-
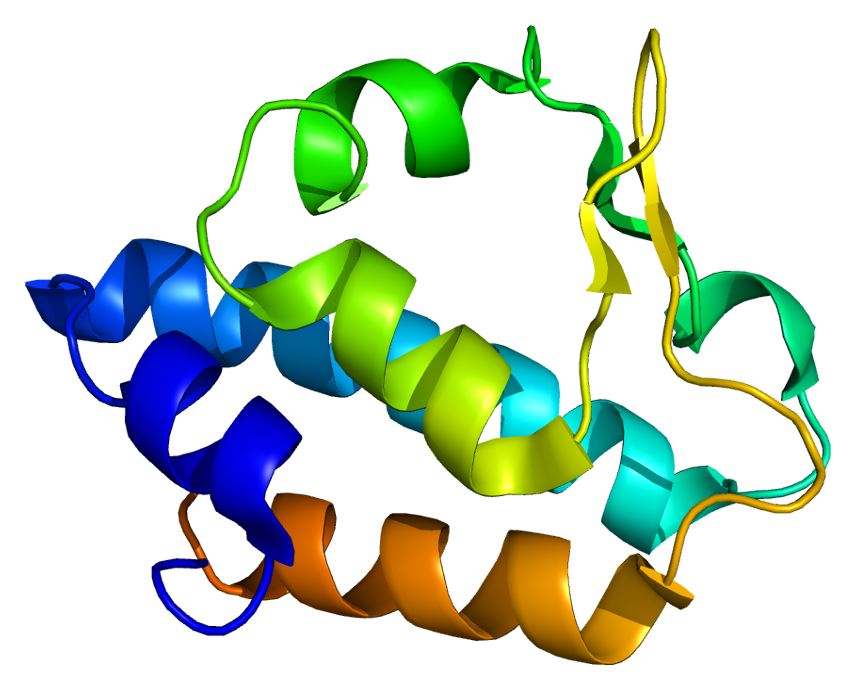
N-Acetylglutamate Synthase Deficiency
Wikipedia
External links [ edit ] GeneReviews/NCBI/NIH/UW entry on Urea Cycle Disorders Overview Classification D OMIM : 237310 MeSH : C536109 DiseasesDB : 29823 External resources eMedicine : ped/10 v t e Inborn error of amino acid metabolism K → acetyl-CoA Lysine /straight chain Glutaric acidemia type 1 type 2 Hyperlysinemia Pipecolic acidemia Saccharopinuria Leucine 3-hydroxy-3-methylglutaryl-CoA lyase deficiency 3-Methylcrotonyl-CoA carboxylase deficiency 3-Methylglutaconic aciduria 1 Isovaleric acidemia Maple syrup urine disease Tryptophan Hypertryptophanemia G G→ pyruvate → citrate Glycine D-Glyceric acidemia Glutathione synthetase deficiency Sarcosinemia Glycine → Creatine : GAMT deficiency Glycine encephalopathy G→ glutamate → α-ketoglutarate Histidine Carnosinemia Histidinemia Urocanic aciduria Proline Hyperprolinemia Prolidase deficiency Glutamate / glutamine SSADHD G→ propionyl-CoA → succinyl-CoA Valine Hypervalinemia Isobutyryl-CoA dehydrogenase deficiency Maple syrup urine disease Isoleucine 2-Methylbutyryl-CoA dehydrogenase deficiency Beta-ketothiolase deficiency Maple syrup urine disease Methionine Cystathioninuria Homocystinuria Hypermethioninemia General BC / OA Methylmalonic acidemia Methylmalonyl-CoA mutase deficiency Propionic acidemia G→ fumarate Phenylalanine / tyrosine Phenylketonuria 6-Pyruvoyltetrahydropterin synthase deficiency Tetrahydrobiopterin deficiency Tyrosinemia Alkaptonuria / Ochronosis Tyrosinemia type I Tyrosinemia type II Tyrosinemia type III / Hawkinsinuria Tyrosine → Melanin Albinism : Ocular albinism ( 1 ) Oculocutaneous albinism ( Hermansky–Pudlak syndrome ) Waardenburg syndrome Tyrosine → Norepinephrine Dopamine beta hydroxylase deficiency reverse: Brunner syndrome G→ oxaloacetate Urea cycle / Hyperammonemia ( arginine aspartate ) Argininemia Argininosuccinic aciduria Carbamoyl phosphate synthetase I deficiency Citrullinemia N-Acetylglutamate synthase deficiency Ornithine transcarbamylase deficiency / translocase deficiency Transport / IE of RTT Solute carrier family : Cystinuria Hartnup disease Iminoglycinuria Lysinuric protein intolerance Fanconi syndrome : Oculocerebrorenal syndrome Cystinosis Other 2-Hydroxyglutaric aciduria Aminoacylase 1 deficiency Ethylmalonic encephalopathy Fumarase deficiency Trimethylaminuria
- Toxic Multinodular Goitre Wikipedia
-
Gaffkaemia
Wikipedia
ISBN 978-0-8138-1844-3 . ^ a b c d e f g h i j k l Jeffrey D. Shields; Fran J. Stephens; Brian Jones (2006).
