Load FindZebra Summary
Disclaimer:
FindZebra Search conducts a search using our specialized medical search engine.
FindZebra Summary uses the text completions API
(subject to OpenAI’s API data usage policies)
to summarize and reason about the search results.
The search is conducted in publicly available information on the Internet that we present “as is”.
You should be aware that FindZebra is not supplying any of the content in the search results.
FindZebra Summary is loading...
-
Cowden Syndrome
MedlinePlus
Causes Changes involving at least four genes, PTEN , SDHB , SDHD , and KLLN , have been identified in people with Cowden syndrome or Cowden-like syndrome. Most cases of Cowden syndrome and a small percentage of cases of Cowden-like syndrome result from mutations in the PTEN gene. ... Other cases of Cowden syndrome and Cowden-like syndrome result from changes involving the KLLN gene. ... A small percentage of people with Cowden syndrome or Cowden-like syndrome have variations in the SDHB or SDHD gene. ... However, researchers are uncertain whether the identified SDHB and SDHD gene variants are directly associated with Cowden syndrome and Cowden-like syndrome.
-
Cowden Syndrome
Wikipedia
Cowden syndrome Other names Cowden's disease, multiple hamartoma syndrome Cumulative risk for the development of cancer in males and females with Cowden syndrome from birth to age 70. ... "Cowden syndrome: recognizing and managing a not-so-rare hereditary cancer syndrome". ... PMID 17920899 . ^ Pilarski R (February 2009). "Cowden syndrome: a critical review of the clinical literature". ... Eng C (November 2000). "Will the real Cowden syndrome please stand up: revised diagnostic criteria" . ... Pilarski R, Eng C (May 2004). "Will the real Cowden syndrome please stand up (again)?PTEN, SDHB, PIK3CA, KLLN, AKT1, SDHD, SEC23B, SDHC, FGFR2, EGFR, TNF, NOD2, TEP1, IL10, BMPR1A, TP53, IL23R, OSR1, BRCA1, MTOR, ATG16L1, SDS, CEACAM6, SARDH, CRP, HLA-DQA1, TGM2, IFNG, SMAD4, KLK3, IL17A, BRCA2, ACAD8, SORD, IL6, PLAG1, PIK3CG, NPEPPS, TGFBI, TESC, PIK3CD, PIK3CB, IL1B, PSAT1, NR3C1, GTF2H1, GTF2H2, GTF2H3, GTF2H4, HIF1A, IBD5, TGFB1, MAPK1, HSP90B1, ADA, TLR2, TLR4, STK11, BDNF, SST, MIR21, SLC12A3, GTF2H5, IL15, TPMT, TSC1, LTA, LCN2, TNFSF15, VWF, IL15RA, PROS1, ERCC2, ERCC3, HEPH, DGCR2, DNAJC6, GDF15, GRAP2, CLOCK, TP63, ARHGEF2, HMGA2, TIMP1, TNFRSF1A, TNNI3, TSC2, UBC, VEGFA, VIM, AIMP2, GPR68, SLC16A3, BFSP2, RASAL1, RABEPK, NR1I2, SQSTM1, SGCE, USP8, SLC16A4, ABCB6, ACAT1, LANCL1, SEMA4D, LYPD1, TAGAP, SLCO6A1, SIRPA, SPRED1, TMPRSS6, USF3, IL27, TCERG1L, ARMH1, GSTK1, ASPG, MIR19A, MIR206, MIR29B1, MIR29B2, DEFA1A3, POU5F1P3, POU5F1P4, DEFB4B, MIR1290, LINC01672, OCLN, RN7SL263P, LOC110806263, IL17F, LMLN, KAT8, IL23A, AHSA1, TXNIP, CCR9, EBNA1BP2, KIF3A, FSTL1, TBC1D9, RNF19A, PTPN22, HAVCR1, IL19, MPC1, TMPRSS13, IL17D, SLC38A2, IL26, MYDGF, SUCNR1, SLURP1, HAMP, GORASP1, P2RY12, WNK1, CYREN, POLDIP2, SCD, TG, PTK2B, ACE, DEFB4A, DMBT1, DSC2, DSG2, TOR1A, EGF, ERCC5, ERCC6, EYA1, EYA2, FAP, CYBB, FGF2, FKBP5, FN1, GABPA, GAPDH, GCH1, GH1, GHSR, GLS, FFAR2, GPX1, CYP11A1, CCN2, TFF3, CASP3, ALB, ALDH1A1, APC, AR, ARSD, ATF3, BAX, BCL2, BGLAP, DDR1, CAMP, CAT, CSH2, CAV1, SERPINH1, CCNH, CD86, CD40, CDH2, CDK7, ERCC8, CRK, MAPK14, CSH1, HFE, HLA-DPB1, HLA-DQA2, CCL2, PMS2, POMC, POU5F1, PPIA, MAPK8, PROX1, PSMD7, RAP1A, RELA, RET, ACHE, CCL11, HLA-DQB1, CCL20, SDC1, SLC2A1, SLC6A4, SLC11A1, STAT3, STAT5A, STAT5B, SYT1, ADAM17, TRBV20OR9-2, ABCB1, PGF, TNFRSF11B, NFE2L2, HLA-DRB4, HSPA9, IFNA1, IFNA13, IL4, IL9, JAK2, KCNN4, RPSA, LBR, EPCAM, SMAD2, SMAD7, MAOA, MAT1A, MBL2, MAP3K5, MMP9, MSMB, MST1, MUC4, MUTYH, MYCN, H3P28
-
Cowden Syndrome 1
OMIM
Busch et al. (2013) studied 23 individuals with PTEN mutations and 2 with PTEN-negative Cowden syndrome or Bannayan-Riley-Ruvalcaba syndrome, respectively. ... Cowden Syndrome With Immunodeficiency Browning et al. (2015) reported 2 unrelated boys with genetically confirmed Cowden syndrome associated with primary immunodeficiency resulting in recurrent infections. ... Marsh et al. (1998) carried out mutation analysis in the PTEN gene in 64 unrelated Cowden syndrome-like families. These families were defined as having some features of Cowden syndrome but did not meet the diagnostic criteria of the International Cowden Consortium. ... The former mutation had been reported in patients with Cowden syndrome, whereas the latter mutation had been reported in patients with Bannayan-Zonana syndrome. ... For discussion of a possible association of Cowden syndrome with variation in the USF3 gene, see 617568.
