-
Waldenström's Macroglobulinemia
Wikipedia
PMID 18809818 . ^ Kristinsson, S.; Björkholm, M.; Goldin, L.; McMaster, M.; Turesson, I.; Landgren, O. (2008). ... V.; Jimenez-Zepeda, V. H.; Schop, R. F. J.; Chesi, M.; Barrett, M.; Stewart, A. K.; Dogan, A.; Bergsagel, P. ... P.; Witzig, T. E.; Hideshima, T.; Brown, M.; Anderson, K. C.; Ghobrial, I. M. (2008). ... PMID 19351844 . ^ Gutiérrez, N.; Ocio, E.; De Las Rivas, J.; Maiso, P.; Delgado, M.; Fermiñán, E.; Arcos, M.; Sánchez, M.; Hernández, J.; San Miguel, J. ... PMID 18813229 . ^ Kyle RA, Treon SP, Alexanian R, Barlogie B, Bjorkholm M, Dhodapkar M, Lister TA, Merlini G, Morel P, Stone M, Branagan AR, Leblond V (2003).MYD88, PAX5, IGH, LPL, CXCR4, ANPEP, MYC, ZAP70, MALT1, CDR3, MYOM2, SDC1, CXCL12, AIMP2, TCL1A, GRAP2, TCL1B, AHSA1, ACSBG1, RNF19A, IBTK, POLDIP2, IGHV4-34, BCL11A, KRT20, EXOC2, RAPH1, MAPK1, NOS1, NOTCH2, NOS2, BCL6, BCL9, BLM, BRAF, BSG, BTK, SERPING1, CCND3, CD6, MS4A1, TNFRSF8, CD40LG, CD79A, CRK, MAPK14, CTNNB1, IL4, IRF4, CD200, NCAM1, CCND1, SLC35B2
-
Blue Cone Monochromacy
Wikipedia
PMID 13682677 . ^ a b c d e f g h i Cideciyan, A V; Hufnagel, R B; Carroll, J; Sumaroka, A; Luo, X; Schwartz, S B; Dubra, A; Land, M; Michaelides, M; Gardner, J C; Hardcastle, A J; Moore, A T; Sisk, R A; Ahmed, Z M; Kohl, S; Wissinger, B; Jacobson, S G (2013). ... PMID 19421413 . ^ a b c d e f g Michaelides, M; Johnson, S; Simunovic, M P; Bradshaw, K; Holder, G; Mollon, J D; Moore, A T; Hunt, D M (2005). ... PMC 1395698 . PMID 5313219 . ^ a b c Crognale, M A; Fry, M; Highsmith, J; Haegerstrom-Portnoy, G; Neitz, M; Neitz, J; Webster, M A (2004). ... PMID 20638402 . ^ Carroll, J; Baraas, R C; Wagner-Schuman, M; Rha, J; Siebe, C A; Sloan, C; Tait, D M; Thompson, S; Morgan, J I; Neitz, J; Williams, D R; Foster, D H; Neitz, M (2009). ... PMC 2791574 . PMID 19934058 . ^ Wagner-Schuman, M; Neitz, J; Rha, J; Williams, D R; Neitz, M; Carroll, J (2010).
