-
Concha Bullosa
Wikipedia
Occasionally, a large concha bullosa may cause it to bulge sufficiently to obstruct the opening of an adjacent sinus, possibly leading to recurrent sinusitis . [1] In such a case the turbinate can be reduced in size by endoscopic nasal surgery ( turbinectomy ). The presence of a concha bullosa is often associated with deviation of the nasal septum toward the opposite side of the nasal cavity. [2] Although it is thought that sinusitis or sinus pathology has relation to concha bullosa, no strong statistical correlation has been demonstrated. [1] Additional image [ edit ] References [ edit ] ^ a b c d Hatipoğlu, HG; Cetin, MA; Yüksel, E (Sep 2005). ... "The incidence of concha bullosa and its relationship to nasal septal deviation and paranasal sinus disease". American Journal of Neuroradiology . 25 (9): 1613–8.
-
Interatrial Communication
Orphanet
Only these two defects are true atrial septal defects. The sinus venosus defect (one-tenth of cases) is a hole outside the confines of the oval fossa, through which a caval vein and/or pulmonary vein(s) override the atrial septum or the septum secundum (superior interatrial fold) producing an interatrial or anomalous veno-atrial communication.The rarest defect, the coronary sinus defect, is a communication between the left atrium and the coronary sinus allowing interatrial communication through the orifice of the coronary sinus, and is due to absence or partial unroofing of the coronary sinus.NKX2-5, PQBP1, GATA4, MYH6, GABRQ, MYT1L, TRIP12, CCN1, NTF3, ACTC1, FOXC1, TBX5, TLL1, PTPN11, PTEN, BMPR1A, SALL4, COMT, NODAL, EVC, B3GLCT, MAP2K1, GATA6, TTN, SHANK3, TRIP13, ABL1, BUB3, SMC3, BAZ1B, CDC45, ARID1A, NAA10, SMC1A, CDK13, SEC24C, EFTUD2, LONP1, ZMPSTE24, GPC6, MED12, RBM8A, WASHC5, FIG4, ZEB2, KIAA0586, TMEM94, SEMA3E, CEP57, TTC37, USP9X, GTF2IRD1, TBX4, RBM10, WT1, MKKS, KMT2D, SOS1, SON, SNRPB, SMN1, SMARCE1, SKIV2L, SCN4A, SALL1, RREB1, RPS17, RPL27, RPL5, RIT1, RFC2, RAF1, STK4, ABCC8, TALDO1, NELFA, SHOC2, KAT6A, PCGF2, ZIC3, XRCC2, CITED2, NSD2, TBX1, CLIP2, KDM6A, UFD1, HIRA, NKX2-1, TBX2, TRAIP, MRAS, MAD2L2, UPF3B, UBE3B, TMEM87B, SLX4, PHF6, BRIP1, CEP290, PALB2, NXN, VAC14, NSD1, STRA6, XYLT2, FANCM, ARHGAP31, ARID1B, KIF15, NEK9, G6PC3, CHST14, MMP21, TTN-AS1, RNU4ATAC, DIPK1A, CTU2, KANSL1, JMJD1C, UBR1, ASXL1, ESCO2, CEP120, CCBE1, GATA5, AMER1, EVC2, B3GALT6, HDAC8, CHD7, SLC19A2, PIGN, TBL2, VPS33B, AUTS2, SETBP1, C2CD3, SH2B1, NIPBL, KAT6B, ASXL2, HAAO, TGDS, SIK3, SPECC1L, RAD51, TXNL4A, KDM5B, NPHP3, CCDC22, UBE2T, SLC25A24, FANCI, SETD5, RFWD3, FANCL, AGGF1, BCOR, NDUFB11, TMCO1, RAB23, OTUD6B, DYNC2LI1, LARP7, DACT1, ZDHHC9, TBX22, RAD51C, STIM1, RAD21, FOXF1, ERCC4, FANCA, FANCC, FANCD2, FANCE, FANCB, FANCF, FANCG, FBN2, FKTN, GPC4, FGFR1, PEX19, FGFR2, FLNB, LETM1, GDF1, GJA1, GPC3, GLI1, GLI3, GP1BB, GPX4, GTF2I, HCCS, HNRNPK, HRAS, HSPA9, HSPG2, KIF11, EP300, ELN, ECE1, DNMT3A, ACTL6A, JAG1, ANK1, ARSD, ARVCF, ATIC, RERE, ATP6V1A, ATP6V1E1, BCR, BMP2, BRCA1, BRAF, BRCA2, BUB1, BUB1B, MYRF, TMEM258, LYST, CHRM3, COL1A1, COL5A1, COL5A2, COX7B, CREBBP, CRKL, CYP11A1, DHCR7, DMD, KRAS, FGFR3, MYH7, MASP1, KMT2A, MMP2, MAP2K2, MMP14, MAPK1, MMUT, NFIX, NOTCH2, LMNA, POR, ROR2, POLA1, PAX3, PCNT, PIGA, PIK3R2, LIMK1, MEIS2, PITX2, SMS, RSS, TBX20, CYP11B2, ACTA2, IL1B, IL18, CRP, WNT1, CNTNAP2, BMP4, CYP1B1, MTHFR, STX18, BDNF, MSX1, SHANK2, ASNS, ACTB, CNTNAP3, MIR499A, ELMOD3, PITX3, SOD1, SIL1, SNAP25, ARSA, MIR486-1, CACNA1C, CAPG, EBPL, LGALS7B, CAT, CCNA2, CDH11, SHROOM3, NUFIP2, POMC, FOXL2, ADO, TARP, ANGPT2, PSD, SLFN14, MAPK3, PTH, SAA1, SAA2, ACTN4, OSR1, RBM45, MIRLET7B, OPN1SW, ACTA1, MIR139, SCN2A, MIR27A, SYTL4, PPP3CA, NEXN, BMPR2, LBX2, RELN, MDD1, LGALS7, CYP2E1, RTN4, COL4A1, HEY2, ZFPM2, MSX2, FOXE3, KDM4C, FMR1, PHB2, WDHD1, MMP3, DGCR6, LZTR1, TSHZ1, GRM5, GRM7, MEFV, MECP2, HLA-DRB1, SMAD4, LRPAP1, AXIN1, HTC2, IL1A, IL4, IL6, CXCL8, ISL1, KLRC2, MYBPC3, VEGFA, NOS3, TGFB1, PCDHGA4, CFC1, CDKL5, PCYT1A, SYN2, CHDH, NRP1, PAX6, HYDIN, PCSK6, DMPK, ARID4B, DPYSL3, PHGDH, TGFBR2, EFNB1, ELK3, PLAC8, OPRD1, TNF, F2, TNFRSF1A, INTU, NPPA, NOTCH3, SUMO1, CERNA3
-
Intraoral Dental Sinus
Wikipedia
Please help improve it to make it understandable to non-experts , without removing the technical details. ( July 2014 ) ( Learn how and when to remove this template message ) Intraoral dental sinus (also termed a parulis and commonly, a gumboil ) is an oral lesion characterized by a soft erythematous papule (red spot) that develops on the alveolar process in association with a non-vital tooth and accompanying dental abscess . [1] A parulis is made up of inflamed granulation tissue . Less commonly, dental infections drain onto the surface of the skin, forming a cutaneous sinus of dental origin . This condition is often resolved by endodontic treatment and does not have indication for antibiotic use. ... ISBN 978-1-4160-2999-1 . v t e Oral and maxillofacial pathology Lips Cheilitis Actinic Angular Plasma cell Cleft lip Congenital lip pit Eclabium Herpes labialis Macrocheilia Microcheilia Nasolabial cyst Sun poisoning Trumpeter's wart Tongue Ankyloglossia Black hairy tongue Caviar tongue Crenated tongue Cunnilingus tongue Fissured tongue Foliate papillitis Glossitis Geographic tongue Median rhomboid glossitis Transient lingual papillitis