-
Syne1 Deficiency
GeneReviews
Arthrogryposis multiplex congenita (AMC); neonatal hypotonia with decreased fetal movements resulting in distal joint contractures (including bilateral clubfoot, adducted thumbs, flexion contractures of fingers) followed by delayed motor milestones and progressive motor decline after the first decade [Attali et al 2009, Baumann et al 2017] Childhood onset. ... Pathogenic variants may include small intragenic deletions/insertions and missense, nonsense, and splice site variants; typically, exon or whole-gene deletions/duplications are not detected. ... Motor milestones are delayed, followed by progressive motor decline after the first decade. Patients use the Gower maneuver when arising from a squatting position and have limited ability to ambulate independently and to alternate their feet when climbing stairs. ... Disorders to Consider in the Differential Diagnosis of SYNE1 Deficiency View in own window MOI Disorder Gene 1 Clinical Features of Differential Diagnosis Disorder Overlapping w/SYNE1 Deficiency Distinguishing from SYNE1 Deficiency AR SCA-AR, 10 (SCAR10; ARCA3) (see Hereditary Ataxia Overview) ANO10 Very similar clinically Pure cerebellar ataxia w/occasional UMN signs Cognitive impairment Absence of polyneuropathy Marked cerebellar atrophy Seen mainly in Europe (whereas SYNE1 deficiency is seen worldwide) Primary coenzyme Q 10 deficiency (SCAR9; ARCA2) COQ8A Often a pure cerebellar ataxia phenotype w/cognitive impairment & cerebellar atrophy Exercise intolerance Epilepsy Myoclonus Occasional stroke-like cerebral lesions Absence of UMN &/or LMN signs Friedreich ataxia FXN Cerebellar ataxia Positive Babinski signs Sensory involvement w/spinal cord atrophy Abolished reflexes Square-wave jerks Hypertrophic cardiomyopathy Childhood to teenage onset Absence of cerebellar atrophy Boucher-Neuhäuser syndrome & PNPLA6 -related Gordon Holmes syndrome (see PNPLA6 -Related Disorders) PNPLA6 Cerebellar ataxia Spasticity Hyperreflexia Hypogonadotropic hypogonadism Chorioretinal dystrophy Childhood onset Pontine atrophy ARSACS (AR spastic ataxia of Charlevoix-Saguenay) SACS Ataxia Dysarthria Eye movement abnormalities UMN signs Seen worldwide but high prevalence in French Canadians Infantile or childhood onset Sensorimotor neuropathy Retinal striation Frequent mitral valve prolapse Spastic paraplegia 7 SPG7 Pyramidal signs w/spasticity Cerebellar ataxia w/cerebellar atrophy Spastic paraparesis more predominant Optic neuropathy Ptosis AD SCA3 ATXN3 Cerebellar ataxia UMN signs w/occasional amyotrophy & fasciculations Cognitive impairment Extrapyramidal features w/dystonia, rigidity, parkinsonism Progressive external ophthalmoparesis SCA6 CACNA1A Cerebellar ataxia w/adult onset & slow progression Occasional UMN signs Extrapyramidal features w/dystonia & blepharospasm XL Fragile X-associated tremor / ataxia syndrome (FXTAS) (see FMR1 -Related Disorders) FMR1 Cerebellar ataxia of adult onset Cognitive impairment Predominant tremor Parkinsonism MRI: White matter lesions in cerebellar peduncles & brain stem AD = autosomal dominant; AR = autosomal recessive; LMN = lower motor neuron; MOI = mode of inheritance; SCA = spinocerebellar ataxia; UMN = upper motor neuron; XL = X-linked 1.
-
Amusia
Wikipedia
It has been found that both amusia and aprosody can arise from seizures occurring in the non-dominant hemisphere. They can also both arise from lesions to the brain, as can Broca's aphasia come about simultaneously with amusia from injury. ... Gall mentioned a "musical organ" in a specific region of the human brain that could be spared or disrupted after a traumatic event resulting in brain damage. [40] In 1865, Jean-Baptiste Bouillaud described the first series of cases that involved the loss of music abilities that were due to brain injury. ... This model for music processing was the earliest produced. [41] While the possibility that certain individuals may be born with musical deficits is not a new notion, the first documented case of congenital amusia was published relatively recently. [22] The study was conducted with a female volunteer, referred to as Monica, who declared herself to be musically impaired in response to an advertisement in the newspaper. [22] Monica had no psychiatric or neurological history, nor did she have any hearing loss. ... Results showed that Monica could barely detect a pitch change as large as two semitones ( whole tone ), or half steps. [22] While this pitch-processing deficit is extremely severe, it does not seem to include speech intonation. [22] This is because pitch variations in speech are very coarse compared with those used in music. [2] In conclusion, Monica's learning disability arose from a basic problem in pitch discrimination, which is viewed as the origin of congenital amusia. [22] Treatment [ edit ] Currently, no forms of treatment have proven effective in treating amusia.
-
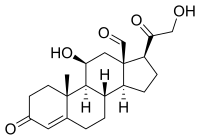
Pseudohypoaldosteronism
Wikipedia
Contents 1 Types 2 Presentation 3 Mechanism 4 Treatment 5 History 6 See also 7 References 8 External links Types [ edit ] Type OMIM Gene Inheritance Description PHA1A 177735 MLR Autosomal dominant with sodium wasting PHA1B 264350 SCNN1A , SCNN1B , SCNN1G of the epithelial sodium channel Autosomal recessive with sodium wasting PHA2 145260 WNK4 , WNK1 without sodium wasting. ... Alternatively, WNK4 mutations that result in a gain of function of the Na-Cl co-transporter may inhibit ROMK activity resulting in hyperkalemia. [4] Unlike in PHA1 in which aldosterone resistance is present, in PHA2 the volume expansion leads to relatively low aldosterone levels. [3] Treatment [ edit ] Treatment of severe forms of PHA1 requires relatively large amounts of sodium chloride . [5] These conditions also involve hyperkalemia . [6] In contrast, PHA2 (Gordon's syndrome) requires salt restriction