that may predispose the newborn for further decreasing blood sugar. [1] Within the physical assessment, comorbidities of hypoglycemia should also be assessed such as intolerance of feeding, or respiratory distress. [1] Another important nursing intervention is assisting the mother in successful breastfeeding as this can prevent and treat hypoglycemia. [1] If an IV infusion of 10% dextrose in water is initiated then the nurse must monitor for: •Circulatory overload [1] •Hyperglycemia [1] •Glycosuria [1] •Intracellular dehydration [1] See also [ edit ] Congenital hyperinsulinism Hyperinsulinemic hypoglycemia References [ edit ] ^ a b c d e f g h i j k l m n o p q r s t u v w x y z aa ab ac ad ae af ag ah ai aj ak al am an ao ap aq ar as at au av aw ax ay az ba bb bc bd be bf bg bh bi bj bk bl bm bn bo Wong's nursing care of infants and children . ... CS1 maint: others ( link ) ^ a b c d e f g h i j k l m n o p q r s t u v w x y z aa Cranmer, Hilliarie. "Neonatal Hypoglycemia" .HNF4A, HNF1A, TBX19, GCK, AKT2, ZMPSTE24, PROP1, ABCC8, UCP2, KDM6A, KLF11, PIGQ, TRIP11, KCNQ1OT1, NEUROD1, APPL1, WAC, POMP, PRKAG2, ASXL2, GATAD2B, NSD1, CLPB, DNAJC19, H19, PAX4, H19-ICR, GYS2, GALC, FBP1, GPC3, KCNQ1, HADH, DBH, CYP11A1, HSD3B2, IGF2, CEL, INS, PDX1, CDKN1C, KCNJ11, BLK, ATP5F1D, MTOR, ALDH7A1, GH1, MLYCD, HIF1A, FOXA2, IGFBP3, HLTF, POMC, PCK1, NHS
-
Chondroblastoma
Wikipedia
However they more commonly originate from the metaphysis, lack calcification and have a different histologic organization pattern. [5] Other differential diagnoses for chondroblastoma consist of giant cell tumors , bone cysts , eosinophilic granulomas , clear cell chondrosarcomas , and enchondromas (this list is not exhaustive). [1] [5] Treatment [ edit ] Chondroblastoma has not been known to spontaneously heal and the standard treatment is surgical curettage of the lesion with bone grafting . [1] To prevent recurrence or complications it is important to excise the entire tumor following strict oncologic criteria . [1] [5] However, in skeletally immature patients intraoperative fluoroscopy may be helpful to avoid destruction of the epiphyseal plate. [1] In patients who are near the end of skeletal growth, complete curettage of the growth plate is an option. [1] In addition to curettage, electric or chemical cauterization (via phenol ) can be used as well as cryotherapy and wide or marginal resection . [1] [5] Depending on the size of the subsequent defect, autograft or allograft bone grafts are the preferred filling materials. [1] [5] Other options include substituting polymethylmethacrylate (PMMA) or fat implantation in place of the bone graft. [1] [3] [5] The work of Ramappa et al suggests that packing with PMMA may be a more optimal choice because the heat of polymerization of the cement is thought to kill any remaining lesion. [1] [3] Both radiotherapy and chemotherapy are not commonly used. [1] [5] Radiotherapy has been implemented in chondroblastoma cases that are at increased risk of being more aggressive and are suspected of malignant transformation . [1] [5] Furthermore, radiofrequency ablation has been used, but is typically most successful for small chondroblastoma lesions (approximately 1.5 cm). [1] Treatment with radiofrequency ablation is highly dependent on size and location due to the increased risk of larger, weight-bearing lesions being at an increased risk for articular collapse and recurrence. [1] [5] Overall, the success and method of treatment is highly dependent upon the location and size of the chondroblastoma. [1] [4] [5] Prognosis [ edit ] Although not specific to one mode of management, lesion size, patient sex, or follow-up, the recurrence rate for chondroblastoma is relatively high, and has been shown in select studies to be dependent upon the anatomical location, method of treatment, and biological aggressiveness of the initial lesion. [1] [3] [5] The rate of recurrence is highly variable, ranging between 5% and 40%, as study results are generally inconclusive. [1] However, local recurrence for long bone lesions is around 10%, with chondroblastoma in flat bones having higher recurrence and more complications. [1] [5] Recurrences are more common in cases involving an open epiphyseal plate where they can be attributed to inadequate curettage to avoid damage. [1] [5] Lesions of the proximal femur are particularly problematic because of difficulties accessing the femoral head for complete excision . [1] Chondroblastoma may recur in the soft tissue surrounding the initial lesion, especially in the case of incomplete curettage. [1] Recurrences have been shown to occur between 5 months and 7 years after initial treatment and are generally treated with repeat curettage and excision of affected soft-tissue. [1] [5] No histological differences have been seen between recurrent and non-recurrent chondroblastomas. [1] [4] [6] Rarely, more aggressive chondroblastomas can metastasize . [1] The most common location for metastases is the lung , with some cases also involving secondary bone sites, soft tissue, skin, or the liver . [1] [5] The prevalence of metastatic chondroblastoma, however, is quite low and is believed to be less than 1%. [1] There is no relationship established between metastasis and previous surgery, non-surgical treatment, anatomical location, or patient age. [1] Survival of patients with metastatic lesions is better when the metastases are surgically resectable, as chemotherapy has been shown to have little to no benefit. [1] Prognosis is bleak for patients with malignant chondroblastomas that are resistant to surgery, radiation, and chemotherapy. [5] However, patients with resectable metastases have survived for several years following diagnosis. [1] While recurrence is the most common complication of chondroblastoma other issues include post-surgery infection , degenerative joint disease , pathological fractures, failure of bone grafts, pre-mature epiphyseal closure , functional impairment, and malignant transformation. [1] [5] Complications are less common in patients presenting with chondroblastoma in accessible areas. [1] Overall, patients with more classical chondroblastoma (appearing in long bones, typical presentation) have better prognoses than patients with atypical chondroblastoma (flat bones, skull, etc.). [1] [3] [4] [5] [6] History [ edit ] Chondroblastoma was first described in 1927 as a cartilage-containing giant cell tumor by Kolodny but later characterized by Codman in 1931. [1] [4] Codman believed chondroblastoma to be an "epiphyseal chondromatous giant cell tumor" in the proximal humerus . [1] [3] This view was changed later by a comprehensive review completed by Jaffe and Lichtenstein in 1942 of similar tumors in other locations than the proximal humerus. [1] [4] They re-defined the tumor as a benign chondroblastoma of the bone that is separate from giant cell tumors. [1] [5] However, chondroblastoma of the proximal humerus is still sometimes referred to as Codman’s Tumor. [1] [3] [4] References [ edit ] ^ a b c d e f g h i j k l m n o p q r s t u v w x y z aa ab ac ad ae af ag ah ai aj ak al am an ao ap aq ar as at au av aw ax ay az ba bb bc bd be bf bg bh bi bj bk bl bm bn bo bp bq De Mattos, Camilia B. ... Web. 5 Dec. 2015. ^ a b c d e f g h i j k l m n o p q r s t u v w x y z aa ab ac ad ae af ag ah Damron, Timothy A.