-
Pancreatic Serous Cystadenoma
Wikipedia
Since these lesions do not have malignant potential, long-term observation with imaging surveillance is unnecessary. [5] Surgery can include the removal of the head of the pancreas (a pancreaticoduodenectomy ), removal of the body and tail of the pancreas (a distal pancreatectomy ), or rarely removal of the entire pancreas (a total pancreatectomy). [7] In selected cases the surgery can be performed using minimally invasive techniques such as laparoscopy . [8] Epidemiology [ edit ] Serous cystadenomas of the pancreas are more common in women. [5] SCAs are usually diagnosed in people 50-60 years of age. [5] See also [ edit ] Ovarian serous cystadenoma Pancreatic mucinous cystadenoma Solid pseudopapillary neoplasm References [ edit ] ^ Jais, B; Rebours, V; Malleo, G; Salvia, R; Fontana, M; Maggino, L; Bassi, C; Manfredi, R; Moran, R; Lennon, AM; Zaheer, A; Wolfgang, C; Hruban, R; Marchegiani, G; Fernández Del Castillo, C; Brugge, W; Ha, Y; Kim, MH; Oh, D; Hirai, I; Kimura, W; Jang, JY; Kim, SW; Jung, W; Kang, H; Song, SY; Kang, CM; Lee, WJ; Crippa, S; Falconi, M; Gomatos, I; Neoptolemos, J; Milanetto, AC; Sperti, C; Ricci, C; Casadei, R; Bissolati, M; Balzano, G; Frigerio, I; Girelli, R; Delhaye, M; Bernier, B; Wang, H; Jang, KT; Song, DH; Huggett, MT; Oppong, KW; Pererva, L; Kopchak, KV; Del Chiaro, M; Segersvard, R; Lee, LS; Conwell, D; Osvaldt, A; Campos, V; Aguero Garcete, G; Napoleon, B; Matsumoto, I; Shinzeki, M; Bolado, F; Fernandez, JM; Keane, MG; Pereira, SP; Acuna, IA; Vaquero, EC; Angiolini, MR; Zerbi, A; Tang, J; Leong, RW; Faccinetto, A; Morana, G; Petrone, MC; Arcidiacono, PG; Moon, JH; Choi, HJ; Gill, RS; Pavey, D; Ouaïssi, M; Sastre, B; Spandre, M; De Angelis, CG; Rios-Vives, MA; Concepcion-Martin, M; Ikeura, T; Okazaki, K; Frulloni, L; Messina, O; Lévy, P (February 2016). ... PMID 26045140 . ^ Colonna, J.; Plaza, JA.; Frankel, WL.; Yearsley, M.; Bloomston, M.; Marsh, WL. (2008). ... PMID 18382099 . S2CID 28918883 . ^ Eras, M.; Yenigun, M.; Acar, C.; Kumbasar, B.; Sar, F.; Bilge, T. (2004).
-
Chronic Enteropathy Associated With Slco2a1 Gene
Wikipedia
You can help by adding to it . ( November 2017 ) References [ edit ] ^ Okabe H, Sakimura M (1968) Nonspecific multiple ulcer of the small intestine. Stomach and Intestine 3: 1539–1549 ^ Matsumoto T, Iida M, Matsui T, Yao T, Watanabe H, Yao T, Okabe H (2004) Non-specific multiple ulcers of the small intestine unrelated to non-steroidal anti-inflammatory drugs. ... Gastrointest Endosc 66(3 Suppl):S99-107 ^ Umeno J, Hisamatsu T, Esaki M, Hirano A, Kubokura N, Asano K, Kochi S, Yanai S, Fuyuno Y, Shimamura K, Hosoe N, Ogata H, Watanabe T, Aoyagi K, Ooi H, Watanabe K, Yasukawa S, Hirai F, Matsui T, Iida M, Yao T, Hibi T, Kosaki K, Kanai T, Kitazono T, Matsumoto T (2015) A hereditary enteropathy caused by mutations in the SLCO2A1 gene, encoding a prostaglandin transporter. PLoS Genet 5:11(11):e1005581. doi: 10.1371/journal.pgen.1005581 ^ Matsumoto T, Nakamura S, Esaki M, Yada S, Koga H, Yao T, Iida M (2006) Endoscopic features of chronic nonspecific multiple ulcers of the small intestine: comparison with nonsteroidal anti-inflammatory drug-induced enteropathy. Dig Dis Sci 51(8):1357-1363 ^ Yanai S, Yamaguchi S, Nakamura S, Kawasaki K, Toya Y, Yamada N, Eizuka M, Uesugi N, Umeno J, Esaki M, Okimoto E, Ishihara S, Sugai T, Matsumoto T (January 2019).