and use of thiazide diuretics to block sodium chloride reabsorption and normalise blood pressure and serum potassium. [ citation needed ] History [ edit ] This syndrome was first described by Cheek and Perry in 1958. [7] Later pediatric endocrinologist Aaron Hanukoglu reported that there are two independent forms of PHA with different inheritance patterns: A renal form with autosomal dominant inheritance exhibiting salt loss mainly from the kidneys, and a multi-system form with autosomal recessive form exhibiting salt loss from kidney, lung, and sweat and salivary glands. [8] [9] The hereditary lack of responsiveness to aldosterone could be due to at least two possibilities: 1. ... External links [ edit ] GeneReviews/NCBI/NIH/UW entry on Pseudohypoaldosteronism Type II Classification D ICD - 10 : N25.8 OMIM : 177735 614495 614491 614496 614492 145260 264350 177735 614495 614491 614496 614492 145260 MeSH : D011546 External resources eMedicine : article/924100 Orphanet : 444916 v t e Adrenal gland disorder Hyperfunction Aldosterone Hyperaldosteronism Primary aldosteronism Conn syndrome Bartter syndrome Glucocorticoid remediable aldosteronism AME Liddle's syndrome 17α CAH Pseudohypoaldosteronism Cortisol Cushing's syndrome Pseudo-Cushing's syndrome Steroid-induced osteoporosis Sex hormones 21α CAH 11β CAH Hypofunction Aldosterone Hypoaldosteronism 21α CAH 11β CAH Cortisol CAH Lipoid 3β 11β 17α 21α Sex hormones 17α CAH Inborn errors of steroid metabolism Adrenal insufficiency Adrenal crisis Adrenalitis Xanthogranulomatous Addison's disease Waterhouse–Friderichsen syndrome v t e Kidney disease Glomerular disease See Template:Glomerular disease Tubules Renal tubular acidosis proximal distal Acute tubular necrosis Genetic Fanconi syndrome Bartter syndrome Gitelman syndrome Liddle's syndrome Interstitium Interstitial nephritis Pyelonephritis Balkan endemic nephropathy Vascular Renal artery stenosis Renal ischemia Hypertensive nephropathy Renovascular hypertension Renal cortical necrosis General syndromes Nephritis Nephrosis Renal failure Acute renal failure Chronic kidney disease Uremia Other Analgesic nephropathy Renal osteodystrophy Nephroptosis Abderhalden–Kaufmann–Lignac syndrome Diabetes insipidus Nephrogenic Renal papilla Renal papillary necrosis Major calyx / pelvis Hydronephrosis Pyonephrosis Reflux nephropathy v t e Genetic disorders relating to deficiencies of transcription factor or coregulators (1) Basic domains 1.2 Feingold syndrome Saethre–Chotzen syndrome 1.3 Tietz syndrome (2) Zinc finger DNA-binding domains 2.1 ( Intracellular receptor ): Thyroid hormone resistance Androgen insensitivity syndrome PAIS MAIS CAIS Kennedy's disease PHA1AD pseudohypoaldosteronism Estrogen insensitivity syndrome X-linked adrenal hypoplasia congenita MODY 1 Familial partial lipodystrophy 3 SF1 XY gonadal dysgenesis 2.2 Barakat syndrome Tricho–rhino–phalangeal syndrome 2.3 Greig cephalopolysyndactyly syndrome / Pallister–Hall syndrome Denys–Drash syndrome Duane-radial ray syndrome MODY 7 MRX 89 Townes–Brocks syndrome Acrocallosal syndrome Myotonic dystrophy 2 2.5 Autoimmune polyendocrine syndrome type 1 (3) Helix-turn-helix domains 3.1 ARX Ohtahara syndrome Lissencephaly X2 MNX1 Currarino syndrome HOXD13 SPD1 synpolydactyly PDX1 MODY 4 LMX1B Nail–patella syndrome MSX1 Tooth and nail syndrome OFC5 PITX2 Axenfeld syndrome 1 POU4F3 DFNA15 POU3F4 DFNX2 ZEB1 Posterior polymorphous corneal dystrophy Fuchs' dystrophy 3 ZEB2 Mowat–Wilson syndrome 3.2 PAX2 Papillorenal syndrome PAX3 Waardenburg syndrome 1&3 PAX4 MODY 9 PAX6 Gillespie syndrome Coloboma of optic nerve PAX8 Congenital hypothyroidism 2 PAX9 STHAG3 3.3 FOXC1 Axenfeld syndrome 3 Iridogoniodysgenesis, dominant type FOXC2 Lymphedema–distichiasis syndrome FOXE1 Bamforth–Lazarus syndrome FOXE3 Anterior segment mesenchymal dysgenesis FOXF1 ACD/MPV FOXI1 Enlarged vestibular aqueduct FOXL2 Premature ovarian failure 3 FOXP3 IPEX 3.5 IRF6 Van der Woude syndrome Popliteal pterygium syndrome (4) β-Scaffold factors with minor groove contacts 4.2 Hyperimmunoglobulin E syndrome 4.3 Holt–Oram syndrome Li–Fraumeni syndrome Ulnar–mammary syndrome 4.7 Campomelic dysplasia MODY 3 MODY 5 SF1 SRY XY gonadal dysgenesis Premature ovarian failure 7 SOX10 Waardenburg syndrome 4c Yemenite deaf-blind hypopigmentation syndrome 4.11 Cleidocranial dysostosis (0) Other transcription factors 0.6 Kabuki syndrome Ungrouped TCF4 Pitt–Hopkins syndrome ZFP57 TNDM1 TP63 Rapp–Hodgkin syndrome / Hay–Wells syndrome / Ectrodactyly–ectodermal dysplasia–cleft syndrome 3 / Limb–mammary syndrome / OFC8 Transcription coregulators Coactivator: CREBBP Rubinstein–Taybi syndrome Corepressor: HR ( Atrichia with papular lesions ) v t e Diseases of ion channels Calcium channel Voltage-gated CACNA1A Familial hemiplegic migraine 1 Episodic ataxia 2 Spinocerebellar ataxia type-6 CACNA1C Timothy syndrome Brugada syndrome 3 Long QT syndrome 8 CACNA1F Ocular albinism 2 CSNB2A CACNA1S Hypokalemic periodic paralysis 1 Thyrotoxic periodic paralysis 1 CACNB2 Brugada syndrome 4 Ligand gated RYR1 Malignant hyperthermia Central core disease RYR2 CPVT1 ARVD2 Sodium channel Voltage-gated SCN1A Familial hemiplegic migraine 3 GEFS+ 2 Febrile seizure 3A SCN1B Brugada syndrome 6 GEFS+ 1 SCN4A Hypokalemic periodic paralysis 2 Hyperkalemic periodic paralysis Paramyotonia congenita Potassium-aggravated myotonia SCN4B Long QT syndrome 10 SCN5A Brugada syndrome 1 Long QT syndrome 3 SCN9A Erythromelalgia Febrile seizure 3B Paroxysmal extreme pain disorder Congenital insensitivity to pain Constitutively active SCNN1B / SCNN1G Liddle's syndrome SCNN1A / SCNN1B / SCNN1G Pseudohypoaldosteronism 1AR Potassium channel Voltage-gated KCNA1 Episodic ataxia 1 KCNA5 Familial atrial fibrillation 7 KCNC3 Spinocerebellar ataxia type-13 KCNE1 Jervell and Lange-Nielsen syndrome Long QT syndrome 5 KCNE2 Long QT syndrome 6 KCNE3 