Glossoptosis Hypoglossia Lingual thyroid Macroglossia Microglossia Rhabdomyoma Palate Bednar's aphthae Cleft palate High-arched palate Palatal cysts of the newborn Inflammatory papillary hyperplasia Stomatitis nicotina Torus palatinus Oral mucosa – Lining of mouth Amalgam tattoo Angina bullosa haemorrhagica Behçet's disease Bohn's nodules Burning mouth syndrome Candidiasis Condyloma acuminatum Darier's disease Epulis fissuratum Erythema multiforme Erythroplakia Fibroma Giant-cell Focal epithelial hyperplasia Fordyce spots Hairy leukoplakia Hand, foot and mouth disease Hereditary benign intraepithelial dyskeratosis Herpangina Herpes zoster Intraoral dental sinus Leukoedema Leukoplakia Lichen planus Linea alba Lupus erythematosus Melanocytic nevus Melanocytic oral lesion Molluscum contagiosum Morsicatio buccarum Oral cancer Benign: Squamous cell papilloma Keratoacanthoma Malignant: Adenosquamous carcinoma Basaloid squamous carcinoma Mucosal melanoma Spindle cell carcinoma Squamous cell carcinoma Verrucous carcinoma Oral florid papillomatosis Oral melanosis Smoker's melanosis Pemphigoid Benign mucous membrane Pemphigus Plasmoacanthoma Stomatitis Aphthous Denture-related Herpetic Smokeless tobacco keratosis Submucous fibrosis Ulceration Riga–Fede disease Verruca vulgaris Verruciform xanthoma White sponge nevus Teeth ( pulp , dentin , enamel ) Amelogenesis imperfecta Ankylosis Anodontia Caries Early childhood caries Concrescence Failure of eruption of teeth Dens evaginatus Talon cusp Dentin dysplasia Dentin hypersensitivity Dentinogenesis imperfecta Dilaceration Discoloration Ectopic enamel Enamel hypocalcification Enamel hypoplasia Turner's hypoplasia Enamel pearl Fluorosis Fusion Gemination Hyperdontia Hypodontia Maxillary lateral incisor agenesis Impaction Wisdom tooth impaction Macrodontia Meth mouth Microdontia Odontogenic tumors Keratocystic odontogenic tumour Odontoma Dens in dente Open contact Premature eruption Neonatal teeth Pulp calcification Pulp stone Pulp canal obliteration Pulp necrosis Pulp polyp Pulpitis Regional odontodysplasia Resorption Shovel-shaped incisors Supernumerary root Taurodontism Trauma Avulsion Cracked tooth syndrome Vertical root fracture Occlusal Tooth loss Edentulism Tooth wear Abrasion Abfraction Acid erosion Attrition Periodontium ( gingiva , periodontal ligament , cementum , alveolus ) – Gums and tooth-supporting structures Cementicle Cementoblastoma Gigantiform Cementoma Eruption cyst Epulis Pyogenic granuloma Congenital epulis Gingival enlargement Gingival cyst of the adult Gingival cyst of the newborn Gingivitis Desquamative Granulomatous Plasma cell Hereditary gingival fibromatosis Hypercementosis Hypocementosis Linear gingival erythema Necrotizing periodontal diseases Acute necrotizing ulcerative gingivitis Pericoronitis Peri-implantitis Periodontal abscess Periodontal trauma Periodontitis Aggressive As a manifestation of systemic disease Chronic Perio-endo lesion Teething Periapical, mandibular and maxillary hard tissues – Bones of jaws Agnathia Alveolar osteitis Buccal exostosis Cherubism Idiopathic osteosclerosis Mandibular fracture Microgenia Micrognathia Intraosseous cysts Odontogenic : periapical Dentigerous Buccal bifurcation Lateral periodontal Globulomaxillary Calcifying odontogenic Glandular odontogenic Non-odontogenic: Nasopalatine duct Median mandibular Median palatal Traumatic bone Osteoma Osteomyelitis Osteonecrosis Bisphosphonate-associated Neuralgia-inducing cavitational osteonecrosis Osteoradionecrosis Osteoporotic bone marrow defect Paget's disease of bone Periapical abscess Phoenix abscess Periapical periodontitis Stafne defect Torus mandibularis Temporomandibular joints , muscles of mastication and malocclusions – Jaw joints, chewing muscles and bite abnormalities Bruxism Condylar resorption Mandibular dislocation Malocclusion Crossbite Open bite Overbite Overeruption Overjet Prognathia Retrognathia Scissor bite Maxillary hypoplasia Temporomandibular joint dysfunction Salivary glands Benign lymphoepithelial lesion Ectopic salivary gland tissue Frey's syndrome HIV salivary gland disease Necrotizing sialometaplasia Mucocele Ranula Pneumoparotitis Salivary duct stricture Salivary gland aplasia Salivary gland atresia Salivary gland diverticulum Salivary gland fistula Salivary gland hyperplasia Salivary gland hypoplasia Salivary gland neoplasms Benign: Basal cell adenoma Canalicular adenoma Ductal papilloma Monomorphic adenoma Myoepithelioma Oncocytoma Papillary cystadenoma lymphomatosum Pleomorphic adenoma Sebaceous adenoma Malignant: Acinic cell carcinoma Adenocarcinoma Adenoid cystic carcinoma Carcinoma ex pleomorphic adenoma Lymphoma Mucoepidermoid carcinoma Sclerosing polycystic adenosis Sialadenitis Parotitis Chronic sclerosing sialadenitis Sialectasis Sialocele Sialodochitis Sialosis Sialolithiasis Sjögren's syndrome Orofacial soft tissues – Soft tissues around the mouth Actinomycosis Angioedema Basal cell carcinoma Cutaneous sinus of dental origin Cystic hygroma Gnathophyma Ludwig's angina Macrostomia Melkersson–Rosenthal syndrome Microstomia Noma Oral Crohn's disease Orofacial granulomatosis Perioral dermatitis Pyostomatitis vegetans Other Eagle syndrome Hemifacial hypertrophy Facial hemiatrophy Oral manifestations of systemic disease This article related to pathology is a stub .