-
Isolated Primary Immunoglobulin M Deficiency
Wikipedia
Isolated primary immunoglobulin M deficiency Other names Selective IgM immunodeficiency Immunoglobulin M Specialty Hematology Isolated primary immunoglobulin M deficiency [1] is a poorly defined dysgammaglobulinemia characterized by decreased levels of IgM while levels of other immunoglobulins are normal. ... Notwithstanding a clear pathogenesis and commonly accepted definition, a cutoff for SIgMD could be the lower limit of the serum IgM reference range, such as 43 mg/dL [5] in adults or even 20 mg/dL. [6] See also [ edit ] Immunodeficiency with hyper-immunoglobulin M Immunoglobulin M List of cutaneous conditions References [ edit ] ^ Rapini, Ronald P.; Bolognia, Jean L.; Jorizzo, Joseph L. (2007). ... "Hypomorphic Mutations in the BCR Signalosome Lead to Selective Immunoglobulin M Deficiency and Impaired B-cell Homeostasis" .
-
Lujan–fryns Syndrome
Wikipedia
S.; Lubs, H. A.; Verloes, A.; May, M. M.; Risheg, H.; Friez, M. J.; Futreal, P. ... PMID 17036352 . ^ a b c d Wittine, L. M.; Josephson, K. D.; Williams, M. S. ... E.; Carlin, M. E.; Lubs, H. A.; Opitz, J. M. (Jan 1984). ... PMID 12784307 . ^ Gambarin, F.; Favalli, V.; Serio, A.; Regazzi, M.; Pasotti, M.; Klersy, C.; Dore, R.; Mannarino, S.; Viganò, M.; Odero, A.; Amato, S.; Tavazzi, L.; Arbustini, E. ... M.; Moeschler, J. B.; Peiffer, A. P.; May, M.; Joseph, S.
-
Macrocephaly-Capillary Malformation
Wikipedia
PMID 22658544 . ^ Lee, JH.; Huynh, M.; Silhavy, JL.; Kim, S.; Dixon-Salazar, T.; Heiberg, A.; Scott, E.; Bafna, V.; et al. (2012). ... PMID 10710221 . ^ Robertson SP, Gattas M, Rogers M, Adès LC (2000). "Macrocephaly--cutis marmorata telangiectatica congenita: report of five patients and a review of the literature" . ... PMID 10649789 . ^ Conway RL, Pressman BD, Dobyns WB, Danielpour M, Lee J, Sanchez-Lara PA, et al. (2007). ... PMID 22329570 . ^ Erener Ercan, T.; Oztunc, F.; Celkan, T.; Bor, M.; Kizilkilic, O.; Vural, M.; Perk, Y.; Islak, C.; Tuysuz, B. ... "Accurately renaming macrocephaly-cutis marmorata telangiectatica congenita (M-CMTC) as macrocephaly-capillary malformation (M-CM)" .
-
Mucinous Cystic Neoplasm
Wikipedia
Mucinous cystic neoplasms of the liver are a type of liver cancer in which tissue similar to the stroma of ovary occurs. [1] References [ edit ] ^ Kishida, N; Shinoda, M; Masugi, Y; Itano, O; Fujii-Nishimura, Y; Ueno, A; Kitago, M; Hibi, T; Abe, Y; Yagi, H; Tanimoto, A; Tanabe, M; Sakamaoto, M; Kitagawa, Y (21 July 2014).