-
Multiple Hamartoma Syndrome
Wikipedia
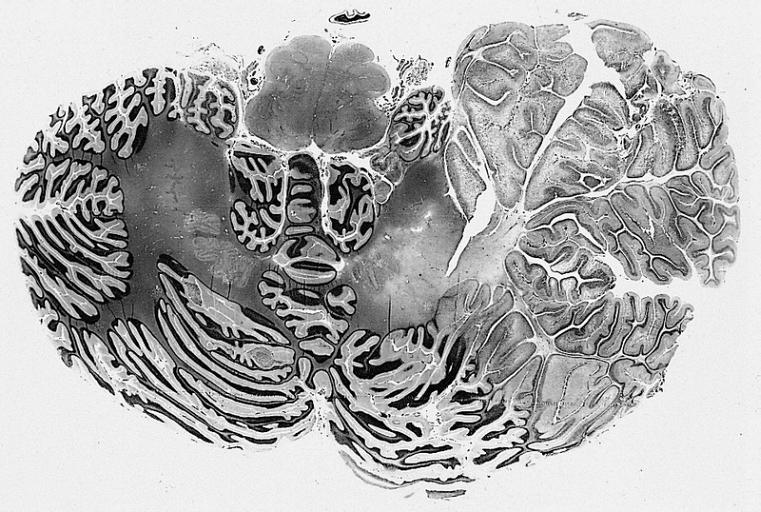
Multiple hamartoma syndrome Specialty Oncology , medical genetics Multiple hamartoma syndrome is a syndrome characterized by more than one hamartoma . [1] : 673 It is sometimes equated with Cowden syndrome . However, MeSH also includes Bannayan–Zonana syndrome (that is, Bannayan–Riley–Ruvalcaba syndrome ) and Lhermitte–Duclos disease under this description. Some articles include Cowden syndrome, Bannayan–Riley–Ruvalcaba syndrome, and at least some forms of Proteus syndrome and Proteus-like syndrome under the umbrella term PTEN hamartoma tumor syndromes ( PHTS ). ... External links [ edit ] Classification D OMIM : 158350 MeSH : D006223 DiseasesDB : 31336 v t e Phakomatosis Angiomatosis Sturge–Weber syndrome Von Hippel–Lindau disease Hamartoma Tuberous sclerosis Hypothalamic hamartoma ( Pallister–Hall syndrome ) Multiple hamartoma syndrome Proteus syndrome Cowden syndrome Bannayan–Riley–Ruvalcaba syndrome Lhermitte–Duclos disease Neurofibromatosis Type I Type II Other Abdallat–Davis–Farrage syndrome Ataxia telangiectasia Incontinentia pigmenti Peutz–Jeghers syndrome Encephalocraniocutaneous lipomatosis This Epidermal nevi, neoplasms, cysts article is a stub .
-
Bannayan–riley–ruvalcaba Syndrome
Wikipedia
The disease is inherited in an autosomal dominant manner. [4] The disease belongs to a family of hamartomatous polyposis syndromes, which also includes Peutz–Jeghers syndrome , juvenile polyposis and Cowden syndrome . Mutation of the PTEN gene underlies this syndrome, as well as Cowden syndrome , Proteus syndrome , and Proteus-like syndrome , these four syndromes are referred to as PTEN Hamartoma-Tumor Syndromes. [5] Contents 1 Signs and symptoms 2 Genetics 3 Diagnosis 3.1 Differential diagnosis 4 Treatment 5 See also 6 References 7 Further reading 8 External links Signs and symptoms [ edit ] Bannayan–Riley–Ruvalcaba syndrome is associated with enlarged head and benign mesodermal hamartomas (multiple hemangiomas , and intestinal polyps ). ... PTEN chromosomal location is 10q23.31, while the molecular location is 87,863,438 to 87,971,930 [2] [7] There are many syndromes that are linked to PTEN aside from Bannayan–Riley–Ruvalcaba Syndrome. [8] The syndrome combines Bannayan–Zonana syndrome, Riley–Smith syndrome, and Ruvalcaba–Myhre–Smith syndrome. [9] Bannayan–Zonana syndrome is named for George A. Bannayan and Jonathan Zonana [10] Diagnosis [ edit ] In terms of diagnosing Bannayan–Riley–Ruvalcaba syndrome there is no current method outside the physical characteristics that may be present as signs/symptoms. [3] There are, however, multiple molecular genetics tests (and cytogenetic test) to determine Bannayan–Riley–Ruvalcaba syndrome. [11] Differential diagnosis [ edit ] The differential diagnosis for BRRS consists of the following: [12] Juvenile polyposis syndrome Peutz–Jeghers syndrome Proteus syndrome Neurofibromatosis 1 Cowden syndrome Treatment [ edit ] Kidney In terms of treatment/management one should observe what signs or symptoms are present and therefore treat those as there is no other current guideline. ... CS1 maint: extra text: authors list ( link ) External links [ edit ] Classification D ICD - 10 : Q87.8 OMIM : 153480 MeSH : D006223 DiseasesDB : 31337 Scholia has a topic profile for Bannayan–Riley–Ruvalcaba syndrome . v t e Congenital abnormality syndromes Craniofacial Acrocephalosyndactylia Apert syndrome Carpenter syndrome Pfeiffer syndrome Saethre–Chotzen syndrome Sakati–Nyhan–Tisdale syndrome Bonnet–Dechaume–Blanc syndrome Other Baller–Gerold syndrome Cyclopia Goldenhar syndrome Möbius syndrome Short stature 1q21.1 deletion syndrome Aarskog–Scott syndrome Cockayne syndrome Cornelia de Lange syndrome Dubowitz syndrome Noonan syndrome Robinow syndrome Silver–Russell syndrome Seckel syndrome Smith–Lemli–Opitz syndrome Snyder–Robinson syndrome Turner syndrome Limbs Adducted thumb syndrome Holt–Oram syndrome Klippel–Trénaunay–Weber syndrome Nail–patella syndrome Rubinstein–Taybi syndrome Gastrulation / mesoderm : Caudal regression syndrome Ectromelia Sirenomelia VACTERL association Overgrowth syndromes Beckwith–Wiedemann syndrome Proteus syndrome Perlman syndrome Sotos syndrome Weaver syndrome Klippel–Trénaunay–Weber syndrome Benign symmetric lipomatosis Bannayan–Riley–Ruvalcaba syndrome Neurofibromatosis type