-
Pott's Puffy Tumor
Wikipedia
The cause of vein thrombosis is explained by venous drainage of the frontal sinus, which occurs through diploic veins, which communicate with the dural venous plexus; septic thrombi can potentially evolve from foci within the frontal sinus and propagate through this venous system. This type of chronic osteomyelitis of the frontal bone is confused with acute sub-periosteal abscess of the frontal bone, which presents as a discrete collection over the frontal sinus. Although it can affect all ages, it is mostly found among teenagers and adolescents . ... Some cases have been seen in a context of intranasal substance abuse (cocaine, methamphetamine). Post-surgical: after frontal sinus reconstruction [4] Diagnosis [ edit ] Diagnosis is suspected clinically and is confirmed using cross sectional imaging of the sinuses and brain. ... At the very least, the abscess is trephined externally as an emergency. Any associated frontal sinus table fracture can be managed electively.
-
Primary Ciliary Dyskinesia
GeneReviews
Chest radiographs and/or chest CT to define distribution and severity of airway disease and bronchiectasis Pulmonary function tests (spirometry) to define severity of obstructive impairment Pulse oximetry, with overnight saturation studies if borderline Nasal congestion and/or sinus symptoms. Sinus imaging (sinus x-rays or preferably sinus CT examination) Chronic/recurrent ear infections. ... Lung transplantation has been performed in persons with end-stage lung disease. Nasal congestion and sinus infections. In some persons with extensive sinus disease, sinus surgery can facilitate drainage and relieve symptoms.DNAI1, DNAAF3, LRRC6, DNAH9, GAS8, CCDC103, CCDC114, CFAP300, CCDC65, CFAP298, GAS2L2, DNAH5, DNAH11, CCDC40, RSPH1, RSPH9, ZMYND10, CCDC39, RPGR, CCDC151, DNAI2, PIH1D3, DNAAF1, RSPH4A, DNAAF4, CFAP221, SPEF2, FOXJ1, ARMC4, DRC1, DNAH1, DNAJB13, DNAAF5, CCNO, STK36, SPAG1, DNAAF2, TTC25, DNAL1, RSPH3, OFD1, MCIDAS, HYDIN, RPGRIP1L, IFT122, LRRC56, INPP5E, CDR2, PCBD1, SLC22A5, AK7, CDR2L, NME8, CFTR, AGTPBP1, MBL2, NT5E, ETFDH, CDR1, WDR19, TUBB, KRT20, CMPK1, RBM45, IL23R, IBD5, CDON, COPD, NTM, TRAT1, POC1B, LINC01194, MBL3P, CMPK2, TRIM9, NOD2, ZIC4, PARP9, TEKT1, NME7, DNAH3, CHD7, CD276, PAG1, DNAH7, SCD5, WNK1, GORASP1, PCBP4, PNPLA2, RSPH6A, ACVR2B, POLL, HLA-DQA1, DNAH8, EIF4E, ERBB2, ETFA, FPR1, NR3C1, HLA-DRB1, SIT1, HSPA4, HSPA5, HSP90AA1, HTC2, ICAM1, IL6, DNAH6, CRP, CREBBP, CREB1, COX8A, AKR1C4, CEL, CDO1, CDKN2A, CD40, MS4A1, CD19, RUNX1T1, CAMP, CA8, C5AR1, BCL2, CXCL8, CXCR2, KIFC1, TP53, LDLRAP1, ACOT11, DPCD, ADRB2, SLC27A5, CBX1, POSTN, CREB3, KIAA0319, NME5, ZIC2, ZIC1, TXN, TPO, TNF, MLN, TCTE3, SYT1, SNRPB, SLC22A4, SDC1, CCL2, RFX1, RELA, OPN1LW, PTPRC, PROC, PPARG, NOTCH3, NCAM1, TRIM67
-
Junctional Rhythm
Wikipedia
Under normal conditions, the heart's sinoatrial node determines the rate by which the organ beats – in other words, it is the heart's "pacemaker". The electrical activity of sinus rhythm originates in the sinoatrial node and depolarizes the atria. Current then passes from the atria through the atrioventricular node and into the bundle of His , from which it travels along Purkinje fibers to reach and depolarize the ventricles. This sinus rhythm is important because it ensures that the heart's atria reliably contract before the ventricles. ... ISBN 9781582553955 . v t e Cardiovascular disease (heart) Ischaemic Coronary disease Coronary artery disease (CAD) Coronary artery aneurysm Spontaneous coronary artery dissection (SCAD) Coronary thrombosis Coronary vasospasm Myocardial bridge Active ischemia Angina pectoris Prinzmetal's angina Stable angina Acute coronary syndrome Myocardial infarction Unstable angina Sequelae hours Hibernating myocardium Myocardial stunning days Myocardial rupture weeks Aneurysm of heart / Ventricular aneurysm Dressler syndrome Layers Pericardium Pericarditis Acute Chronic / Constrictive Pericardial effusion Cardiac tamponade Hemopericardium Myocardium Myocarditis Chagas disease Cardiomyopathy Dilated Alcoholic Hypertrophic Tachycardia-induced Restrictive Loeffler endocarditis Cardiac amyloidosis Endocardial fibroelastosis Arrhythmogenic right ventricular dysplasia Endocardium / valves Endocarditis infective endocarditis Subacute bacterial endocarditis non-infective endocarditis Libman–Sacks endocarditis Nonbacterial thrombotic endocarditis Valves mitral regurgitation prolapse stenosis aortic stenosis insufficiency tricuspid stenosis insufficiency pulmonary stenosis insufficiency Conduction / arrhythmia Bradycardia Sinus bradycardia Sick sinus syndrome Heart block : Sinoatrial AV 1° 2° 3° Intraventricular Bundle branch block Right Left Left anterior fascicle Left posterior fascicle Bifascicular Trifascicular Adams–Stokes syndrome Tachycardia ( paroxysmal and sinus ) Supraventricular Atrial Multifocal Junctional AV nodal reentrant Junctional ectopic Ventricular Accelerated idioventricular rhythm Catecholaminergic polymorphic Torsades de pointes Premature contraction Atrial Junctional Ventricular Pre-excitation syndrome Lown–Ganong–Levine Wolff–Parkinson–White Flutter / fibrillation Atrial flutter Ventricular flutter Atrial fibrillation Familial Ventricular fibrillation Pacemaker Ectopic pacemaker / Ectopic beat Multifocal atrial tachycardia Pacemaker syndrome Parasystole Wandering atrial pacemaker Long QT syndrome Andersen–Tawil Jervell and Lange-Nielsen Romano–Ward Cardiac arrest Sudden cardiac death Asystole Pulseless electrical activity Sinoatrial arrest Other / ungrouped hexaxial reference system Right axis deviation Left axis deviation QT Short QT syndrome T T wave alternans ST Osborn wave ST elevation ST depression Strain pattern Cardiomegaly Ventricular hypertrophy Left Right / Cor pulmonale Atrial enlargement Left Right Athletic heart syndrome Other Cardiac fibrosis Heart failure Diastolic heart failure Cardiac asthma Rheumatic fever