-
Coffin–siris Syndrome
Wikipedia
References [ edit ] ^ Levy P, Baraitser M (May 1991). "Coffin-Siris syndrome" . ... Retrieved 13 June 2015 . ^ Sousa SB, Abdul-Rahman OA, Bottani A, Cormier-Daire V, Fryer A, Gillessen-Kaesbach G, Horn D, Josifova D, Kuechler A, Lees M, MacDermot K, Magee A, Morice-Picard F, Rosser E, Sarkar A, Shannon N, Stolte-Dijkstra I, Verloes A, Wakeling E, Wilson L, Hennekam RC (August 2009). ... Retrieved 13 June 2015 . ^ Vals MA, Õiglane-Shlik E, Nõukas M, Shor R, Peet A, Kals M, Kivistik PA, Metspalu A, Õunap K (November 2014). ... PMID 24569609 . ^ Tsurusaki Y, Koshimizu E, Ohashi H, Phadke S, Kou I, Shiina M, Suzuki T, Okamoto N, Imamura S, Yamashita M, Watanabe S, Yoshiura K, Kodera H, Miyatake S, Nakashima M, Saitsu H, Ogata K, Ikegawa S, Miyake N, Matsumoto N (June 2014). ... PMID 24886874 . ^ Gazdagh G, Blyth M, Scurr I, Turnpenny PD, Mehta SG, Armstrong R, McEntagart M, Newbury-Ecob R, Tobias ES, Joss S (April 2018).ARID1B, ARID1A, SMARCE1, SOX11, SMARCB1, SMARCA4, SMARCA1, SMARCA2, DPF2, ARID2, PHF6, SOX4, SMARCC2, BANF1, WG, SDHD, IL10, SDHB, SDHC, CMAS, IL17RB, CCL26, FAM3C, SDS, NIPBL, PTPN22, SMARCAL1, WNT16, PGR, TNFRSF10C, MYDGF, CD14, IL25, CPED1, ATR, ATM, SARDH, TNF, TNFSF10, EDN1, PRTN3, MPO, SET, MMP9, MMP2, ITGB2, IL5, FASLG, SORD, HLA-DRB4, HLA-DRB1, TRBV20OR9-2, TGFB1, TGFB2, PREP, FAS
-
Leber Hereditary Optic Neuropathy
Gene_reviews
The diagnosis of LHON is established in a proband with bilateral, painless, subacute visual failure that develops during young adult life and/or by the identification of one of three common mtDNA pathogenic variants (m.3460G>A in MT-ND1 , m.11778G>A in MT-ND4 , or m.14484T>C in MT-ND6 ) on molecular genetic testing. ... Following the nadir, visual acuity may improve; such improvement is more likely in individuals with the m.14484T>C pathogenic variant than in those with the m.11778G>A or m.3460G>A pathogenic variant (see Genotype-Phenotype Correlations). ... Genotype-Phenotype Correlations Some broad categorization can be made with regard to specific LHON-causing pathogenic variants: m.3460G>A is associated with the worst impairment in visual function. m.11778G>A has an intermediate phenotype. m.14484T>C is associated with the best long-term visual outcome. ... Lifetime Risk for Visual Failure in Individuals with a Homoplasmic Primary LHON-Causing Mitochondrial DNA Pathogenic Variant by Study View in own window Mitochondrial DNA Pathogenic Variant Risk of Developing Symptoms Median Age at Onset (Males) Male/Female Ratio Reference Males Females m.3460G>A 32% 15% 20 yrs 4.3:1 Nikoskelainen [1994] m.3460G>A 49% 28% 22 yrs 1.7:1 Yu-Wai-Man