I Laurence–Moon–Bardet–Biedl Bardet–Biedl syndrome Laurence–Moon syndrome Combined/other, known locus 2 ( Feingold syndrome ) 3 ( Zimmermann–Laband syndrome ) 4 / 13 ( Fraser syndrome ) 8 ( Branchio-oto-renal syndrome , CHARGE syndrome ) 12 ( Keutel syndrome , Timothy syndrome ) 15 ( Marfan syndrome ) 19 ( Donohue syndrome ) Multiple Fryns syndrome v t e Phakomatosis Angiomatosis Sturge–Weber syndrome Von Hippel–Lindau disease Hamartoma Tuberous sclerosis Hypothalamic hamartoma ( Pallister–Hall syndrome ) Multiple hamartoma syndrome Proteus syndrome Cowden syndrome Bannayan–Riley–Ruvalcaba syndrome Lhermitte–Duclos disease Neurofibromatosis Type I Type II Other Abdallat–Davis–Farrage syndrome Ataxia telangiectasia Incontinentia pigmenti Peutz–Jeghers syndrome Encephalocraniocutaneous lipomatosis v t e Deficiencies of intracellular signaling peptides and proteins GTP-binding protein regulators GTPase-activating protein Neurofibromatosis type I Watson syndrome Tuberous sclerosis Guanine nucleotide exchange factor Marinesco–Sjögren syndrome Aarskog–Scott syndrome Juvenile primary lateral sclerosis X-Linked mental retardation 1 G protein Heterotrimeic cAMP / GNAS1 : Pseudopseudohypoparathyroidism Progressive osseous heteroplasia Pseudohypoparathyroidism Albright's hereditary osteodystrophy McCune–Albright syndrome CGL 2 Monomeric RAS: HRAS Costello syndrome KRAS Noonan syndrome 3 KRAS Cardiofaciocutaneous syndrome RAB: RAB7 Charcot–Marie–Tooth disease RAB23 Carpenter syndrome RAB27 Griscelli syndrome type 2 RHO: RAC2 Neutrophil immunodeficiency syndrome ARF : SAR1B Chylomicron retention disease ARL13B Joubert syndrome 8 ARL6 Bardet–Biedl syndrome 3 MAP kinase Cardiofaciocutaneous syndrome Other kinase / phosphatase Tyrosine kinase BTK X-linked agammaglobulinemia ZAP70 ZAP70 deficiency Serine/threonine kinase RPS6KA3 Coffin-Lowry syndrome CHEK2 Li-Fraumeni syndrome 2 IKBKG Incontinentia pigmenti STK11 Peutz–Jeghers syndrome DMPK Myotonic dystrophy 1 ATR Seckel syndrome 1 GRK1 Oguchi disease 2 WNK4 / WNK1 Pseudohypoaldosteronism 2 Tyrosine phosphatase PTEN Bannayan–Riley–Ruvalcaba syndrome Lhermitte–Duclos disease Cowden syndrome Proteus-like syndrome MTM1 X-linked myotubular myopathy PTPN11 Noonan syndrome 1 LEOPARD syndrome Metachondromatosis Signal transducing adaptor proteins EDARADD EDARADD Hypohidrotic ectodermal dysplasia SH3BP2 Cherubism LDB3 Zaspopathy Other NF2 Neurofibromatosis type II NOTCH3 CADASIL PRKAR1A Carney complex PRKAG2 Wolff–Parkinson–White syndrome PRKCSH PRKCSH Polycystic liver disease XIAP XIAP2 See also intracellular signaling peptides and proteins
-
Trichilemmoma
Wikipedia
Multifocal occurrence is associated with Cowden syndrome , in which hamartomatous intestinal polyposis is seen in conjunction with multiple tricholemmoma lesions. Contents 1 Additional images 2 See also 3 References 4 External links Additional images [ edit ] A trichilemmoma on a forehead See also [ edit ] Cowden syndrome Trichilemmal carcinoma List of cutaneous conditions List of cutaneous neoplasms associated with systemic syndromes References [ edit ] ^ Busam Klaus J., Dermatopathology s.386; 2010 Saunders ISBN 978-0-443-06654-2 ^ James, William D.; Berger, Timothy G.; et al. (2006). ... External links [ edit ] Classification D ICD - 10 : D23 ( ILDS D23.L12) v t e Cancers of skin and associated structures Glands Sweat gland Eccrine Papillary eccrine adenoma Eccrine carcinoma Eccrine nevus Syringofibroadenoma Spiradenoma Apocrine Cylindroma Dermal cylindroma Syringocystadenoma papilliferum Papillary hidradenoma Hidrocystoma Apocrine gland carcinoma Apocrine nevus Eccrine / apocrine Syringoma Hidradenoma or Acrospiroma / Hidradenocarcinoma Ceruminous adenoma Sebaceous gland Nevus sebaceous Muir–Torre syndrome Sebaceous carcinoma Sebaceous adenoma Sebaceoma Sebaceous nevus syndrome Sebaceous hyperplasia Mantleoma Hair Pilomatricoma / Malignant pilomatricoma Trichoepithelioma Multiple familial trichoepithelioma Solitary trichoepithelioma Desmoplastic trichoepithelioma Generalized trichoepithelioma Trichodiscoma Trichoblastoma Fibrofolliculoma Trichilemmoma Trichilemmal carcinoma Proliferating trichilemmal cyst Giant solitary trichoepithelioma Trichoadenoma Trichofolliculoma Dilated pore Isthmicoma Fibrofolliculoma Perifollicular fibroma Birt–Hogg–Dubé syndrome Hamartoma Basaloid follicular hamartoma Folliculosebaceous cystic hamartoma Folliculosebaceous-apocrine hamartoma Nails Neoplasms of the nailbed This Epidermal nevi, neoplasms, cysts article is a stub .