-
Red Thread Disease
Wikipedia
References [ edit ] ^ Buczacki, S. and Harris, K., Pests, Diseases and Disorders of Garden Plants , HarperCollins, 1998, p484 External links [ edit ] http://www.lawnandmower.com/red-thread-disease.aspx http://www.grassclippings.co.uk/RedThread.pdf
- Aortoiliac Occlusive Disease Wikipedia
- Kufs Disease Wikipedia
- Sertoli Cell Tumour Wikipedia
- Osteochondrosis Wikipedia
-
Pusher Syndrome
Wikipedia
Steps to follow: A guide to the treatment of adult hemiplegia : Based on the concept of K. and B. Bobath . New York: Springer-Verlag. ^ O'Sullivan, S. (2007).
- Wiedemann–rautenstrauch Syndrome Wikipedia
- Ngly1 Deficiency Wikipedia
-
Mystical Psychosis
Wikipedia
Deikman considered that all-encompassing unity opened in mysticism can be all-encompassing unity of reality. [15] See also [ edit ] Altered state of consciousness Depersonalization and Derealization Existential crisis Dhyāna in Buddhism Dhyāna in Hinduism Jerusalem syndrome Mental health Moksha Mirror neurons Mysticism Monomyth Near-death experience Posttraumatic stress disorder Religious experience Spiritualism Spirituality Spiritual crisis Wujud References [ edit ] ^ Whitney, E. (1998). " Personal accounts: Mania as spiritual emergency " Psychiatric Services 49 : 1547–1548 ^ Jackson, M., & Fulford, K.W.M., K. W. M.; Jackson, Mike (1997). "Spiritual experience and psychopathology".
-
Salla Disease
Wikipedia
PMID 420628 . [ permanent dead link ] ^ Autio-Harmainen H, Oldfors A, Sourander P, Renlund M, Dammert K, Simila S (1988). "Neuropathology of Salla disease".SLC17A5, GNE, CEACAM5, MATN1, VEGFA, RENBP, CD274, HPGDS, SGCB, TAF2, TGFB1, ZFPM2-AS1, TNF, EFL1, PCGF2, ZBTB16, PER2, ADIPOQ, KDM5A, DLL3, BACE1, RETN, LAMP3, APP, PIK3CD, PIK3CG, ATP7A, CALB2, CASP3, CD28, CDKN2B, CHIT1, DBH, DCC, DCX, EPO, ERBB2, GH1, HSP90AA1, IFNG, IDO1, LEP, LSAMP, NPY, PIK3CA, PIK3CB, LOC108281177
- Gourmand Syndrome Wikipedia
-
Duodenal Lymphocytosis
Wikipedia
. ^ a b c d Hammer, Suntrea T. G.; Greenson, Joel K. (2013). "The Clinical Significance of Duodenal Lymphocytosis With Normal Villus Architecture".
- Perineal Hernia Wikipedia
-
Pacific Coast Tick Fever
Wikipedia
., Robinson, L.K., White, F.H., Slater, K., Karpathy, S.E., Eremeeva, M.E. and Dasch, G.A.
-
Nodular Fasciitis
Wikipedia
Because recurrence is rare, even when there is incomplete excision, in case of recurrence initial diagnosis of nodular fasciitis should be revisited. [5] See also [ edit ] Leiomyosarcoma List of cutaneous conditions Inflammatory myofibroblastic tumour References [ edit ] ^ a b c Freedberg IM, Eisen AZ, Wolff K, Austen KF, Goldsmith LA, Katz SI, eds. (2003).
- Aschoff Body Wikipedia
- Damping Off Wikipedia