Brugada syndrome 5 KCNH2 Short QT syndrome KCNQ1 Jervell and Lange-Nielsen syndrome Romano–Ward syndrome Short QT syndrome Long QT syndrome 1 Familial atrial fibrillation 3 KCNQ2 BFNS1 Inward-rectifier KCNJ1 Bartter syndrome 2 KCNJ2 Andersen–Tawil syndrome Long QT syndrome 7 Short QT syndrome KCNJ11 TNDM3 KCNJ18 Thyrotoxic periodic paralysis 2 Chloride channel CFTR Cystic fibrosis Congenital absence of the vas deferens CLCN1 Thomsen disease Myotonia congenita CLCN5 Dent's disease CLCN7 Osteopetrosis A2, B4 BEST1 Vitelliform macular dystrophy CLCNKB Bartter syndrome 3 TRP channel TRPC6 FSGS2 TRPML1 Mucolipidosis type IV Connexin GJA1 Oculodentodigital dysplasia Hallermann–Streiff syndrome Hypoplastic left heart syndrome GJB1 Charcot–Marie–Tooth disease X1 GJB2 Keratitis–ichthyosis–deafness syndrome Ichthyosis hystrix Bart–Pumphrey syndrome Vohwinkel syndrome ) GJB3 / GJB4 Erythrokeratodermia variabilis Progressive symmetric erythrokeratodermia GJB6 Clouston's hidrotic ectodermal dysplasia Porin AQP2 Nephrogenic diabetes insipidus 2 See also: ion channels v t e Deficiencies of intracellular signaling peptides and proteins GTP-binding protein regulators GTPase-activating protein Neurofibromatosis type I Watson syndrome Tuberous sclerosis Guanine nucleotide exchange factor Marinesco–Sjögren syndrome Aarskog–Scott syndrome Juvenile primary lateral sclerosis X-Linked mental retardation 1 G protein Heterotrimeic cAMP / GNAS1 : Pseudopseudohypoparathyroidism Progressive osseous heteroplasia Pseudohypoparathyroidism Albright's hereditary osteodystrophy McCune–Albright syndrome CGL 2 Monomeric RAS: HRAS Costello syndrome KRAS Noonan syndrome 3 KRAS Cardiofaciocutaneous syndrome RAB: RAB7 Charcot–Marie–Tooth disease RAB23 Carpenter syndrome RAB27 Griscelli syndrome type 2 RHO: RAC2 Neutrophil immunodeficiency syndrome ARF : SAR1B Chylomicron retention disease ARL13B Joubert syndrome 8 ARL6 Bardet–Biedl syndrome 3 MAP kinase Cardiofaciocutaneous syndrome Other kinase / phosphatase Tyrosine kinase BTK X-linked agammaglobulinemia ZAP70 ZAP70 deficiency Serine/threonine kinase RPS6KA3 Coffin-Lowry syndrome CHEK2 Li-Fraumeni syndrome 2 IKBKG Incontinentia pigmenti STK11 Peutz–Jeghers syndrome DMPK Myotonic dystrophy 1 ATR Seckel syndrome 1 GRK1 Oguchi disease 2 WNK4 / WNK1 Pseudohypoaldosteronism 2 Tyrosine phosphatase PTEN Bannayan–Riley–Ruvalcaba syndrome Lhermitte–Duclos disease Cowden syndrome Proteus-like syndrome MTM1 X-linked myotubular myopathy PTPN11 Noonan syndrome 1 LEOPARD syndrome Metachondromatosis Signal transducing adaptor proteins EDARADD EDARADD Hypohidrotic ectodermal dysplasia SH3BP2 Cherubism LDB3 Zaspopathy Other NF2 Neurofibromatosis type II NOTCH3 CADASIL PRKAR1A Carney complex PRKAG2 Wolff–Parkinson–White syndrome PRKCSH PRKCSH Polycystic liver disease XIAP XIAP2 See also intracellular signaling peptides and proteins
-
Chronic Lyme Disease
Wikipedia
All these factors have contributed to a great deal of public confusion with little appreciation of the serious harm caused to many patients who have received a misdiagnosis and have been inappropriately treated. [1] The 2008 documentary film Under Our Skin: The Untold Story of Lyme Disease opened June 19, 2009, in New York City. [51] The film, made by a director whose sister self-identified with the condition, is based on the premise that chronic Lyme disease exists. [52] A columnist for Entertainment Weekly wrote of the film: [ Under Our Skin ] embraces, with bits and pieces of skimpy evidence and a whole lot more paranoid leftist fervor, the notion that "chronic Lyme disease" is a condition that the medical establishment is locked in a conspiracy to deny the existence of. ... Retrieved 29 August 2015 . ^ http://www.tamatoledonews.com/page/content.detail/id/603916/Cornfileds--Common-Sense-and-Community.html?
-
Gonadotropin-Releasing Hormone Insensitivity
Wikipedia
Causes [ edit ] Congenital Causes Genetic Mutations Kallmann syndrome ANOS1 (formerly KAL1), X-linked recessive KS SOX10 (SRY-box 10 gene), autosomal dominant KS with variable penetrance IL17RD , autosomal dominant KS with variable penetrance SEMA3A , autosomal dominant KS with variable penetrance FEZF1 , autosomal recessive KS IL17RD , autosomal dominant KS with variable penetrance Digenic and Oligogenic Mutations A heterozygous FGFR1 mutation and heterozygous deletion in the NSMF gene in the anosmic pedigree A compound heterozygous GNRHR mutation and heterozygous FGFR1 mutation in the normosmic pedigree GnRH deficiency associated with mental retardation / obesity Congenital malformations often associated with craniofacial anomalies Laurence-Moon-Biedl syndrome Prader-Willi syndrome Acquired Causes Benign tumors and cysts Craniopharyngiomas Germinomas , meningiomas , gliomas , astrocytomas Metastatic tumors (breast, lung, prostate) Chronic systemic disease Malnutrition , anorexia nervosa , bulimia Hypothyroidism , hyperprolactinemia , diabetes mellitus , Cushing's disease Post-androgen abuse Infiltrative diseases Hemochromatosis Granulomatous diseases Histiocytosis Head trauma Pituitary apoplexy Drugs - marijuana , opioids , anabolic steroids Pathophysiology [ edit ] The genetic mechanisms of gonadotropin-releasing hormone (GnRH) insensitivity involve mutations in at least twenty-four genes regulating GnRH neuronal migration, secretion, and activity. ... Normal appearance of the hypothalamus and pituitary region on magnetic resonance imaging (MRI) ; when seeking this diagnosis, it is useful to request fine (1 mm) cuts through the olfactory bulb region of the MRI to define subtle abnormalities of the olfactory system that may signal which genetic tests to request first. Differential diagnosis — For patients fulfilling the above laboratory criteria, the main (and most difficult) differential diagnosis is with constitutional delay of growth and puberty (CDGP).