-
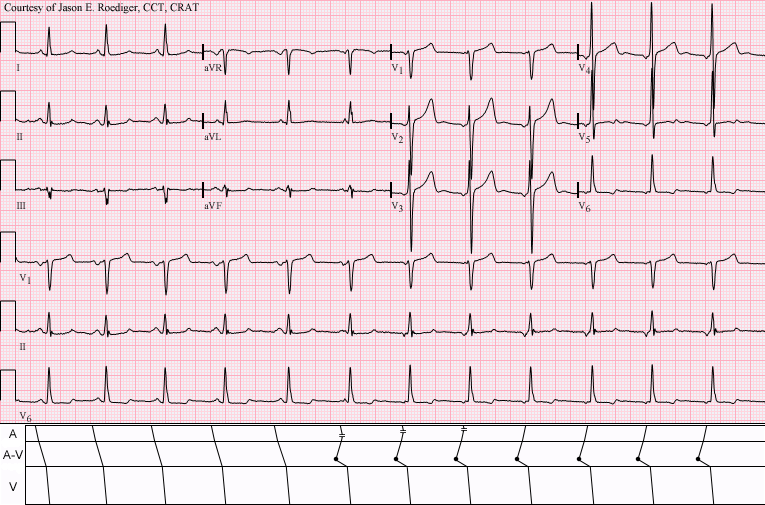
Automatic Tachycardia
Wikipedia
Automatic tachycardia Junctional tachycardia (rate about 115/min) dissociated from a slightly slower sinus tachycardia (rate about 107/min). ... This means that whereas a reentrant tachycardia will both begin and end abruptly as cardiac conduction utilises then ceases to utilise the accessory pathway, an automatic tachycardia will rise and fall gradually in rate as the automatic focus increases and decreases its automatic rate of electrical discharge. [1] Contents 1 Types 2 Treatment 3 See also 4 References Types [ edit ] Sinus tachycardia may be considered an automatic tachycardia, since the sinoatrial node (SAN) is discharging at an abnormally fast rate. ... Department of Anaesthesia and Intensive Care of The Chinese University of Hong Kong, Hong Kong 2016. v t e Cardiovascular disease (heart) Ischaemic Coronary disease Coronary artery disease (CAD) Coronary artery aneurysm Spontaneous coronary artery dissection (SCAD) Coronary thrombosis Coronary vasospasm Myocardial bridge Active ischemia Angina pectoris Prinzmetal's angina Stable angina Acute coronary syndrome Myocardial infarction Unstable angina Sequelae hours Hibernating myocardium Myocardial stunning days Myocardial rupture weeks Aneurysm of heart / Ventricular aneurysm Dressler syndrome Layers Pericardium Pericarditis Acute Chronic / Constrictive Pericardial effusion Cardiac tamponade Hemopericardium Myocardium Myocarditis Chagas disease Cardiomyopathy Dilated Alcoholic Hypertrophic Tachycardia-induced Restrictive Loeffler endocarditis Cardiac amyloidosis Endocardial fibroelastosis Arrhythmogenic right ventricular dysplasia Endocardium / valves Endocarditis infective endocarditis Subacute bacterial endocarditis non-infective endocarditis Libman–Sacks endocarditis Nonbacterial thrombotic endocarditis Valves mitral regurgitation prolapse stenosis aortic stenosis insufficiency tricuspid stenosis insufficiency pulmonary stenosis insufficiency Conduction / arrhythmia Bradycardia Sinus bradycardia Sick sinus syndrome Heart block : Sinoatrial AV 1° 2° 3° Intraventricular Bundle branch block Right Left Left anterior fascicle Left posterior fascicle Bifascicular Trifascicular Adams–Stokes syndrome Tachycardia ( paroxysmal and sinus ) Supraventricular Atrial Multifocal Junctional AV nodal reentrant Junctional ectopic Ventricular Accelerated idioventricular rhythm Catecholaminergic polymorphic Torsades de pointes Premature contraction Atrial Junctional Ventricular Pre-excitation syndrome Lown–Ganong–Levine Wolff–Parkinson–White Flutter / fibrillation Atrial flutter Ventricular flutter Atrial fibrillation Familial Ventricular fibrillation Pacemaker Ectopic pacemaker / Ectopic beat Multifocal atrial tachycardia Pacemaker syndrome Parasystole Wandering atrial pacemaker Long QT syndrome Andersen–Tawil Jervell and Lange-Nielsen Romano–Ward Cardiac arrest Sudden cardiac death Asystole Pulseless electrical activity Sinoatrial arrest Other / ungrouped hexaxial reference system Right axis deviation Left axis deviation QT Short QT syndrome T T wave alternans ST Osborn wave ST elevation ST depression Strain pattern Cardiomegaly Ventricular hypertrophy Left Right / Cor pulmonale Atrial enlargement Left Right Athletic heart syndrome Other Cardiac fibrosis Heart failure Diastolic heart failure Cardiac asthma Rheumatic fever
-
Chronic Atrial And Intestinal Dysrhythmia Syndrome
Orphanet
A rare genetic disease characterized by co-occurrence of sick sinus syndrome (manifesting as sinus bradycardia, often requiring pacemaker implantation) and chronic intestinal pseudo-obstruction (which may be of myogenic or neurogenic origin and usually requires total parenteral nutrition), with an age of onset within the first four decades of life.
-
Congenital Urachal Anomaly
Orphanet
Congenital urachal anomaly (CUA) describes a group of urachal remnants, found more frequently in males than females, that result from incomplete closure of the urachus (an embryological remnant of the allantois) during prenatal development, and that are usually asymptomatic (and found as an incidental finding on a radiological study) but can also present with umbilical discharge (in patent urachus or urachal sinus), infraumblical mass and pain, or with complications such as obstruction and infection. CUAs include patent urachus, urachal sinus, urachal cyst and urachal diverticulum (see these terms).