et al [2003] m.11778G>A 43% 11% 24 yrs 3.7:1 Harding et al [1995] m.11778G>A 51% 9% 22 yrs 5.1:1 Yu-Wai-Man et al [2003] m.14484T>C 47% 8% 20 yrs 7.7:1 Macmillan et al [1998] A multiple sclerosis-like illness has been reported in association with all three primary mtDNA LHON-causing pathogenic variants (m.3460G>A, m.11778G>A, and m.14484T>C), but with a female bias [Pfeffer et al 2013]. ... In total, 85 affected individuals harboring one of the three primary mtDNA LHON-causing variants (m.3460G>A, m.11778G>A, and m.14484T>C) were successfully enrolled in this multicenter study [Klopstock et al 2013].ND6, ND1, ND4, ND5, ND4L, ATP6, CYTB, COX3, ND2, RPE65, NDUFS2, COX1, IL1B, IL1A, LRAT, CPLX1, OPA1, TBC1D24, PARL, OPA3, CEP290, NDUFA1, CRYZ, FXN, MFN2, PLXNA2, NPTX2, SOD2, RP2, SPG7, RPGR, TAP2, SCN1A, TFPI, TFAM, ABCA4, TK2, TWNK, GGT2, POTEF, GGTLC3, GGTLC5P, SLC26A5, GLIS3, GMCL2, GMCL1, RPGRIP1, ADI1, TP53, NDUFB11, YARS2, GCA, AIPL1, KIF1B, IMMT, OPTN, COX5A, PHLDA2, POLG, RNR2, SERPINA1, PGD, ERG, EPHX1, ENO2, ENDOG, TIMM8A, ACE, CPOX, COX8A, CAT, CASP3, BNIP3L, BNIP3, AR, AQP4, AMD1P2, AMD1, AKR1B1, ESR2, GGT1, GCLC, MAS1, TRNK, TRNF, ACTB, RNR1, MTHFR, COX2, TRNC, MAPT, GRIA1, TACSTD2, KRT10, HLA-B, HLA-A, GSR, GRM2, GRIA2, GGTLC4P
-
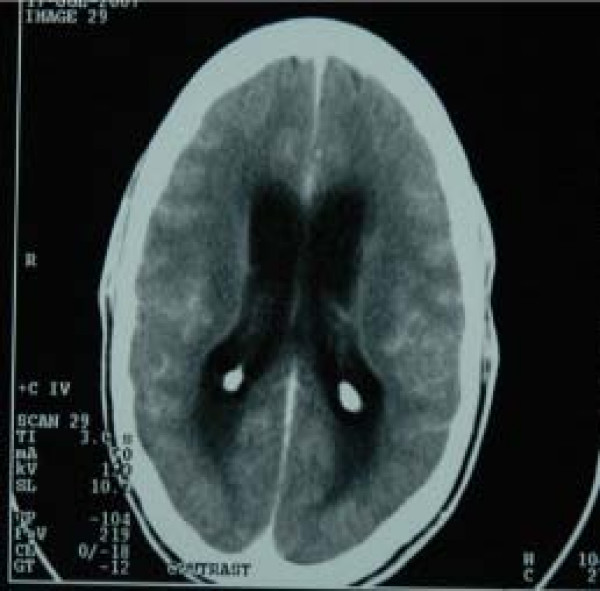
Tuberculous Meningitis
Wikipedia
Acid-fast bacilli are sometimes seen on a CSF smear, but more commonly, M. tuberculosis is grown in culture. [11] A spiderweb clot in the collected CSF is characteristic of TB meningitis, but is a rare finding. ... Retrieved 2015-06-02 . ^ Leach, Richard M. (2010-06-11). Acute and Critical Care Medicine at a Glance . ... External links [ edit ] Classification D ICD - 10 : A17.0 , G01 ICD - 9-CM : 013.0 , 322.9 MeSH : D014390 External resources MedlinePlus : 000650 eMedicine : neuro/385 Scholia has a topic profile for Tuberculous meningitis . v t e Gram-positive bacterial infection : Actinobacteria Actinomycineae Actinomycetaceae Actinomyces israelii Actinomycosis Cutaneous actinomycosis Tropheryma whipplei Whipple's disease Arcanobacterium haemolyticum Arcanobacterium haemolyticum infection Actinomyces gerencseriae Propionibacteriaceae Propionibacterium acnes Corynebacterineae Mycobacteriaceae M. tuberculosis / M. bovis Tuberculosis : Ghon focus / Ghon's complex Pott disease brain Meningitis Rich focus Tuberculous lymphadenitis Tuberculous cervical lymphadenitis cutaneous Scrofuloderma Erythema induratum Lupus vulgaris Prosector's wart Tuberculosis cutis orificialis Tuberculous cellulitis Tuberculous gumma Lichen scrofulosorum Tuberculid Papulonecrotic tuberculid Primary inoculation tuberculosis