-
Juvenile Polyposis Of Infancy
Orphanet
Early death has been reported and the risk of cancer in surviving children has not yet been clearly established. Signs of the Cowden or Bannayan-Riley-Ruvalcaba (BRRS) syndromes (see these terms) such as macrocephaly, lipomas, and hemangioblastomas can be observed. ... Differential diagnosis The differential diagnosis should include the allelic disorders Cowden syndrome and Bannayan-Riley-Ruvalcaba syndrome, which are caused by mutations in the PTEN gene, as well as familial adenomatous polyposis and Peutz-Jeghers syndrome (see these terms).
-
Glycogenic Acanthosis
Wikipedia
Extensive glycogenic acanthosis has been shown to be associated with Cowden's syndrome . [5] Diagnosis [ edit ] Glycogenic acanthosis is characterized by epithelial hyperplasia, with an increased number of enlarged epithelial cells containing abundant glycogen. ... Diffuse esophageal glycogenic acanthosis: an endoscopic marker of Cowden's disease. Am J Gastroenterol . 1997 Jun;92(6):1038-40 PMID 9177527 External links [ edit ] Microscopic images
-
Watson Syndrome
Wikipedia
Watson syndrome Specialty Medical genetics Watson syndrome is an autosomal dominant condition characterized by Lisch nodules of the ocular iris , axillary/inguinal freckling, pulmonary valvular stenosis , relative macrocephaly , short stature , and neurofibromas . [1] Watson syndrome is allelic to NF1 , the same gene associated with neurofibromatosis type 1 . [2] See also [ edit ] Westerhof syndrome List of cutaneous conditions References [ edit ] ^ Rapini, Ronald P.; Bolognia, Jean L.; Jorizzo, Joseph L. (2007). ... ISBN 978-1-4160-2999-1 . ^ Allanson JE, Upadhyaya M, Watson GH, et al. (November 1991). "Watson syndrome: is it a subtype of type 1 neurofibromatosis?" ... External links [ edit ] Classification D ICD - 10 : Q87.1 OMIM : 193520 MeSH : D009456 DiseasesDB : 32244 External resources Orphanet : 3444 v t e Phakomatosis Angiomatosis Sturge–Weber syndrome Von Hippel–Lindau disease Hamartoma Tuberous sclerosis Hypothalamic hamartoma ( Pallister–Hall syndrome ) Multiple hamartoma syndrome Proteus syndrome Cowden syndrome Bannayan–Riley–Ruvalcaba syndrome Lhermitte–Duclos disease Neurofibromatosis Type I Type II Other Abdallat–Davis–Farrage syndrome Ataxia telangiectasia Incontinentia pigmenti Peutz–Jeghers syndrome Encephalocraniocutaneous lipomatosis v t e Deficiencies of intracellular signaling peptides and proteins GTP-binding protein regulators GTPase-activating protein Neurofibromatosis type I Watson syndrome Tuberous sclerosis Guanine nucleotide exchange factor Marinesco–Sjögren syndrome Aarskog–Scott syndrome Juvenile primary lateral sclerosis X-Linked mental retardation 1 G protein Heterotrimeic cAMP / GNAS1 : Pseudopseudohypoparathyroidism Progressive osseous heteroplasia Pseudohypoparathyroidism Albright's hereditary osteodystrophy McCune–Albright syndrome CGL 2 Monomeric RAS: HRAS Costello syndrome KRAS Noonan syndrome 3 KRAS Cardiofaciocutaneous syndrome RAB: RAB7 Charcot–Marie–Tooth disease RAB23 Carpenter syndrome RAB27 Griscelli syndrome type 2 RHO: RAC2 Neutrophil immunodeficiency syndrome ARF : SAR1B Chylomicron retention disease ARL13B Joubert syndrome 8 ARL6 Bardet–Biedl syndrome 3 MAP kinase Cardiofaciocutaneous syndrome Other kinase / phosphatase Tyrosine kinase BTK X-linked agammaglobulinemia ZAP70 ZAP70 deficiency Serine/threonine kinase RPS6KA3 Coffin-Lowry syndrome CHEK2 Li-Fraumeni syndrome 2 IKBKG Incontinentia pigmenti STK11 Peutz–Jeghers syndrome DMPK Myotonic dystrophy 1 ATR Seckel syndrome 1 GRK1 Oguchi disease 2 WNK4 / WNK1 Pseudohypoaldosteronism 2 Tyrosine phosphatase PTEN Bannayan–Riley–Ruvalcaba syndrome Lhermitte–Duclos disease Cowden syndrome Proteus-like syndrome MTM1 X-linked myotubular myopathy PTPN11 Noonan syndrome 1 LEOPARD syndrome Metachondromatosis Signal transducing adaptor proteins EDARADD EDARADD Hypohidrotic ectodermal dysplasia SH3BP2 Cherubism LDB3 Zaspopathy Other NF2 Neurofibromatosis type II NOTCH3 CADASIL PRKAR1A Carney complex PRKAG2 Wolff–Parkinson–White syndrome PRKCSH PRKCSH Polycystic liver disease XIAP XIAP2 See also intracellular signaling peptides and proteins This Genodermatoses article is a stub .