-
Wandering Atrial Pacemaker
Wikipedia
This shifting of the pacemaker from the SA node to adjacent tissues is identifiable on ECG Lead II by morphological changes in the P-wave ; sinus beats have smooth upright P waves, while atrial beats have flattened, notched, or diphasic P-waves. ... External links [ edit ] Classification D ICD - 9-CM : 427.89 v t e Cardiovascular disease (heart) Ischaemic Coronary disease Coronary artery disease (CAD) Coronary artery aneurysm Spontaneous coronary artery dissection (SCAD) Coronary thrombosis Coronary vasospasm Myocardial bridge Active ischemia Angina pectoris Prinzmetal's angina Stable angina Acute coronary syndrome Myocardial infarction Unstable angina Sequelae hours Hibernating myocardium Myocardial stunning days Myocardial rupture weeks Aneurysm of heart / Ventricular aneurysm Dressler syndrome Layers Pericardium Pericarditis Acute Chronic / Constrictive Pericardial effusion Cardiac tamponade Hemopericardium Myocardium Myocarditis Chagas disease Cardiomyopathy Dilated Alcoholic Hypertrophic Tachycardia-induced Restrictive Loeffler endocarditis Cardiac amyloidosis Endocardial fibroelastosis Arrhythmogenic right ventricular dysplasia Endocardium / valves Endocarditis infective endocarditis Subacute bacterial endocarditis non-infective endocarditis Libman–Sacks endocarditis Nonbacterial thrombotic endocarditis Valves mitral regurgitation prolapse stenosis aortic stenosis insufficiency tricuspid stenosis insufficiency pulmonary stenosis insufficiency Conduction / arrhythmia Bradycardia Sinus bradycardia Sick sinus syndrome Heart block : Sinoatrial AV 1° 2° 3° Intraventricular Bundle branch block Right Left Left anterior fascicle Left posterior fascicle Bifascicular Trifascicular Adams–Stokes syndrome Tachycardia ( paroxysmal and sinus ) Supraventricular Atrial Multifocal Junctional AV nodal reentrant Junctional ectopic Ventricular Accelerated idioventricular rhythm Catecholaminergic polymorphic Torsades de pointes Premature contraction Atrial Junctional Ventricular Pre-excitation syndrome Lown–Ganong–Levine Wolff–Parkinson–White Flutter / fibrillation Atrial flutter Ventricular flutter Atrial fibrillation Familial Ventricular fibrillation Pacemaker Ectopic pacemaker / Ectopic beat Multifocal atrial tachycardia Pacemaker syndrome Parasystole Wandering atrial pacemaker Long QT syndrome Andersen–Tawil Jervell and Lange-Nielsen Romano–Ward Cardiac arrest Sudden cardiac death Asystole Pulseless electrical activity Sinoatrial arrest Other / ungrouped hexaxial reference system Right axis deviation Left axis deviation QT Short QT syndrome T T wave alternans ST Osborn wave ST elevation ST depression Strain pattern Cardiomegaly Ventricular hypertrophy Left Right / Cor pulmonale Atrial enlargement Left Right Athletic heart syndrome Other Cardiac fibrosis Heart failure Diastolic heart failure Cardiac asthma Rheumatic fever
-
Language Delay And Attention Deficit-Hyperactivity Disorder/cognitive Impairment With Or Without Cardiac Arrhythmia
OMIM
Some patients develop cardiac arrhythmias reminiscent of sick sinus syndrome (summary by Lodder et al., 2016 and Shamseldin et al., 2016). ... Two Moroccan sibs, 13 and 8 years of age, presented in early childhood with sinus node dysfunction manifest as sinus bradycardia and sinus arrhythmia without structural heart abnormalities; one child required pacemaker implantation. ... A 23-year-old man, born of consanguineous Brazilian parents, had borderline to mild intellectual disability, keratoconus, and sinus arrhythmia. Shamseldin et al. (2016) reported a large consanguineous Saudi family in which 5 girls had severe language delay. ... INHERITANCE - Autosomal recessive CARDIOVASCULAR Heart - Sick sinus syndrome (in some patients) - Bradycardia (in some patients) - Arrhythmias (in some patients) MUSCLE, SOFT TISSUES - Hypotonia (in some patients) NEUROLOGIC Central Nervous System - Developmental delay (in some patients) - Intellectual disability (in some patients) - Speech delay - Impaired fine motor skills (in some patients) Behavioral Psychiatric Manifestations - Attention deficit - Hyperactivity MISCELLANEOUS - Onset in early childhood - Three unrelated families have been reported (last curated November 2016) MOLECULAR BASIS - Caused by mutation in the guanine nucleotide-binding protein, beta-5 gene (GNB5, 604447.0006 ) ▲ Close
-
Idiopathic Neonatal Atrial Flutter
Orphanet
AFL is sustained although conversion from atrial flutter to sinus rhythm may occur spontaneously (<24 hours). ... Management and treatment The first aim of treatment is the restoration of sinus rhythm. This is most easily achieved by transoesophageal overdrive pacing or synchronised low energy DC cardioversion using around 0.5-1 J/kg. ... Prognosis In the absence of additional arrhythmias, infants with AFL have an excellent prognosis once in sinus rhythm, with a low risk of recurrence, and chronic anti arrhythmic therapy is unlikely to be necessary.