-
Copper Deficiency
Wikipedia
On the other hand, Menkes disease is a genetic disorder of copper deficiency involving a wide variety of symptoms that is often fatal. [4] Copper is required for the functioning of many enzymes, such as cytochrome c oxidase , which is complex IV in the mitochondrial electron transport chain , ceruloplasmin , Cu/Zn superoxide dismutase , and in amine oxidases . [2] These enzyme catalyze reactions for oxidative phosphorylation , iron transportation, antioxidant and free radical scavenging and neutralization, and neurotransmitter synthesis, respectively. [2] Diets vary in the amount of copper they contain, but may provide about 5 mg/day, of which only 20-50% is absorbed. [3] The diet of the elderly may have a lower copper content than the recommended daily intake. [3] Dietary copper can be found in whole grain cereals , legumes , oysters , organ meats (particularly liver ), cherries , dark chocolate , fruits , leafy green vegetables, nuts , poultry , prunes , and soybeans products like tofu . [5] Copper deficiency can have many hematological consequences, such as myelodysplasia , anemia , low white blood cell count , and low count of neutrophils (a type of white blood cell that is often called "the first line of defense" of the immune system). [3] Copper deficiency has long been known for as a cause of myelodysplasia (when a blood profile has indicators of possible future leukemia development), but it was not until 2001 that copper deficiency was associated with neurological manifestations like sensory ataxia (irregular coordination due to proprioceptive loss), spasticity, muscle weakness, and more rarely visual loss due to damage in the peripheral nerves , myelopathy (disease of the spinal cord), and rarely optic neuropathy . ... Unlike most cases of myelodysplastic syndrome, the bone marrow aspirate in copper deficiency characteristically shows cytoplasmic vacuoles within red and white cell precursors, and karyotyping in cases of copper deficiency does not reveal cytogenetic features characteristic of myelodysplastic syndrome. [6] [7] Anemia and neutropenia typically resolve within six weeks of copper replacement. [8] Neurological symptoms [ edit ] Copper deficiency can cause a wide variety of neurological problems including myelopathy , peripheral neuropathy , and optic neuropathy . [2] [7] Myelopathy [ edit ] Copper deficiency myelopathy in humans was discovered and first described by Schleper and Stuerenburg in 2001. [9] They described a patient with a history of gastrectomy and partial colonic resection who presented with severe tetraparesis and painful paraesthesias and who was found on imaging to have dorsomedial cervical cord T2 hyperintensity. ... The woman consumed over 600 coins, and started to show neurological symptoms such as unsteady gait and mild ataxia . [17] Hereditary disorders [ edit ] Menkes disease showing symptoms of the sparse, steel colored "kinky hair" and paleness Menkes disease is a congenital disease that is a cause of copper deficiency. [4] [7] [18] Menkes disease is a hereditary condition caused by a defective gene involved with the metabolism of copper in the body. [7] Menkes disease involves a wide variety of symptoms including floppy muscle tone, seizures , abnormally low temperatures, and a peculiar steel color hair that feels very rough. [4] [18] Menkes disease is usually a fatal disease with most children dying within the first ten years of life. [4] [18] Other [ edit ] It is rarely suggested that excess iron supplementation causes copper deficiency myelopathy . [2] Another rarer cause of copper deficiency is celiac disease , probably due to malabsorption in the intestines. [2] Still, a large percentage, around 20%, of cases have unknown causes. [2] Pathophysiology [ edit ] Copper functions as a prosthetic group, which permits electron transfers in key enzymatic pathways like the electron transport chain . [2] [3] [19] Copper is integrated in the enzymes cytochrome c oxidase , which is involved in cellular respiration and oxidative phosphorylation , Cu/Zn dismutase, which is involved in antioxidant defense, and many more listed in the table below. [3] Several Copper Dependent Enzymes and Their Function [2] Group Enzyme Function Oxidases Flavin -containing amine oxidase Metabolism of neurotransmitters: noradrenaline , dopamine , serotonin and some dietary amines Protein-lysine-6-oxidase ( lysyl oxidase ) Connective tissue synthesis- cross-linking of collagen and elastin Copper-containing amine oxidase (a family of enzymes which includes primary-amine oxidase and diamine oxidase ) Oxidation of biogenic amines including neurotransmitters , histamines , putrescine , cadaverine , and xenobiotic amines Cytochrome c oxidase Oxidative phosphorylation, electron transport in the mitochondrial membrane Superoxide dismutase (Cu/Zn dismutase) Antioxidant and free radical scavenger, oxidizes dangerous superoxides to safer hydrogen peroxide Ferroxidase I ( ceruloplasmin ) Iron transport-oxidation of Fe 2+ to Fe 3+ , copper storage and transport, antioxidant and free radical neutralizer Hephaestin (ferroxidase) Iron transport and oxidation of Fe 2+ to Fe 3+ in intestinal cells to enable iron uptake Monooxygenases Dopamine beta-monooxygenase Conversion of dopamine to norepinephrine Peptidylglycine monooxygenase Peptide hormone maturation- amidation of alpha-terminal carboxylic acid group of glycine Monophenol monooxygenase ( Tyrosinase ) Melanin synthesis Methylation Cycle Methionine synthase Transfer of methyl group from methyltetrahydrofolate to homocysteine to generate methionine for the methylation cycle and tetrahydrofolate for purine synthesis Adenosylhomocysteinase ( S-Adenosyl-L-homocysteine ) Regeneration of homocysteine from adenosylhomocyesteine ( S-Adenosyl-L-homocysteine ) in the methylation cycle Neurological [ edit ] Cytochrome c Oxidase mechanism in mitochondrial membrane Cytochrome c oxidase [ edit ] There have been several hypotheses about the role of copper and some of its neurological manifestations. ... On average, patients are diagnosed with copper deficiency around 1.1 years after their first symptoms are reported to a physician. [2] Copper deficiency can be treated with either oral copper supplementation or intravenous copper. [7] If zinc intoxication is present, discontinuation of zinc may be sufficient to restore copper levels back to normal, but this usually is a very slow process. [7] People who suffer from zinc intoxication will usually have to take copper supplements in addition to ceasing zinc consumption.
-
Eosinophilic Esophagitis
Wikipedia
Symptoms include swallowing difficulty , food impaction , vomiting, and heartburn . [3] Eosinophilic esophagitis was first described in children but also occurs in adults. ... Eosinophilic inflammation is not limited to the esophagus alone, and does extend through the whole gastrointestinal tract . Profoundly degranulated eosinophils may also be present, as may micro-abscesses and an expansion of the basal layer. [3] [10] Patients found to have signs of EoE on endoscopy should undergo an empiric 8-week trial of high-dose proton pump inhibitor therapy (twice daily) before repeat endoscopy in order to rule out GERD. [7] Although endoscopic findings are helpful in identifying patients with EoE, they are not diagnostic of the disease if the patient has no clinical symptoms. [7] [14] Esophageal mucosal biopsy [ edit ] Currently, endoscopic mucosal biopsy remains the most important diagnostic test for EoE, and is required to confirm the diagnosis. ... If remission is achieved, foods are slowly reintroduced. [21] Pharmacologic treatment [ edit ] In patients diagnosed with EoE, a trial of PPI 20 mg to 40 mg oral daily or twice daily as a first line therapy is a reasonable option. ... Systemic (oral) corticosteroids were one of the first treatment options shown to be effective in patients with EoE. ... It is possible that long-standing, untreated disease may result in esophageal remodeling, leading to strictures, Schatzki ring and, eventually, achalasia. [7] History [ edit ] The first case of eosinophilic esophagitis was reported in 1978. [1] In the early 1990s, it became recognized as a distinct disease. [25] See also [ edit ] Eosinophilic gastroenteritis References [ edit ] ^ a b Gómez-Aldana A, Jaramillo-Santos M, Delgado A, Jaramillo C, Lúquez-Mindiola A (August 2019).TSLP, CAPN14, TRIM8, TNK2, STAT6, JAZF1, EMSY, CCL26, IL13, IFFO2, HSF2BP, LINC02588, ANKRD27, CCDC81, MEAK7, SHROOM3, KIF17, IL5, CLEC16A, DCC, TIMP2, P2RX6, LINC02240, XKR6, CAPN5, CEP295NL, TGFB1, POSTN, FLG, TNF, DSG1, IL33, CCL11, FOXP3, ATP12A, ATP4A, IL4, IL6, IL15, EPC2, SPINK7, WDR36, CLDN7, CPA3, SIGLEC8, MID1, IL18, TNFSF10, SOAT1, EPX, CLDN1, DHTKD1, RNASE2, IL9, FFAR3, ALOX15, BDNF, IL18R1, COPD, LOC283710, IL32, IL1RL1, SLC9C2, SERPINA13P, MIR223, SPAG9, NR1I2, OGDHL, DEFB103A, FST, TNFRSF14, MIR375, EMBP1, BECN1, ABCB11, DEFB4B, BANCR, EOS, CBLL2, RSAD2, TRPV1, HBS1L, DEFB103B, CRLF2, ANO1, OXR1, SLC52A1, RHOF, TLR9, BCL11A, KLF13, CPA4, MUL1, LRRC31, CHIA, ACAD8, PANK2, MAPK8IP2, FIP1L1, SYNPO, PTGDR2, SERPINB12, SPINK5, REEP5, AGA, VCAM1, GFER, ESR2, F2RL1, FGF9, FKBP4, FKBP5, GABPA, LRRC32, GJA1, DNM1, GRM5, HIF1A, ICAM1, IFNG, IL1A, IL1B, IL5RA, ESR1, DEFB4A, TYK2, CD1D, ALOX5, ANXA5, CCND1, BID, BNIP3, CALB2, CAMP, CD44, CYP2C19, CEACAM8, CLC, CCR3, CCR8, ABCC2, COL8A2, CSF2, IL9R, IL15RA, ITGAM, CCL18, KLK6, PTGDR, PTGS2, RNASE3, S100A7, SAFB, CCL2, SGSH, KCNJ2, AGXT, SPRR3, STAT1, STC1, TFDP1, TLR3, TNFRSF4, KLK7, PRG2, PTPA, PLG, LALBA, LCT, LOX, LTC4S, SMAD2, KITLG, MIF, MMP2, MMP14, MPG, MYB, NFE2L2, SLC22A18, OSM, PRKN, SLC9A3
-
Pulmonary Venoocclusive Disease 1, Autosomal Dominant
OMIM
In a cohort of 48 patients with PPH, 24 of whom had histologic evidence of PVOD, Montani et al. (2008) identified mutations in the BMPR2 gene in 2 patients with PVOD (600799.0027 and 600799.0028) and in 4 patients with no evidence of PVOD. INHERITANCE - Autosomal dominant CARDIOVASCULAR Heart - Prominent second heart sound Vascular - Elevated jugular venous pressure - Pulmonary arterial hypertension RESPIRATORY Lung - Pulmonary veno-occlusive disease seen on biopsy - Centrilobular ground glass opacities seen on CT - Thickened interlobular septae seen on CT - Occult alveolar hemorrhage MISCELLANEOUS - Variable clinical presentation MOLECULAR BASIS - Caused by mutation in the bone morphogenetic receptor, type II gene (BMPR2, 600799.0001 ) ▲ Close
-
Cornea Plana 2, Autosomal Recessive
OMIM
Clinical Features Eriksson et al. (1973) pointed out that the autosomal recessive form of CNA has more severe manifestations than the dominant form (CNA1; 121400) in terms of reduced visual activity, extreme hyperopia (usually +10 diopters (D) or more), hazy corneal limbus, opacities in the corneal parenchyma, and marked arcus senilis (often detected at an early age). Tahvanainen et al. (1996) noted that a round and opaque thickening, approximately 5 mm wide and located centrally, occurs in most cases of the recessive form but never in the dominant form. Additional anomalies such as malformations of the iris, a slit-like pupil, and adhesions between the iris and cornea are more prevalent in the recessive form. Tahvanainen et al. (1996) compared dominant and recessive forms of cornea plana in the Finnish population by measuring horizontal corneal refraction values in diopters. ... Although the 12q region was excluded as the site of the mutation in 2 Finnish families with autosomal dominant cornea plana (CNA1) by Tahvanainen et al. (1996), Tahvanainen et al. (1996) described a Cuban pedigree in which dominantly inherited cornea plana was linked to the same region of 12q in which the recessive form is located.
-
Chorea, Benign Hereditary
OMIM
Other regions of the brain showed nonspecific astrocytosis without noticeable neuronal loss. Inheritance Possible dominant inheritance of BHC was demonstrated in 2 families by Chun et al. (1973). Harper (1978) favored autosomal dominant inheritance with reduced penetrance in females. ... Furthermore, X-linked inheritance appears to be excluded by the apparent transmission through an unaffected male in the family of Pincus and Chutorian (1967). Both a dominant and a recessive form (215450) may exist. ... Nomenclature Schady and Meara (1988) discussed the use of the label 'benign' and concurred with Behan and Bone (1977) that the most accurate term was 'hereditary chorea without dementia.' INHERITANCE - Autosomal dominant NEUROLOGIC Central Nervous System - Chorea - Delayed motor development - Dysarthria may occur - Gait abnormalities may occur - Movements are exacerbated by anxiety - Severity of symptoms peak in the second decade and do not progress - No dementia - Mildly decreased intelligence has been reported MISCELLANEOUS - Variable phenotype - Onset in childhood (usually before age 5 years) - Allelic disorder to choreoathetosis, congenital hypothyroidism, and neonatal respiratory distress ( 610978 ), which is a more severe disorder MOLECULAR BASIS - Caused by mutation in the thyroid transcription factor-1 gene (TITF1, 600635.0001 ) ▲ Close
-
Tango2-Related Metabolic Encephalopathy And Arrhythmias
GeneReviews
Individuals can present with intermittent acute episodes of rhabdomyolysis. The first episode of myoglobinuria has been known to occur as early as age five months. ... Variants may include small intragenic deletions/insertions and missense, nonsense, and splice site variants; typically, exon or whole-gene deletions/duplications are not detected. ... Dark urine due to myoglobinuria and profound lower-extremity weakness can develop. The first episode of myoglobinuria has been known to occur as early as age five months. ... Baseline gait incoordination, progressively unsteady gait, difficulty with speech, or clumsiness is frequently reported in ambulatory individuals, even prior to the first episode of acute myoglobinuria. ... If systolic function is severely depressed, continue magnesium as first-line treatment. Death due to refractory arrhythmias has occurred despite treatment; thus ECMO should be considered for support through metabolic crises.
-
Rinderpest
Wikipedia
This policy was not very popular and used only sparingly in the first part of the century. Later, it was used successfully in several countries, although it was sometimes seen as too costly or drastic, and depended on a strong central authority to be effective (which was notably lacking in the Dutch Republic ). ... Their experiments confirmed the concepts of those who saw infectious diseases as caused by specific agents, and were the first to recognize maternally derived immunity . [11] Early English experimentation [ edit ] The first written report of rinderpest inoculation was published in a letter signed "T.S." in the November 1754 issue of The Gentleman's Magazine , [11] a widely read journal which also supported the progress of smallpox inoculation. ... These letters encouraged further application of inoculation in the fight against diseases. The first inoculation against measles was made three years after their publication. [11] From early 1755 onwards, experiments were taking place in the Netherlands, as well, results of which were also published in The Gentleman's Magazine . ... Although they were not able to perfect the inoculation procedure, they did make some useful observations. [11] Reinders resumed his experiments in 1774, concentrating on the inoculation of calves from cows that had recovered from rinderpest. He was probably the first to make practical use of maternally derived immunity . [11] The detailed results of his trials were published in 1776 and reprinted in 1777. ... Sometimes this could be done with minimal sacrifices; at other times, it required slaughter at a massive scale. [11] 19th century [ edit ] Cows dead from rinderpest in South Africa, 1896 A major outbreak affected the whole of the British Isles for three years after 1865. [19] Around the turn of the century, a plague struck in Southern Africa. [19] The outbreak in the 1890s killed an estimated 80 to 90% of all cattle in eastern and southern Africa, as well as in the Horn of Africa .