-
Non-Distal Monosomy 10q
Orphanet
Non-distal monosomy 10q is a rare chromosomal anomaly syndrome, resulting from a partial deletion of the long arm of chromosome 10, with a highly variable phenotype principally characterized by developmental delays (usually of language and speech), variable cognitive impairment and neurobehavioral abnormalities such as autism spectrum disorders and attention deficit disorder. Macrocephaly and mild dysmorphic features may by associated. Overlap with other syndromes, such as Cowden syndrome, Bannayan-Riley-Ruvalcaba syndrome and juvenile polyposis syndrome has been reported.
-
Juvenile Polyposis Syndrome
OMIM
It had been suggested that juvenile polyposis can be caused by mutations in the PTEN gene (601728), the same gene that is mutant in Cowden syndrome-1 (158350). In a comprehensive review of PTEN, Waite and Eng (2002) concluded that juvenile intestinal polyposis is not a so-called PTEN hamartoma-tumor syndrome (PHTS). ... Eng and Peacocke (1998) and Eng and Ji (1998) suggested further that the 3 patients found by Olschwang et al. (1998) to have germline PTEN mutations had either Cowden disease or Bannayan-Zonana syndrome; a 74-year-old man had manifestations they interpreted as suggestive of Cowden disease, and the 2 children may not have yet demonstrated features of Cowden disease, which has a penetrance well below 10% under 15 years of age (Nelen et al., 1996). In a long review of the PTEN gene, Waite and Eng (2002) reviewed the evidence that juvenile polyposis syndrome is not one of the so-called PTEN hamartoma-tumor syndromes (PHTS). Lynch et al. (1997) referred to germline mutations in individuals with JPS, but it was obvious to Waite and Eng (2002), from the text, that all of the individuals had Cowden syndrome. Kurose et al. (1999) provided a single hospital-based series that looked for germline PTEN mutations in JPS. They identified 1 individual with a germline PTEN mutation, but on reexamination, classic cutaneous features of Cowden syndrome were found. PTEN was formally excluded as a JPS-susceptibility gene by Marsh et al. (1997) and it is known that germline mutations in MADH4 (600993) on 18q and BMPR1A (601299) on 10q account for 40 to 60% of JPS.BMPR1A, SMAD4, ENG, PTEN, CRP, ACVRL1, STK11, PTGS2, IL1B, TLR2, SLPI, MBL2, IL6, MUTYH, ELAVL1, TLR4, BMPR2, SAG, BMP2, BCS1L, TGFA, APC, TNF, HPT, TP53, SMUG1, GREM1, MBL3P, CRELD2, CDC73, CASP1, PTCH1, PMS2, PIK3CG, PIK3CD, PIK3CB, PIK3CA, MYH11, ADA, MUC5AC, CDKN1B, SMAD5, CDX2, PDX1, CTNNB1, DCC, HTC2, HHT3
-
Segmental Outgrowth-Lipomatosis-Arteriovenous Malformation-Epidermal Nevus Syndrome
Orphanet
Segmental outgrowth-lipomatosis-arteriovenous malformation-epidermal nevus syndrome is a rare, genetic, polymalformative syndrome characterized by progressive, proportionate, asymmetric segmental overgrowth (with soft tissue hypertrophy and ballooning effect) that develops and progresses rapidly in early childhood, arteriovenous and lymphatic vascular malformations, lipomatosis and linear epidermal nevus (arranged in whorls along the lines of Blaschko). Clinical symptoms of Cowden syndrome, such as macrocephaly and progressive development of numerous hypertrophic hamartomatous and neoplastic lesions involving multiple organs and systems, are also associated.