Miliary Tuberculous pericarditis Urogenital tuberculosis Multi-drug-resistant tuberculosis Extensively drug-resistant tuberculosis M. leprae Leprosy : Tuberculoid leprosy Borderline tuberculoid leprosy Borderline leprosy Borderline lepromatous leprosy Lepromatous leprosy Histoid leprosy Nontuberculous R1 : M. kansasii M. marinum Aquarium granuloma R2 : M. gordonae R3 : M. avium complex / Mycobacterium avium / Mycobacterium intracellulare / MAP MAI infection M. ulcerans Buruli ulcer M. haemophilum R4 / RG : M. fortuitum M. chelonae M. abscessus Nocardiaceae Nocardia asteroides / Nocardia brasiliensis / Nocardia farcinica Nocardiosis Rhodococcus equi Corynebacteriaceae Corynebacterium diphtheriae Diphtheria Corynebacterium minutissimum Erythrasma Corynebacterium jeikeium Group JK corynebacterium sepsis Bifidobacteriaceae Gardnerella vaginalis v t e Meningitis and other diseases of meninges Meningitis Arachnoiditis Bacterial Tuberculous Haemophilus Pneumococcal Viral Herpesviral Fungal Cryptococcal Aseptic Drug-induced Other MeningoencephalitisBBS9, CSF2, LAMC2, ADA, LTA4H, MMP9, IFNG, RHOF, TLR2, RNF34, NCAPG2, MT1JP, TIRAP, IL10, CRP, TNF, IL1B, IL13, THEMIS, BECN1, ZNF410, VEGFA, CCN6, MIR29A, TTR, TRC-GCA24-1, VDR, GDF15, C1QTNF4, ARTN, SMUG1, AGO2, TIMP2, DLL1, CD274, RMC1, VSX1, TLR9, NAT2, SAA2, TIMP1, SPN, ADSL, AGRP, ALOX5, CAMP, CAT, CSF3, ESR1, GC, CFH, HPD, IL2, IL4, IL6, CXCL8, IL12B, IL17A, CXCL10, INS, MMP2, MUC5AC, NCAM1, SAA1, CCL1, CCL2, CCL3, SIGLEC14
-
Plasma Cell Granuloma
Wikipedia
Localization [ edit ] Lung [3] [4] See also [ edit ] Pulmonary hyalinizing granuloma References [ edit ] ^ Dias, O. M.; Kawassaki Ade, M; Haga, H; Cukier, A; Carvalho, C. ... PMID 22086532 . ^ Nonomura, A; Mizukami, Y; Matsubara, F; Shimizu, J; Oda, M; Watanabe, Y; Kamimura, R; Takashima, T; Kitagawa, M (1992). ... PMID 1392177 . ^ Nonomura, A; Mizukami, Y; Matsubara, F; Shimizu, J; Oda, M; Watanabe, Y; Kamimura, R; Takashima, T; Kitagawa, M (1992).
-
Ichthyosis With Confetti
Wikipedia
.; Palcesky, D.; Busbey, S.; Medenica, M. (2003). "Congenital reticular ichthyosiform erythroderma--ichthyosis variegata: a case report and review of the literature" . ... Nature . doi : 10.1038/news.2010.434 . ^ a b Kretzschmar, Kai; Watt, Fiona M. (2012). "Lineage Tracing" . Cell . 148 (1–2): 33–45. doi : 10.1016/j.cell.2012.01.002 . PMID 22265400 . ^ Choate, K. A.; Lu, Y.; Zhou, J.; Choi, M.; Elias, P. M.; Farhi, A.; Nelson-Williams, C.; Crumrine, D.; Williams, M. L.; Nopper, A. J.; Bree, A.; Milstone, L. M.; Lifton, R. P. (2010). "Mitotic Recombination in Patients with Ichthyosis Causes Reversion of Dominant Mutations in KRT10" .