-
Tfr2-Related Hereditary Hemochromatosis
GeneReviews
Sequence analysis of TFR2 is performed first and followed by gene-targeted deletion/duplication analysis if only one or no pathogenic variant is found. ... Pathogenic variants may include small intragenic deletions/insertions and missense, nonsense, and splice site variants; typically, exon or whole-gene deletions/duplications are not detected. ... Primary Iron Overload Disorders to Consider in the Differential Diagnosis of TFR2 -HHC View in own window Disorder 1 Gene(s) MOI Clinical Features of This Disorder Overlapping with TFR2 -HHC Distinguishing from TRF2 -HHC HFE -related hereditary hemochromatosis HFE AR Biochemical & clinical features of iron overload Lower penetrance Later onset Juvenile hereditary hemochromatosis HJV HAMP AR Biochemical & clinical features of iron overload Full penetrance Earlier onset More severe clinical manifestations, esp cardiomyopathy & hypogonadism Ferroportin 1-associated hemochromatosis (OMIM 606069) SLC40A1 AD Biochemical & clinical features of iron overload Later-onset clinical manifestations of iron overload Ferroportin disease 2 SLC40A1 AD Hyperferritinemia At early stage: anemia & low transferrin saturation Iron deposition in hepatic reticuloendothelial (not parenchymal) cells Reduced tolerance to phlebotomy Aceruloplasminemia CP AR Hyperferritinemia Diabetes mellitus Anemia Iron deposition in hepatic reticuloendothelial (not parenchymal) cells Brain iron accumulation manifesting as retinal degeneration & neurologic disease (movement disorders & ataxia) African iron overload (OMIM 601195) Unknown Liver iron accumulation in reticuloendothelial & parenchymal cells Cirrhosis In drinkers of beer brewed in non-galvanized steel drums Lower frequency of cardiomyopathy & diabetes Susceptibility to tuberculosis & other infections Neonatal hemochromatosis (congenital alloimmune hepatitis) (OMIM 231100) Unknown Iron deposition in multiple organs (liver, pancreas, heart, endocrine glands) Alloimmune pathogenesis Iron overload in fetus Severe liver failure at birth, often fatal without liver transplant Bmp6-related iron overload (OMIM 112266) BMP6 AD Biochemical features of iron overload Liver iron accumulation Normal transferrin saturation in some Mild-to-moderate late onset of iron overload AD = autosomal dominant; AR = autosomal recessive; MOI = mode of inheritance 1.
-
Paracoccidioidomycosis
Wikipedia
Most of the remaining infections are in Argentina, Colombia and Venezuela. [16] Most epidemiological reports have focused on P. brasliensis , with P. lutzii epidemiology poorly understood as of 2015. [16] Rising cases have been linked to agriculturalization and deforestation in Brazil, urbanisation to peripheral city areas with poor infrastructure, as well as increased soil and air humidity. [9] [16] One Brazilian indigenous tribe, the Surui, after changing from substitience agriculture to coffee farming showed higher infection rates than surrounding tribes. [16] There have also been reports in non-endemic areas with the rise of eco-tourism, in the United States, Europe and Japan. [11] All reported cases were returned travellers from endemic regions. [16] History [ edit ] Lutz-Splendore-de Almeida disease [2] is named for the physicians Adolfo Lutz , [21] Alfonso Splendor (1871–1953), an Italo-Brazilian Parasitologist [22] and Floriano Paulo de Almeida (1898–1977), a Brazilian Pathologist specializing in Pathologic Mycology (Study of Infectious Fungi), [23] [24] who first characterized the disease in Brazil in the early 20th century. ... Melhoramentos (in Portuguese), São Paulo: 98 pages External links [ edit ] Classification D ICD - 10 : B41 ICD - 9-CM : 116.1 MeSH : D010229 DiseasesDB : 29815 External resources eMedicine : med/1731 Orphanet : 73260 v t e Fungal infection and mesomycetozoea Superficial and cutaneous ( dermatomycosis ): Tinea = skin ; Piedra ( exothrix / endothrix ) = hair Ascomycota Dermatophyte ( Dermatophytosis ) By location Tinea barbae / tinea capitis Kerion Tinea corporis Ringworm Dermatophytids Tinea cruris Tinea manuum Tinea pedis (athlete's foot) Tinea unguium/onychomycosis White superficial onychomycosis Distal subungual onychomycosis Proximal subungual onychomycosis Tinea corporis gladiatorum Tinea faciei Tinea imbricata Tinea incognito Favus By organism Epidermophyton floccosum Microsporum canis Microsporum audouinii Trichophyton interdigitale/mentagrophytes Trichophyton tonsurans Trichophyton schoenleini Trichophyton rubrum Trichophyton verrucosum Other Hortaea werneckii Tinea nigra Piedraia hortae Black piedra Basidiomycota Malassezia furfur Tinea versicolor Pityrosporum folliculitis Trichosporon White piedra Subcutaneous , systemic , and opportunistic Ascomycota Dimorphic (yeast+mold) Onygenales Coccidioides immitis / Coccidioides posadasii Coccidioidomycosis Disseminated coccidioidomycosis Primary cutaneous coccidioidomycosis .IFNG, IL10, TNF, IL4, CTLA4, S100A10, HSPD1, CD40LG, EXOSC3, HSPA14, TPI1, VDR, CHST3, TUBA1B, IL37, PYCARD, CD209, NLRP3, RBM45, TLR5, IL23A, YTHDF1, NLN, CLEC7A, LPAL2, IL33, OPN4, APOA2, SFTPD, TLR3, ICAM1, TSPO, CD28, CHRM3, FCGR2A, G6PD, GPI, GSR, HLA-DRB1, IL12B, STAT4, IL12RB1, IL17A, LGALS3, NOS2, NOTCH1, OPRM1, STS, STAT3, IL23R