-
Acute Infectious Thyroiditis
Wikipedia
Despite all this, a persistent fistula from the piriform sinus may make the left lobe of the thyroid susceptible to infection and abscess formation. [1] AIT is most often caused by a bacterial infection but can also be caused by a fungal or parasitic infection, most commonly in an immunocompromised host. ... The most common cause of infection in children is a congenital abnormality such as pyriform sinus fistula . [5] In most cases, the infection originates in the piriform sinus and spreads to the thyroid via the fistula. [8] In many reported cases of AIT the infection occurs following an upper respiratory tract infection . ... Repeated fine needle aspirates [1] Perforation of esophagus [4] Regional infection Diagnosis [ edit ] Patients who are suspected of having AIT often undergo tests to detect for elevated levels of white blood cells as well as an ultrasound to reveal unilobular swelling. [1] [4] Depending on the age and immune status of the patient more invasive procedures may be performed such as fine needle aspiration of the neck mass to facilitate a diagnosis. [4] In cases where the infection is thought to be associated with a sinus fistula it is often necessary to confirm the presence of the fistula through surgery or laryngoscopic examination. [6] While invasive procedures can often tell definitively whether or not a fistula is present, new studies are working on the use of computed tomography as a useful method to visualize and detect the presence of a sinus fistula. [6] Diagnostic tests [ edit ] Fever, redness, swelling Pain Blood tests of thyroid functions including TSH, T4 and T3 are usually normal [3] Ultrasonographic examination often shows the abscess or swelling in thyroid Gallium scan will be positive Barium swallow will show fistula connection to the piriform sinus and left lobe Elevated white blood cell count [3] Elevated erythrocyte sedimentation rate [3] Fine-needle aspiration Subtypes of thyroiditis [ edit ] Subtypes Causes Hashimoto's thyroiditis , Chronic lymphocytic thyroiditis, [3] Chronic autoimmune thyroiditis, Lymphadenoid goiter [5] Autoimmune [3] Subacute lymphocytic thyroiditis , Postpartum thyroiditis, Sporadic painless thyroiditis, [3] Silent sporadic thyroiditis [5] Autoimmune [3] Acute infectious thyroiditis, Microbial inflammatory thyroiditis, Suppurative thyroiditis, [3] Pyrogenic thyroiditis, Bacterial thyroiditis [5] Cause: Bacterial, Parasitic, Fungal [3] de Quervain's thyroiditis , Subacute granulomatous thyroiditis, [3] Giant-cell thyroiditis, Pseudogranulomatous thyroiditis, Painful subacute thyroiditis, [5] Viral [3] Riedel's thyroiditis , Riedel's struma, Invasive fibrous thyroiditis Unknown [3] Treatment [ edit ] Treatment of AIT involves antibiotic treatment. ... "Neck Infection Associated with Pyriform Sinus Fistula: Imaging Findings." American Journal of Neuroradiology Am J Neuroradiol 21 (2000): 817-22. ^ 3) Lazarus, John, and James Hennessey. ... New York: Elsevier, 1996 ^ Yamada, H., Fujita, K., Tokuriki, T., & Ishida, R. (2002). "Nine cases of piriform sinus fistula with acute suppurative thyroiditis."
-
Heart-Hand Syndrome, Spanish Type
OMIM
The cardiac defect was intraventricular conduction defect in 3 and sick sinus syndrome in 1. The brachydactyly affected mainly the middle phalanges; the index and fifth fingers were more severely affected than the others. ... Cardiac - Intraventricular conduction defect - Sick sinus syndrome Skel - Brachydactyly - Short middle phalanges, esp. index and fifth fingers - Ulnar deviation of index fingers Inheritance - Autosomal dominant ▲ Close
-
Congenital Lip Pit
Wikipedia
Congenital lip pit Specialty Oral & Maxillofacial Surgery Usual onset At birth Treatment Fistulectomy Prognosis Excellent A congenital lip pit or lip sinus is a congenital disorder characterized by the presence of pits and possibly associated fistulas in the lips. They are often hereditary, and may occur alone or in association with cleft lip and palate , termed Van der Woude syndrome . [1] Contents 1 Diagnosis 1.1 Classification 2 Treatment 3 See also 4 References 5 External links Diagnosis [ edit ] Classification [ edit ] They are divided into three types based on their location: [2] commissural pits, which are small pits near the labial commissure of the mouth , [3] a pit in the upper lip, in which case it may be called a midline sinus of the upper lip , [2] and pits in the lower lip, in which case it may be called a congenital sinus of the lower lip . [2] In some cases commissural pits have been reported in combination with preauricaluar pits , which are near the ear . [1] Treatment [ edit ] Lip pits are harmless and do not usually require any treatment, although in some reported cases surgical excision has been used or if associated with a draining sinus tract. [1] See also [ edit ] Skin dimple References [ edit ] ^ a b c Rajendran A; Sundaram S (10 February 2014). ... External links [ edit ] Classification D OMIM : 120500 v t e Oral and maxillofacial pathology Lips Cheilitis Actinic Angular Plasma cell Cleft lip Congenital lip pit Eclabium Herpes labialis Macrocheilia Microcheilia Nasolabial cyst Sun poisoning Trumpeter's wart Tongue Ankyloglossia Black hairy tongue Caviar tongue Crenated tongue Cunnilingus tongue Fissured tongue Foliate papillitis Glossitis Geographic tongue Median rhomboid glossitis Transient lingual papillitis Glossoptosis Hypoglossia Lingual thyroid Macroglossia Microglossia Rhabdomyoma Palate Bednar's aphthae Cleft palate High-arched palate Palatal cysts of the newborn Inflammatory papillary hyperplasia Stomatitis nicotina Torus palatinus Oral mucosa – Lining of mouth Amalgam tattoo Angina bullosa haemorrhagica Behçet's disease Bohn's nodules Burning mouth syndrome Candidiasis Condyloma acuminatum Darier's disease Epulis fissuratum Erythema multiforme Erythroplakia Fibroma Giant-cell Focal epithelial hyperplasia Fordyce spots Hairy leukoplakia Hand, foot and mouth disease Hereditary benign intraepithelial dyskeratosis Herpangina Herpes zoster Intraoral dental sinus Leukoedema Leukoplakia Lichen planus Linea alba Lupus erythematosus Melanocytic nevus Melanocytic oral lesion Molluscum contagiosum Morsicatio buccarum Oral cancer Benign: Squamous cell papilloma Keratoacanthoma Malignant: Adenosquamous carcinoma Basaloid squamous carcinoma Mucosal melanoma Spindle cell carcinoma Squamous cell carcinoma Verrucous carcinoma Oral florid papillomatosis Oral melanosis Smoker's melanosis Pemphigoid Benign mucous membrane Pemphigus Plasmoacanthoma Stomatitis Aphthous Denture-related Herpetic Smokeless tobacco keratosis Submucous fibrosis Ulceration Riga–Fede disease Verruca vulgaris