-
Migrainous Infarction
Wikipedia
CS1 maint: DOI inactive as of January 2021 ( link ) ^ a b c d e Viana, M.; Linde, M.; Sances, G.; Ghiotto, N.; Guaschino, E.; Allena, M.; Terrazzino, S.; Nappi, G.; Goadsby, P. ... PMID 9565010 . ^ a b Montaner, J.; Perea-Gainza, M.; Delgado, P.; Ribó, M.; Chacón, P.; Rosell, A.; Quintana, M.; Palacios, M. ... S2CID 1690024 . ^ Wessels, T.; Röttger, C.; Jauss, M.; Kaps, M.; Traupe, H.; Stolz, E. (2005-04-01). ... PMID 15746460 . S2CID 15123728 . ^ Jauss, M.; Wessels, T.; Trittmacher, S.; Allendörfer, J.; Kaps, M. (2006-08-01). ... S2CID 53549605 . ^ a b Hacke, W.; Kaste, M.; Bluhmki, E.; Brozman, M.; Dávalos, A.; Guidetti, D.; Larrue, V.; Lees, K.
-
Narp Syndrome
Orphanet
Etiology NARP syndrome is caused in the large majority of patients by a m.8993T>C/G in the subunit 6 of mitochondrial H(+)-ATPase gene ( MTATP6 ). Most NARP patients have 70-90% mutated mitochondrial DNA. The m.8993T>G mutation is also present in 8-10% of patients with Leigh syndrome when mutated mitochondrial DNA is > 90%. Less common ATP6 heteroplasmic mutations include m.8839G>C, m.8989G>C, m.8618-8619insT, m.9032T>C, and m.9127-9128 delAT microdeletion, all identified in single families.
-
Distal Spinal Muscular Atrophy Type 1
Wikipedia
M.; Lombardo, F.; Crisafulli, G.; De Luca, F. (2011). ... PMID 16964485 . ^ a b c d e f g Kaindl, A. M.; Guenther, U. -P.; Rudnik-Schoneborn, S.; Varon, R.; Zerres, K.; Schuelke, M.; Hubner, C.; Von Au, K. (2007). ... H.; Finkel, R. S.; Bertini, E. S.; Schroth, M.; Simonds, A.; Wong, B.; Aloysius, A.; Morrison, L.; Main, M.; Crawford, T. ... Journal of Child Neurology . 23 (2): 199–204. doi : 10.1177/0883073807310989 . PMID 18263757 . Messina, M. F.; Messina, S.; Gaeta, M.; Rodolico, C.; Salpietro Damiano, A. M.; Lombardo, F.; Crisafulli, G.; De Luca, F. (2011).
-
Elastofibroma Dorsi
Wikipedia
.; Grimer, R. J.; Carter, S. R.; Tillman, R. M.; Abudu, A.; Davies, A. M.; Sumathi, V. ... PMID 18382611 . ^ a b c d Briccoli, A.; Casadei, R.; Di Renzo, M.; Favale, L.; Bacchini, P.; Bertoni, F. (2000). ... PMID 10664338 . ^ a b c d e f Mortman, K. D.; Hochheiser, G. M.; Giblin, E. M.; Manon-Matos, Y.; Frankel, K. M. (2007). "Elastofibroma Dorsi: Clinicopathologic Review of 6 Cases". ... M.; Saifuddin, A.; Pollock, R. C.; Skinner, J.