-
Muscle Weakness
Wikipedia
"Finding May Solve Riddle of Fatigue in Muscles" . The New York Times . ^ Page 59 in: Hugue Ouellette (2008). Orthopedics Made Ridiculously Simple (Medmaster Ridiculously Simple) (Medmaster Ridiculously Simple) . ... ISBN 978-0-940780-86-6 . ^ Neurologic Examination Archived 2009-05-11 at the Wayback Machine at First Year Medical Curriculum at University of Florida College of Medicine.DMD, PMP22, AMPD1, GYG1, TBCD, MYOT, TTN, CSF3, CSF2, CAMKMT, SMN1, DES, SOD1, LMNA, VCP, FLNC, ETFDH, FBN1, IFIH1, CACNA1A, HLA-DRB1, MYH3, SYNE1, CLCN1, FGF23, TRNL1, FKTN, KCNJ11, DMPK, MSTO1, MPZ, ACAD9, AGL, DAG1, COL6A2, LRP4, TNFRSF11B, ALS2, TMEM126B, TTR, TOR1AIP1, TP53, SPTA1, SPG7, PROK2, SPP1, SPR, TRMT5, SNAP25, ACADVL, SPTB, SCNN1B, CEP126, SCNN1A, SDHA, SFRP4, SPARC, SDHD, SMPD1, SLC25A19, SLC4A1, SLC12A3, SLC34A1, HAMP, SLC22A5, SOX10, SMARCB1, SOS2, SOS1, SMN2, PTPN22, SARS1, SCN4A, PGK1, PMM2, PML, PLP1, FKRP, CDC73, PIGA, PHKB, PHKA1, PGM1, PFN1, PPOX, PFKM, PEX13, PEX7, SLC26A4, TBL1XR1, PDCD1, PDE11A, ARMC5, NUMA1, SLC25A24, CPLANE1, ATXN7, RAF1, XYLT2, POMT2, RYR1, RRAS, RPS6KA3, RIT1, IRF2BPL, RASA2, RARA, ALDH18A1, NABP1, PEX5, PTPN11, PSMB8, PSAP, PRPS1, PRPH, PRNP, PRKAR1A, PRKACA, TWNK, TGFB1, STAT3, STAT4, POLR3A, B4GAT1, AFG3L2, SEPTIN9, IL17RD, POMT1, CNNM2, TRPM7, SEMA3A, APTX, WARS2, QRICH1, TFG, RXYLT1, KLHL41, COQ7, OPTN, TSFM, SCO2, ERLIN2, SCN11A, EXOSC8, ISCU, NSMF, NDUFAF3, RTTN, SEPSECS, FLRT3, ABHD5, PIK3R5, KAT6B, ACTL6B, MRAS, ATP13A2, TRIM2, BICD2, AGTPBP1, LPIN1, ADA2, DPM3, MORC2, BCOR, TTC19, ADPRS, TSHR, AAAS, PAX8, ZBTB16, TMEM165, XK, VRK1, TTPA, NRAS, TRH, AGK, NKX2-1, TCN2, MLX, GMPPB, TACR3, SURF1, ABCC8, STAT5B, LZTR1, WDR11, DARS2, AIFM1, PREPL, POMGNT1, NFU1, HS6ST1, CHD7, TRIP4, LARGE1, SLC33A1, SLC7A7, CASK, LIMS2, ASCC1, CCN6, FGF17, HESX1, PEX11B, TRMU, PDE8B, SCNN1G, PNPLA8, HLA-DQB1, A2ML1, GCK, GCH1, GBE1, B4GALNT1, BTD, NPM1, TANGO2, FXN, FMR1, FOXE1, CHCHD10, FOXC2, C1QA, C1R, FGFR1, FGF8, DNAJC19, PROKR2, BRCA2, SYT2, SLC25A26, FDX2, ATP5F1D, HMBS, FAM111B, ATP7A, HLA-B, HEXB, CYP2R1, GJA1, SDHAF1, HBB, BCS1L, GPI, GNAS, BRAF, CCDC78, SLC34A3, EXT2, IFRD1, EXT1, CPT2, CAPN3, CCDC141, FEZF1, COL12A1, CAV1, COL6A1, COL5A2, COL5A1, COL4A1, COL1A1, CFL2, CCR6, CLCNKB, ERCC8, CHRND, CHRNB1, STAC3, SLC25A20, NKX2-5, CACNA1S, ETFB, ETFA, ERCC6, EPB42, HJV, B3GALNT2, DUSP6, C9orf72, CCN2, DCTN1, DCC, CYP27B1, CYP27A1, RNASEH1, CYP11B2, CYP11B1, HSPG2, IRF2BP2, ND5, MPV17, COX1, COX2, NDP, COX3, MTHFR, ANK1, ND1, ND2, ND3, NBN, ND4, NAGA, ND6, MYO9A, TRNE, TRNF, TRNH, TRNI, TRNK, C19orf12, POMK, ACTB, TRNP, ACY1, TRNQ, ALAS2, TRNS1, TRNS2, TRNT, TRNW, ATP6, TUBB6, KCNJ18, TIMM50, C12orf65, SLC25A46, LYRM7, IL12B, INS, PDX1, IRAK1, IRF5, ATP1A3, ITGA7, FIP1L1, D2HGDH, ANOS1, NF1, POMGNT2, KCNJ5, MECP2, NDUFB8, NDUFS2, NEFH, KISS1R, CRPPA, SPRY4, NEU1, L1CAM, ARSA, KRAS, TRNV, STMN1, SNURF, SNRPN, ACTA1, TPM2, NEB, GAA, SI, MYH7, DYSF, TPM3, MGAM, FHL1, ANO5, SGCA, AR, MB, IMMT, POLG, KIF1B, PABPN1, ACHE, DOK7, MYH2, ALB, IGF1, CAV3, AQP4, BIN1, PAX7, RAB7A, BEST1, MTM1, HMGCR, STIM1, GFPT1, LAMA2, UTRN, PIK3C2A, SELENON, DNM2, CRYAB, MYH8, COL13A1, GNE, ZMPSTE24, ACE2, MTMR14, NT5C1A, PIEZO2, AGRN, FSD1L, TNS3, YARS2, FSD1, TNFAIP8L2, SOST, MYPN, CHST14, SLC5A7, ALG2, TLR7, TAOK3, HCN1, ADSS1, PTRH2, PLF, PRMT8, ZC4H2, COPD, PLEKHM3, GLDN, WLS, ACADM, NOX4, FUS, GH1, GJB1, GSK3B, HDAC2, HEXA, HLA-DQA1, HSPB1, IGFALS, IGFBP1, IGHMBP2, IL2RA, ISG20, KCNH2, LEP, MAP6, MET, MIP, TRNM, MUSK, MYBPC1, NEFL, NOTCH1, NPTX2, MSTN, FES, OPA1, FBN2, SLC25A4, APP, ASAH1, BCL2, BRCA1, BTF3P11, CAT, CCND3, CFTR, CHKB, CHRNA4, CNTF, COL1A2, COL6A3, COX8A, CPOX, CRP, CYP19A1, DNAH8, DYNC1H1, EEF1A2, EMD, FABP3, NTF3, PDK4, CD274, PLA2G6, RNMT, APLN, COX5A, GTF2IRD1, MAD2L1BP, SLK, MATR3, MFN2, HNRNPDL, TRDN, MICU1, NDRG1, STK25, RBCK1, CUL9, NFASC, SMCHD1, TARDBP, MORC3, MMD, TNPO3, PRPF6, MCAT, TCAP, CNBP, PGD, VGF, PKM, PLA2G4A, PLAT, PPP1R1A, PRKAA1, PRKAA2, PRKAB1, REN, RYR2, ATXN1, SCN8A, CCL2, CCL18, SGCD, SHBG, SLC18A3, SNCA, SPRR2A, SPTBN1, TRIM21, RO60, TPM1, VEGFA, DUX4
-
Agrammatism
Wikipedia
Contents 1 History 1.1 Verb Inflection 2 See also 3 Notes 4 References History [ edit ] Agrammatism was first coined by Adolf Kussmaul in 1887 to explain the inability to form words grammatically and to syntactically order them into a sentence. ... Nowadays, the image has slightly changed: grammatical impairment has been found to be selective rather than complete, and a cross-linguistic perspective under the framework of Universal Grammar (UG) together with a shift from morphosyntax to morphosemantics is à la page. Now the focus of study in agrammatism embraces all natural languages and the idiosyncrasies scholars think a specific language has are put in relation to other languages so as to better understand agrammatism, help its treatment, and review and advance in the field of theoretical linguistics .