Verruciform xanthoma White sponge nevus Teeth ( pulp , dentin , enamel ) Amelogenesis imperfecta Ankylosis Anodontia Caries Early childhood caries Concrescence Failure of eruption of teeth Dens evaginatus Talon cusp Dentin dysplasia Dentin hypersensitivity Dentinogenesis imperfecta Dilaceration Discoloration Ectopic enamel Enamel hypocalcification Enamel hypoplasia Turner's hypoplasia Enamel pearl Fluorosis Fusion Gemination Hyperdontia Hypodontia Maxillary lateral incisor agenesis Impaction Wisdom tooth impaction Macrodontia Meth mouth Microdontia Odontogenic tumors Keratocystic odontogenic tumour Odontoma Dens in dente Open contact Premature eruption Neonatal teeth Pulp calcification Pulp stone Pulp canal obliteration Pulp necrosis Pulp polyp Pulpitis Regional odontodysplasia Resorption Shovel-shaped incisors Supernumerary root Taurodontism Trauma Avulsion Cracked tooth syndrome Vertical root fracture Occlusal Tooth loss Edentulism Tooth wear Abrasion Abfraction Acid erosion Attrition Periodontium ( gingiva , periodontal ligament , cementum , alveolus ) – Gums and tooth-supporting structures Cementicle Cementoblastoma Gigantiform Cementoma Eruption cyst Epulis Pyogenic granuloma Congenital epulis Gingival enlargement Gingival cyst of the adult Gingival cyst of the newborn Gingivitis Desquamative Granulomatous Plasma cell Hereditary gingival fibromatosis Hypercementosis Hypocementosis Linear gingival erythema Necrotizing periodontal diseases Acute necrotizing ulcerative gingivitis Pericoronitis Peri-implantitis Periodontal abscess Periodontal trauma Periodontitis Aggressive As a manifestation of systemic disease Chronic Perio-endo lesion Teething Periapical, mandibular and maxillary hard tissues – Bones of jaws Agnathia Alveolar osteitis Buccal exostosis Cherubism Idiopathic osteosclerosis Mandibular fracture Microgenia Micrognathia Intraosseous cysts Odontogenic : periapical Dentigerous Buccal bifurcation Lateral periodontal Globulomaxillary Calcifying odontogenic Glandular odontogenic Non-odontogenic: Nasopalatine duct Median mandibular Median palatal Traumatic bone Osteoma Osteomyelitis Osteonecrosis Bisphosphonate-associated Neuralgia-inducing cavitational osteonecrosis Osteoradionecrosis Osteoporotic bone marrow defect Paget's disease of bone Periapical abscess Phoenix abscess Periapical periodontitis Stafne defect Torus mandibularis Temporomandibular joints , muscles of mastication and malocclusions – Jaw joints, chewing muscles and bite abnormalities Bruxism Condylar resorption Mandibular dislocation Malocclusion Crossbite Open bite Overbite Overeruption Overjet Prognathia Retrognathia Scissor bite Maxillary hypoplasia Temporomandibular joint dysfunction Salivary glands Benign lymphoepithelial lesion Ectopic salivary gland tissue Frey's syndrome HIV salivary gland disease Necrotizing sialometaplasia Mucocele Ranula Pneumoparotitis Salivary duct stricture Salivary gland aplasia Salivary gland atresia Salivary gland diverticulum Salivary gland fistula Salivary gland hyperplasia Salivary gland hypoplasia Salivary gland neoplasms Benign: Basal cell adenoma Canalicular adenoma Ductal papilloma Monomorphic adenoma Myoepithelioma Oncocytoma Papillary cystadenoma lymphomatosum Pleomorphic adenoma Sebaceous adenoma Malignant: Acinic cell carcinoma Adenocarcinoma Adenoid cystic carcinoma Carcinoma ex pleomorphic adenoma Lymphoma Mucoepidermoid carcinoma Sclerosing polycystic adenosis Sialadenitis Parotitis Chronic sclerosing sialadenitis Sialectasis Sialocele Sialodochitis Sialosis Sialolithiasis Sjögren's syndrome Orofacial soft tissues – Soft tissues around the mouth Actinomycosis Angioedema Basal cell carcinoma Cutaneous sinus of dental origin Cystic hygroma Gnathophyma Ludwig's angina Macrostomia Melkersson–Rosenthal syndrome Microstomia Noma Oral Crohn's disease Orofacial granulomatosis Perioral dermatitis Pyostomatitis vegetans Other Eagle syndrome Hemifacial hypertrophy Facial hemiatrophy Oral manifestations of systemic disease This dermatology article is a stub .
-
Aplasia Cutis Congenita With Intestinal Lymphangiectasia
OMIM
He died in shock at 2 months of age, after sudden profuse bleeding from the sagittal sinus. Neuro - Sagittal sinus bleeding Skull - Bony defect underlying ACC Inheritance - Autosomal recessive Lab - Hypoproteinemia Heme - Lymphopenia Skin - Aplasia cutis congenita of vertex - Generalized edema GI - Intestinal lymphangiectasia ▲ Close
-
Perifolliculitis Capitis Abscedens Et Suffodiens, Familial
OMIM
Description Perifolliculitis capitis abscedens et suffodiens is a chronic inflammatory disease of the scalp characterized by the presence of large and small nodules that suppurate and intercommunicate by sinus formation. It may be more frequent in black males than in others (summary by McMullan and Zeligman, 1956). ... INHERITANCE - Isolated cases SKIN, NAILS, & HAIR Skin - Suppurative scalp nodules - Scalp sinus formation - Small areas of alopecia - Scalp itching - S. epidermidis only microorganism isolated MISCELLANEOUS - Successful treatment with oral isotretinoin ▲ Close
-
Distichiasis With Congenital Anomalies Of The Heart And Peripheral Vasculature
OMIM
Two daughters had surgery for patent ductus arteriosus (see 607411). Sinus bradycardia alone (elder son), with stress-induced asystole (younger son), and with wandering atrial pacemaker (both daughters) were documented electrocardiographically. ... Hair - Double rows of eyelashes Cardiac - Congenital heart defect - Ventricular septal defect - Patent ductus arteriosus - Sinus bradycardia - Stress-induced asystole - Wandering atrial pacemaker Limbs - Leg edema - Varicose veins - Arterial disease of legs Inheritance - Autosomal dominant ▲ Close
-
Heart Block
Wikipedia