-
Multifocal Micronodular Pneumocyte Hyperplasia
Wikipedia
.; Leslie, K. O.; Popper, H; Kitaichi, M; Gagné, E; Emelin, J. K.; Vinters, H. ... The American Journal of Surgical Pathology . 22 (4): 465–72. doi : 10.1097/00000478-199804000-00012 . PMID 9537475 . ^ Ishii, M; Asano, K; Kamiishi, N; Hayashi, Y; Arai, D; Haraguchi, M; Sugiura, H; Naoki, K; Tasaka, S; Soejima, K; Sayama, K; Betsuyaku, T (2012). ... PMID 22884294 . ^ Shintani, Y; Ohta, M; Iwasaki, T; Ikeda, N; Tomita, E; Nagano, T; Kawahara, K (2010). ... PMID 20190710 . ^ Kobashi, Y; Sugiu, T; Mouri, K; Irei, T; Nakata, M; Oka, M (2008). "Multifocal micronodular pneumocyte hyperplasia associated with tuberous sclerosis: Differentiation from multiple atypical adenomatous hyperplasia" . ... PMID 9331299 . ^ Fujitaka, K; Isobe, T; Oguri, T; Yamasaki, M; Miyazaki, M; Kohno, N; Takeshima, Y; Inai, K (2002).
-
Congenital Amegakaryocytic Thrombocytopenia
Wikipedia
It is known for patients to continue to create very small numbers of platelets over time. [ citation needed ] See also [ edit ] Thrombopoietin Myeloproliferative leukemia virus oncogene References [ edit ] ^ Ballmaier M, Germeshausen M, Schulze H, et al. ... Blood . 97 (1): 139–46. doi : 10.1182/blood.V97.1.139 . PMID 11133753 . ^ Germeshausen M, Ballmaier M, Welte K (March 2006). ... S2CID 23164119 . ^ a b Ihara K, Ishii E, Eguchi M, Takada H, Suminoe A, Good RA, Hara T (1999). ... PMC 15907 . PMID 10077649 . ^ Ballmaier M, Germeshausen M, Schulze H, Cherkaoui K, Lang S, Gaudig A, Krukemeier S, Eilers M, Strauss G, Welte K (2001). ... PMID 11133753 . ^ King S, Germeshausen M, Strauss G, Welte K, Ballmaier M (December 2005).
-
Mycobacterium Avium-Intracellulare Infection
Wikipedia
It is typically treated with a series of three antibiotics for a period of at least six months. M. avium , M. intracellulare , and M. chimaera are each saprotrophic organisms present in soil and water; entry into hosts is usually via the gastrointestinal tract , but also can be via the lungs . ... M. avium typically causes unilateral swelling of one of the lymph nodes of the neck. ... M. avium , M. intracellulare , and M. chimaera . [4] It causes Mycobacterium avium-intracellulare infection. [5] [6] Some sources also include Mycobacterium avium subspecies paratuberculosis (MAP). [7] Risk factors [ edit ] MAI is common in immunocompromised individuals, including senior citizens and those with HIV/AIDS or cystic fibrosis . ... MMWR Recomm Rep . 42 (RR-9): 14–20. PMID 8393134 . ^ Wickremasinghe M, Ozerovitch LJ, Davies G, et al. (December 2005). ... ISSN 0012-3692 . PMID 1600780 . ^ Reich, Jerome M. (August 2018). "In Defense of Lady Windermere Syndrome" .HSPD1, TNF, SLC11A1, IFNG, NTM, STAT1, STAT4, TLR2, TNFSF4, TP63, TNFSF9, ARHGEF2, IL32, AIM2, RABEPK, LANCL1, STS, PSMD7, IL37, PYCARD, IL23A, NCAPG2, RGMA, MLIP, NLRP3, IL31RA, ARMH1, MIR346, AK6, EBNA1BP2, MAPK1, CAMP, IFNA13, CASP1, TNFSF8, CD70, CFTR, CCR5, FCN2, GATA2, HLA-B, HSPE1, ICAM1, IFNA1, IFNB1, NMT1, IL1B, IL2, IL9, IL12RB1, TNFRSF9, IL17A, CXCL10, RPSA, CXCL9, MT1JP, RNR1, H3P28