-
Cardiac Tamponade
Wikipedia
The fluid involved is often blood , but pus is also found in some circumstances. [10] Surgery [ edit ] One of the most common settings for cardiac tamponade is in the first 7 days after heart surgery. [14] After heart surgery, chest tubes are placed to drain blood. ... S2CID 205395461 . ^ a b c Kahan, Scott (2008). In a Page: Medicine . Lippincott Williams & Wilkins. p. 20.
-
Extracranial Germ Cell Tumor
Wikipedia
Type of tumor This article is an orphan , as no other articles link to it . Please introduce links to this page from related articles ; try the Find link tool for suggestions. ( June 2019 ) Extracranial Germ Cell Tumor A mixed germ cell tumor Specialty Oncology Symptoms Painless bump in the center of body, abnormal menstruation, bump in testes Risk factors Specific genetic syndrome, congenital abnormalities Diagnostic method Tumor marker test, immunohistochemistry , MRI , chest x-ray , CT scan , ultrasound exam, biopsy Treatment Surgery , chemotherapy , radiotherapy Medication Cisplatin based chemotherapy, BEP (cisplatin, etoposide, and bleomycin) Prognosis High survival rate after treatments Frequency 3%(<15) and 14%(≥15) An Extracranial Germ-Cell Tumor ( EGCT ) occurs in the abnormal growth of germ cells in the gonads (testes or ovaries) and the areas other than the brain via tissue , lymphatic system , or circulatory system . ... Both classifications are used by professionals to diagnose the type of tumor the patient has by the assistance of multiple results from different testaments. The first classification organized the EGCTs into two types, gonadal and extragonadal germ-cell tumor.
-
Mastocytoma
Wikipedia
. ^ FDA NEWS RELEASE ^ [1] ^ CBS News FDA Approves First-Ever Dog Cancer Drug ^ Séguin B, Besancon M, McCallan J, Dewe L, Tenwolde M, Wong E, Kent M (2006). ... Veterinary Learning Systems. 29 (4): 204. ^ Turrel J, Farrelly J, Page R, McEntee M (2006). "Evaluation of strontium 90 irradiation in treatment of cutaneous mast cell tumors in cats: 35 cases (1992–2002)".
-
Shigellosis
Wikipedia
Additionally, ampicillin (but not amoxicillin ) was effective in treating this disease previously, but now the first choice of drug is pivmecillinam . [25] Epidemiology [ edit ] Insufficient data exist, [26] but it is estimated to have caused the death of 34,000 children under the age of five in 2013, and 40,000 deaths in people over five years of age. [16] Shigella also causes about 580,000 cases annually among travelers and military personnel from industrialized countries. [27] An estimated 500,000 cases of shigellosis occur annually in the United States. [20] Infants, the elderly, and the critically ill are susceptible to the most severe symptoms of disease, but all humans are susceptible to some degree. ... External links [ edit ] CDC's Shigellosis Page Vaccine Resource Library: Shigellosis and enterotoxigenic Escherichia coli (ETEC) Classification D ICD - 10 : A03 ICD - 9-CM : 004 MeSH : D004405 External resources MedlinePlus : 000295 eMedicine : med/2112 Patient UK : Shigellosis v t e Proteobacteria -associated Gram-negative bacterial infections α Rickettsiales Rickettsiaceae / ( Rickettsioses ) Typhus Rickettsia typhi Murine typhus Rickettsia prowazekii Epidemic typhus , Brill–Zinsser disease , Flying squirrel typhus Spotted fever Tick-borne Rickettsia rickettsii Rocky Mountain spotted fever Rickettsia conorii Boutonneuse fever Rickettsia japonica Japanese spotted fever Rickettsia sibirica North Asian tick typhus Rickettsia australis Queensland tick typhus Rickettsia honei Flinders Island spotted fever Rickettsia africae African tick bite fever Rickettsia parkeri American tick bite fever Rickettsia aeschlimannii Rickettsia aeschlimannii infection Mite-borne Rickettsia akari Rickettsialpox Orientia tsutsugamushi Scrub typhus Flea-borne Rickettsia felis Flea-borne spotted fever Anaplasmataceae Ehrlichiosis : Anaplasma phagocytophilum Human granulocytic anaplasmosis , Anaplasmosis Ehrlichia chaffeensis Human monocytotropic ehrlichiosis Ehrlichia ewingii Ehrlichiosis ewingii infection Rhizobiales Brucellaceae Brucella abortus Brucellosis Bartonellaceae Bartonellosis : Bartonella henselae Cat-scratch disease Bartonella quintana Trench fever Either B. henselae or B. quintana Bacillary angiomatosis Bartonella bacilliformis Carrion's disease , Verruga peruana β Neisseriales M+ Neisseria meningitidis/meningococcus Meningococcal disease , Waterhouse–Friderichsen syndrome , Meningococcal septicaemia M− Neisseria gonorrhoeae/gonococcus Gonorrhea ungrouped: Eikenella corrodens / Kingella kingae HACEK Chromobacterium violaceum Chromobacteriosis infection Burkholderiales Burkholderia pseudomallei Melioidosis Burkholderia mallei Glanders Burkholderia cepacia complex Bordetella pertussis / Bordetella parapertussis Pertussis γ Enterobacteriales ( OX− ) Lac+ Klebsiella pneumoniae Rhinoscleroma , Pneumonia Klebsiella granulomatis Granuloma inguinale Klebsiella oxytoca Escherichia coli : Enterotoxigenic Enteroinvasive Enterohemorrhagic O157:H7 O104:H4 Hemolytic-uremic syndrome Enterobacter aerogenes / Enterobacter cloacae Slow/weak Serratia marcescens Serratia infection Citrobacter koseri / Citrobacter freundii Lac− H2S+ Salmonella enterica Typhoid fever , Paratyphoid fever , Salmonellosis H2S− Shigella dysenteriae / sonnei / flexneri / boydii Shigellosis , Bacillary dysentery Proteus mirabilis / Proteus vulgaris Yersinia pestis Plague / Bubonic plague Yersinia enterocolitica Yersiniosis Yersinia pseudotuberculosis Far East scarlet-like fever Pasteurellales Haemophilus : H. influenzae Haemophilus meningitis Brazilian purpuric fever H. ducreyi Chancroid H. parainfluenzae HACEK Pasteurella multocida Pasteurellosis Actinobacillus Actinobacillosis Aggregatibacter actinomycetemcomitans HACEK Legionellales Legionella pneumophila / Legionella longbeachae Legionnaires' disease Coxiella burnetii Q fever Thiotrichales Francisella tularensis Tularemia Vibrionaceae Vibrio cholerae Cholera Vibrio vulnificus Vibrio parahaemolyticus Vibrio alginolyticus Plesiomonas shigelloides Pseudomonadales Pseudomonas aeruginosa Pseudomonas infection Moraxella catarrhalis Acinetobacter baumannii Xanthomonadaceae Stenotrophomonas maltophilia Cardiobacteriaceae Cardiobacterium hominis HACEK Aeromonadales Aeromonas hydrophila / Aeromonas veronii Aeromonas infection ε Campylobacterales Campylobacter jejuni Campylobacteriosis , Guillain–Barré syndrome Helicobacter pylori Peptic ulcer , MALT lymphoma , Gastric cancer Helicobacter cinaedi Helicobacter cellulitis