-
Hamartoma
Wikipedia
Hamartomas are usually caused by a genetic syndrome that affects the development cycle of all or at least multiple cells. [3] Many of these conditions are classified as overgrowth syndromes or cancer syndromes . ... About 50% of such cases manifest abdominal pain, and they are often associated with hematologic abnormalities and spontaneous rupture. Cowden syndrome [ edit ] This section does not cite any sources . ... Unsourced material may be challenged and removed . ( March 2017 ) ( Learn how and when to remove this template message ) Cowden syndrome is a serious genetic disorder [13] characterized by multiple hamartomas. ... The hamartomas themselves may cause symptoms or even death, but morbidity is more often associated with increased occurrence of malignancies, usually in the breast or thyroid. Cowden syndrome is considered a PTEN hamartoma tumor syndrome (PHTS), which also includes Bannayan–Riley–Ruvalcaba syndrome , Proteus syndrome and Proteus-like syndrome . ... "Topic 316: Lung Hamartoma" . eMedicine.com Radio . 2018-12-17. v t e Phakomatosis Angiomatosis Sturge–Weber syndrome Von Hippel–Lindau disease Hamartoma Tuberous sclerosis Hypothalamic hamartoma ( Pallister–Hall syndrome ) Multiple hamartoma syndrome Proteus syndrome Cowden syndrome Bannayan–Riley–Ruvalcaba syndrome Lhermitte–Duclos disease Neurofibromatosis Type I Type II Other Abdallat–Davis–Farrage syndrome Ataxia telangiectasia Incontinentia pigmenti Peutz–Jeghers syndrome Encephalocraniocutaneous lipomatosis v t e Overview of tumors , cancer and oncology Conditions Benign tumors Hyperplasia Cyst Pseudocyst Hamartoma Malignant progression Dysplasia Carcinoma in situ Cancer Metastasis Primary tumor Sentinel lymph node Topography Head and neck ( oral , nasopharyngeal ) Digestive system Respiratory system Bone Skin Blood Urogenital Nervous system Endocrine system Histology Carcinoma Sarcoma Blastoma Papilloma Adenoma Other Precancerous condition Paraneoplastic syndrome Staging / grading TNM Ann Arbor Prostate cancer staging Gleason grading system Dukes classification Carcinogenesis Cancer cell Carcinogen Tumor suppressor genes / oncogenes Clonally transmissible cancer Oncovirus Carcinogenic bacteria Misc.CYP1A1, FLCN, PTEN, TSC2, SMO, STK11, NEK9, ACTB, DYNC2LI1, TFAP2A, NTRK2, CDC73, HMGA2, ACVR1, KLLN, TSC1, TCTN3, MTOR, SMAD4, SLC12A3, TESC, LPP, PIK3CA, TP53, PIK3CD, GLI3, CDX2, PTGS2, PIK3CG, PIK3CB, RAD51B, COX2, TEP1, CD34, MTCO2P12, PGRMC1, DCTN6, DICER1, ZNRD2, DKK1, LHFPL6, ABCA4, OSTM1, SMUG1, GREM1, TMED7, WDPCP, SUFU, KRT20, FBLIM1, FBXW7, SLC12A9, GOPC, AKT1S1, TICAM2, MIR21, TMED7-TICAM2, LGR5, SHH, MOGS, VIM, BRAF, CD6, CDKN1A, CDKN2A, CLCN7, CMM, EGFR, EREG, ESR2, GNAS, GRM1, GSTM1, GSTM2, GSTT1, HMGA1, SLC29A2, IFI27, IGF2, LAMA4, MDM2, NGFR, PRRX1, PSMD9, RET, RPE, SDHB, SMARCB1, TIMP1, VEGFA, H3P23
-
Attenuated Familial Adenomatous Polyposis
Wikipedia
Attenuated familial adenomatous polyposis Other names Attenuated familial polyposis coli Specialty Oncology Attenuated familial adenomatous polyposis is a form of familial adenomatous polyposis , a cancer syndrome . It is a pre-malignant disease that can develop into colorectal cancer . ... Cancer might develop as early as the age of five, though typically presents later than classical FAP. [1] See also [ edit ] Familial adenomatous polyposis Birt–Hogg–Dubé syndrome Cowden syndrome Cronkhite–Canada syndrome Juvenile polyposis MUTYH Peutz–Jeghers syndrome References [ edit ] ^ Herold, Gerd (2012).
-
Macrocephaly/autism Syndrome
OMIM
A number sign (#) is used with this entry because of evidence that macrocephaly/autism syndrome is caused by heterozygous mutation in the PTEN gene (601728) on chromosome 10q23. Heterozygous mutation in the PTEN gene can also cause Cowden syndrome (CWS1; 158350), which shows some overlapping features. ... Naqvi et al. (2000) suggested that this may represent a recognizable syndrome within the autism behavioral phenotype. ... There were no features suggestive of Cowden syndrome (158350) except for pigmented macules on the glans penis of 1 boy. ... An unrelated 4-year-old boy with macrocephaly/autism syndrome was found to have an R130X mutation (601728.0007), which had also been found in patients with Cowden syndrome and BRRS.
-
Papillary Thyroid Microcarcinoma
OMIM
Two patterns of presentation had been described for familial differentiated thyroid cancer: a pattern associated with an inherited tumor syndrome such as Gardner syndrome (APC; 175100) and Cowden disease (158350), and a second pattern of familial aggregation without other associated neoplasms.BRAF, RET, CCDC6, F9, PTCH1, TAS2R38, LOC110806263, NRAS, TG, HT, TSHR, VIM, PAX8, PPP1R13L, FOXP3, ZNF654, SHC3, ANKRD36B, ERAP2, MEDAG, MIR21, MIR221, MIR222, MIR324, MIR146B, VEGFA, ALK, TPO, CD82, CAV1, CD59, CDKN1B, CRYZ, NQO1, GDF1, HIF1A, LAMC2, TP53, LGALS3, NQO2, SERPINF1, PPARG, RNH1, S100A4, CCND1, SLC5A5
-
Encephalocraniocutaneous Lipomatosis
Wikipedia
Encephalocraniocutaneous lipomatosis Other names Haberland syndrome , [1] Specialty Neurology Encephalocraniocutaneous lipomatosis ( ECCL ), is a rare condition primarily affecting the brain , eyes , and skin of the head and face. [2] It is characterized by unilateral subcutaneous and intracranial lipomas , alopecia , unilateral porencephalic cysts , epibulbar choristoma and other ophthalmic abnormalities. ... "Encephalocraniocutaneous lipomatosis (haberland's syndrome): a case report of a neurocutaneous syndrome and a review of the literature" . ... External links [ edit ] Classification D ICD - 10 : E88.2 OMIM : 613001 MeSH : C535736 External resources Orphanet : 2396 v t e Phakomatosis Angiomatosis Sturge–Weber syndrome Von Hippel–Lindau disease Hamartoma Tuberous sclerosis Hypothalamic hamartoma ( Pallister–Hall syndrome ) Multiple hamartoma syndrome Proteus syndrome Cowden syndrome Bannayan–Riley–Ruvalcaba syndrome Lhermitte–Duclos disease Neurofibromatosis Type I Type II Other Abdallat–Davis–Farrage syndrome Ataxia telangiectasia Incontinentia pigmenti Peutz–Jeghers syndrome Encephalocraniocutaneous lipomatosis This article about a medical condition affecting the nervous system is a stub .