Conduction is initiated by the sinoatrial node ("sinus node" or "SA node"), and then travels to the atrioventricular node ("AV node") which also contains a secondary "pacemaker" that acts as a backup for the SA nodes, then to the bundle of His and then via the bundle branches to the point of the apex of the fascicular branches . ... Contents 1 Types 1.1 SA nodal blocks 1.2 AV nodal blocks 1.3 Infra-Hisian block 2 References 3 External links Types [ edit ] Conduction system of the heart Sinus rhythm with acute inferior infarction complicated by Type I AV block manifest in the form of 5:4 Wenckebach periods; R-P/P-R reciprocity. Sinus rhythm (rate = 100/min) with 3:2 and 2:1 Type II AV block; right bundle branch block Sinus tachycardia with complete AV block and resulting junctional escape Following the path of the electrical signals, the places where conduction can be blocked give rise to different kinds of heart blocks: Location Name Within the sinoatrial node (SA node or Sinus node), where the heart's signals originate Sinoatrial nodal blocks (often abbreviated "SA nodal block" or "SA block", sometimes written "Sinuatrial block") Within the atrioventricular node (AV node) Atrioventricular block (often abbreviated "AV nodal block", "AV block" or AVB). ... External links [ edit ] Classification D ICD - 10 : I44 - I45 ICD - 9-CM : 426.9 MeSH : D006327 DiseasesDB : 10477 v t e Cardiovascular disease (heart) Ischaemic Coronary disease Coronary artery disease (CAD) Coronary artery aneurysm Spontaneous coronary artery dissection (SCAD) Coronary thrombosis Coronary vasospasm Myocardial bridge Active ischemia Angina pectoris Prinzmetal's angina Stable angina Acute coronary syndrome Myocardial infarction Unstable angina Sequelae hours Hibernating myocardium Myocardial stunning days Myocardial rupture weeks Aneurysm of heart / Ventricular aneurysm Dressler syndrome Layers Pericardium Pericarditis Acute Chronic / Constrictive Pericardial effusion Cardiac tamponade Hemopericardium Myocardium Myocarditis Chagas disease Cardiomyopathy Dilated Alcoholic Hypertrophic Tachycardia-induced Restrictive Loeffler endocarditis Cardiac amyloidosis Endocardial fibroelastosis Arrhythmogenic right ventricular dysplasia Endocardium / valves Endocarditis infective endocarditis Subacute bacterial endocarditis non-infective endocarditis Libman–Sacks endocarditis Nonbacterial thrombotic endocarditis Valves mitral regurgitation prolapse stenosis aortic stenosis insufficiency tricuspid stenosis insufficiency pulmonary stenosis insufficiency Conduction / arrhythmia Bradycardia Sinus bradycardia Sick sinus syndrome Heart block : Sinoatrial AV 1° 2° 3° Intraventricular Bundle branch block Right Left Left anterior fascicle Left posterior fascicle Bifascicular Trifascicular Adams–Stokes syndrome Tachycardia ( paroxysmal and sinus ) Supraventricular Atrial Multifocal Junctional AV nodal reentrant Junctional ectopic Ventricular Accelerated idioventricular rhythm Catecholaminergic polymorphic Torsades de pointes Premature contraction Atrial Junctional Ventricular Pre-excitation syndrome Lown–Ganong–Levine Wolff–Parkinson–White Flutter / fibrillation Atrial flutter Ventricular flutter Atrial fibrillation Familial Ventricular fibrillation Pacemaker Ectopic pacemaker / Ectopic beat Multifocal atrial tachycardia Pacemaker syndrome Parasystole Wandering atrial pacemaker Long QT syndrome Andersen–Tawil Jervell and Lange-Nielsen Romano–Ward Cardiac arrest Sudden cardiac death Asystole Pulseless electrical activity Sinoatrial arrest Other / ungrouped hexaxial reference system Right axis deviation Left axis deviation QT Short QT syndrome T T wave alternans ST Osborn wave ST elevation ST depression Strain pattern Cardiomegaly Ventricular hypertrophy Left Right / Cor pulmonale Atrial enlargement Left Right Athletic heart syndrome Other Cardiac fibrosis Heart failure Diastolic heart failure Cardiac asthma Rheumatic fever
-
Lown–ganong–levine Syndrome
Wikipedia
Those with LGL syndrome have episodes of abnormal heart racing with a short PR interval and normal QRS complexes seen on their electrocardiogram when in a normal sinus rhythm . LGL syndrome was originally thought to be due to an abnormal electrical connection between the atria and the ventricles , but is now thought to be due to accelerated conduction through the atrioventricular node in the majority of cases. [1] The syndrome is named after Bernard Lown , William Francis Ganong, Jr. , and Samuel A. ... The only morbidity associated with the syndrome is the occurrence of paroxysmal episodes of tachycardia which may be of several types, including sinus tachycardia , atrioventricular nodal re-entrant tachycardia , atrial fibrillation , or atrial flutter . [4] See also [ edit ] Cardiac electrophysiology Electrocardiogram Electrophysiology study Premature ventricular contraction Wolff–Parkinson–White syndrome References [ edit ] ^ a b c d Josephson, Mark E. (2015-08-10). ... External links [ edit ] Classification D ICD - 10 : I45.6 ICD - 9-CM : 426.81 OMIM : 108950 MeSH : D008151 DiseasesDB : 7599 SNOMED CT : 55475008 External resources eMedicine : med/2954 Orphanet : 844 v t e Cardiovascular disease (heart) Ischaemic Coronary disease Coronary artery disease (CAD) Coronary artery aneurysm Spontaneous coronary artery dissection (SCAD) Coronary thrombosis Coronary vasospasm Myocardial bridge Active ischemia Angina pectoris Prinzmetal's angina Stable angina Acute coronary syndrome Myocardial infarction Unstable angina Sequelae hours Hibernating myocardium Myocardial stunning days Myocardial rupture weeks Aneurysm of heart / Ventricular aneurysm Dressler syndrome Layers Pericardium Pericarditis Acute Chronic / Constrictive Pericardial effusion Cardiac tamponade Hemopericardium Myocardium Myocarditis Chagas disease Cardiomyopathy Dilated Alcoholic Hypertrophic Tachycardia-induced Restrictive Loeffler endocarditis Cardiac amyloidosis Endocardial fibroelastosis Arrhythmogenic right ventricular dysplasia Endocardium / valves Endocarditis infective endocarditis Subacute bacterial endocarditis non-infective endocarditis Libman–Sacks endocarditis Nonbacterial thrombotic endocarditis Valves mitral regurgitation prolapse stenosis aortic stenosis insufficiency tricuspid stenosis insufficiency pulmonary stenosis insufficiency Conduction / arrhythmia Bradycardia Sinus bradycardia Sick sinus syndrome Heart block : Sinoatrial AV 1° 2° 3° Intraventricular Bundle branch block Right Left Left anterior fascicle Left posterior fascicle Bifascicular Trifascicular Adams–Stokes syndrome Tachycardia ( paroxysmal and sinus ) Supraventricular Atrial Multifocal Junctional AV nodal reentrant Junctional ectopic Ventricular Accelerated idioventricular rhythm Catecholaminergic polymorphic Torsades de pointes Premature contraction Atrial Junctional Ventricular Pre-excitation syndrome Lown–Ganong–Levine Wolff–Parkinson–White Flutter / fibrillation Atrial flutter Ventricular flutter Atrial fibrillation Familial Ventricular fibrillation Pacemaker Ectopic pacemaker / Ectopic beat Multifocal atrial tachycardia Pacemaker syndrome Parasystole Wandering atrial pacemaker Long QT syndrome Andersen–Tawil Jervell and Lange-Nielsen Romano–Ward Cardiac arrest Sudden cardiac death Asystole Pulseless electrical activity Sinoatrial arrest Other / ungrouped hexaxial reference system Right axis deviation Left axis deviation QT Short QT syndrome T T wave alternans ST Osborn wave ST elevation ST depression Strain pattern Cardiomegaly Ventricular hypertrophy Left Right / Cor pulmonale Atrial enlargement Left Right Athletic heart syndrome Other Cardiac fibrosis Heart failure Diastolic heart failure Cardiac asthma Rheumatic fever