-
Abdallat–davis–farrage Syndrome
Wikipedia
Abdallat Davis Farrage syndrome Abdallat–Davis–Farrage syndrome has an autosomal recessive pattern of inheritance . Specialty Neurology Abdallat–Davis–Farrage syndrome is a form of phakomatosis , a disease of the central nervous system accompanied by skin abnormalities. ... The condition is named after the team of medical professionals who first wrote it up, describing the appearance of the syndrome in a family from Jordan. It was characterized in 1980 by Adnan Abdallat , a Jordanian doctor. [1] Contents 1 Signs and symptoms 2 Genetics 3 Diagnosis 4 Treatment 5 References 6 External links Signs and symptoms [ edit ] Albinism (hair) Irregular decreased skin pigmentation Excessive freckling Insensitivity to pain Paraparesis / quadraparesis Genetics [ edit ] The syndrome is thought to be inherited as an autosomal recessive genetic trait, meaning that in order to manifest symptoms, a person must inherit a gene for Abdallat–Davis–Farrage syndrome from both parents. ... "Disordered pigmentation, spastic paraparesis and peripheral neuropathy in three siblings: A new neurocutaneous syndrome" . Journal of Neurology, Neurosurgery, and Psychiatry . 43 (11): 962–966. doi : 10.1136/jnnp.43.11.962 . ... External links [ edit ] Classification D OMIM : 270750 MeSH : C536859 v t e Phakomatosis Angiomatosis Sturge–Weber syndrome Von Hippel–Lindau disease Hamartoma Tuberous sclerosis Hypothalamic hamartoma ( Pallister–Hall syndrome ) Multiple hamartoma syndrome Proteus syndrome Cowden syndrome Bannayan–Riley–Ruvalcaba syndrome Lhermitte–Duclos disease Neurofibromatosis Type I Type II Other Abdallat–Davis–Farrage syndrome Ataxia telangiectasia Incontinentia pigmenti Peutz–Jeghers syndrome Encephalocraniocutaneous lipomatosis This genetic disorder article is a stub .
-
Legius Syndrome
Wikipedia
Legius syndrome Other names Neurofibromatosis 1-like syndrome [1] This condition is inherited in an autosomal dominant manner. ... "Legius Syndrome" . GeneReviews . PMID 20945555 . Retrieved 1 June 2017 . update 2015 ^ a b [ http://ghr.nlm.nih.gov/condition/legius-syndrome "Legius syndrome", Genetics Home Reference, National Institutes of Health ^ a b "Legius syndrome | Genetic and Rare Diseases Information Center (GARD) – an NCATS Program" . rarediseases.info.nih.gov . ... "The RASopathies: Developmental syndromes of Ras/MAPK pathway dysregulation" . ... Review External links [ edit ] PubMed Classification D ICD - 10 : Q85.0 OMIM : 611431 MeSH : C548032 DiseasesDB : 34916 External resources GeneReviews : Legius Syndrome Orphanet : 137605 Scholia has a topic profile for Legius syndrome . v t e Phakomatosis Angiomatosis Sturge–Weber syndrome Von Hippel–Lindau disease Hamartoma Tuberous sclerosis Hypothalamic hamartoma ( Pallister–Hall syndrome ) Multiple hamartoma syndrome Proteus syndrome Cowden syndrome Bannayan–Riley–Ruvalcaba syndrome Lhermitte–Duclos disease Neurofibromatosis Type I Type II Other Abdallat–Davis–Farrage syndrome Ataxia telangiectasia Incontinentia pigmenti Peutz–Jeghers syndrome Encephalocraniocutaneous lipomatosis v t e Deficiencies of intracellular signaling peptides and proteins GTP-binding protein regulators GTPase-activating protein Neurofibromatosis type I Watson syndrome Tuberous sclerosis Guanine nucleotide exchange factor Marinesco–Sjögren syndrome Aarskog–Scott syndrome Juvenile primary lateral sclerosis X-Linked mental retardation 1 G protein Heterotrimeic cAMP / GNAS1 : Pseudopseudohypoparathyroidism Progressive osseous heteroplasia Pseudohypoparathyroidism Albright's hereditary osteodystrophy McCune–Albright syndrome CGL 2 Monomeric RAS: HRAS Costello syndrome KRAS Noonan syndrome 3 KRAS Cardiofaciocutaneous syndrome RAB: RAB7 Charcot–Marie–Tooth disease RAB23 Carpenter syndrome RAB27 Griscelli syndrome type 2 RHO: RAC2 Neutrophil immunodeficiency syndrome ARF : SAR1B Chylomicron retention disease ARL13B Joubert syndrome 8 ARL6 Bardet–Biedl syndrome 3 MAP kinase Cardiofaciocutaneous syndrome Other kinase / phosphatase Tyrosine kinase BTK X-linked agammaglobulinemia ZAP70 ZAP70 deficiency Serine/threonine kinase RPS6KA3 Coffin-Lowry syndrome CHEK2 Li-Fraumeni syndrome 2 IKBKG Incontinentia pigmenti STK11 Peutz–Jeghers syndrome DMPK Myotonic dystrophy 1 ATR Seckel syndrome 1 GRK1 Oguchi disease 2 WNK4 / WNK1 Pseudohypoaldosteronism 2 Tyrosine phosphatase PTEN Bannayan–Riley–Ruvalcaba syndrome Lhermitte–Duclos disease Cowden syndrome Proteus-like syndrome MTM1 X-linked myotubular myopathy PTPN11 Noonan syndrome 1 LEOPARD syndrome Metachondromatosis Signal transducing adaptor proteins EDARADD EDARADD Hypohidrotic ectodermal dysplasia SH3BP2 Cherubism LDB3 Zaspopathy Other NF2 Neurofibromatosis type II NOTCH3 CADASIL PRKAR1A Carney complex PRKAG2 Wolff–Parkinson–White syndrome PRKCSH PRKCSH Polycystic liver disease XIAP XIAP2 See also intracellular signaling peptides and proteins
-
Neutrophil Immunodeficiency Syndrome
Wikipedia
Neutrophil immunodeficiency syndrome Specialty Immunology Frequency <1 / 1 000 000 [1] Neutrophil immunodeficiency syndrome is a condition caused by mutations in the Rac2 gene. [2] See also [ edit ] Immunodeficiency with hyper-IgM List of cutaneous conditions Chronic granulomatous disease References [ edit ] ^ RESERVED, INSERM US14-- ALL RIGHTS. "Orphanet: Neutrophil immunodeficiency syndrome" . www.orpha.net . Retrieved 18 March 2019 . ^ Rapini, Ronald P.; Bolognia, Jean L.; Jorizzo, Joseph L. (2007). ... External links [ edit ] Classification D ICD - 10 : D71 OMIM : 608203 MeSH : C564275 SNOMED CT : 723443003 External resources Orphanet : 183707 v t e Diseases of monocytes and granulocytes Monocytes and macrophages ↑ -cytosis : Monocytosis Histiocytosis Chronic granulomatous disease ↓ -penia : Monocytopenia Granulocytes ↑ -cytosis : granulocytosis Neutrophilia Eosinophilia / Hypereosinophilic syndrome Basophilia Bandemia ↓ -penia : Granulocytopenia/agranulocytosis ( Neutropenia / Severe congenital neutropenia / Cyclic neutropenia Eosinopenia Basopenia ) Disorder of phagocytosis Chemotaxis and degranulation Leukocyte adhesion deficiency LAD1 LAD2 Chédiak–Higashi syndrome Neutrophil-specific granule deficiency Respiratory burst Chronic granulomatous disease Neutrophil immunodeficiency syndrome Myeloperoxidase deficiency v t e Deficiencies of intracellular signaling peptides and proteins GTP-binding protein regulators GTPase-activating protein Neurofibromatosis type I Watson syndrome Tuberous sclerosis Guanine nucleotide exchange factor Marinesco–Sjögren syndrome Aarskog–Scott syndrome Juvenile primary lateral sclerosis X-Linked mental retardation 1 G protein Heterotrimeic cAMP / GNAS1 : Pseudopseudohypoparathyroidism Progressive osseous heteroplasia Pseudohypoparathyroidism Albright's hereditary osteodystrophy McCune–Albright syndrome CGL 2 Monomeric RAS: HRAS Costello syndrome KRAS Noonan syndrome 3 KRAS Cardiofaciocutaneous syndrome RAB: RAB7 Charcot–Marie–Tooth disease RAB23 Carpenter syndrome RAB27 Griscelli syndrome type 2 RHO: RAC2 Neutrophil immunodeficiency syndrome ARF : SAR1B Chylomicron retention disease ARL13B Joubert syndrome 8 ARL6 Bardet–Biedl syndrome 3 MAP kinase Cardiofaciocutaneous syndrome Other kinase / phosphatase Tyrosine kinase BTK X-linked agammaglobulinemia ZAP70 ZAP70 deficiency Serine/threonine kinase RPS6KA3 Coffin-Lowry syndrome CHEK2 Li-Fraumeni syndrome 2 IKBKG Incontinentia pigmenti STK11 Peutz–Jeghers syndrome DMPK Myotonic dystrophy 1 ATR Seckel syndrome 1 GRK1 Oguchi disease 2 WNK4 / WNK1 Pseudohypoaldosteronism 2 Tyrosine phosphatase PTEN Bannayan–Riley–Ruvalcaba syndrome Lhermitte–Duclos disease Cowden syndrome Proteus-like syndrome MTM1 X-linked myotubular myopathy PTPN11 Noonan syndrome 1 LEOPARD syndrome Metachondromatosis Signal transducing adaptor proteins EDARADD EDARADD Hypohidrotic ectodermal dysplasia SH3BP2 Cherubism LDB3 Zaspopathy Other NF2 Neurofibromatosis type II NOTCH3 CADASIL PRKAR1A Carney complex PRKAG2 Wolff–Parkinson–White syndrome PRKCSH PRKCSH Polycystic liver disease XIAP XIAP2 See also intracellular signaling peptides and proteins This dermatology article is a stub .