-
Sleep State Misperception
Wikipedia
Sleep state misperception Other names Paradoxical insomnia, pseudo-insomnia, subjective insomnia, subjective sleepiness, sleep hypochondriasis [1] Specialty Sleep medicine Sleep state misperception ( SSM ) is a term in the International Classification of Sleep Disorders (ICSD) most commonly used for people who mistakenly perceive their sleep as wakefulness, [1] [2] though it has been proposed that it be applied to those who severely overestimate their sleep time as well [3] ("positive" sleep state misperception). [4] While most sleepers with this condition will report not having slept in the previous night at all or having slept very little, [5] clinical recordings generally show normal sleep patterns. ... Philadelphia: WB Saunders, 1994. [ page needed ] External links [ edit ] Classification D ICD - 10 : F51.0 , G47.0 ICD - 9-CM : 307.42 , 307.49 , 780.52 MeSH : D020919 DiseasesDB : 26877 SNOMED CT : 427745001 External resources eMedicine : med/2698 v t e Sleep and sleep disorders Stages of sleep cycles Rapid eye movement (REM) Non-rapid eye movement Slow-wave Brain waves Alpha wave Beta wave Delta wave Gamma wave K-complex Mu rhythm PGO waves Sensorimotor rhythm Sleep spindle Theta wave Sleep disorders Dyssomnia Excessive daytime sleepiness Hypersomnia Insomnia Kleine–Levin syndrome Narcolepsy Night eating syndrome Nocturia Sleep apnea Catathrenia Central hypoventilation syndrome Obesity hypoventilation syndrome Obstructive sleep apnea Periodic breathing Sleep state misperception Circadian rhythm disorders Advanced sleep phase disorder Cyclic alternating pattern Delayed sleep phase disorder Irregular sleep–wake rhythm Jet lag Non-24-hour sleep–wake disorder Shift work sleep disorder Parasomnia Bruxism Nightmare disorder Night terror Periodic limb movement disorder Rapid eye movement sleep behavior disorder Sleepwalking Somniloquy Benign phenomena Dreams Exploding head syndrome Hypnic jerk Hypnagogia / Sleep onset Hypnopompic state Sleep paralysis Sleep inertia Somnolence Nocturnal clitoral tumescence Nocturnal penile tumescence Nocturnal emission Treatment Sleep diary Sleep hygiene Sleep induction Hypnosis Lullaby Somnology Polysomnography Other Sleep medicine Behavioral sleep medicine Sleep study Daily life Bed Bunk bed Daybed Four-poster bed Futon Hammock Mattress Sleeping bag Bed bug Bedding Bedroom Bedtime Bedtime story Bedtime toy Biphasic and polyphasic sleep Chronotype Dream diary Microsleep Mouth breathing Nap Nightwear Power nap Second wind Siesta Sleep and creativity Sleep and learning Sleep deprivation / Sleep debt Sleeping while on duty Sleepover Snoring
-
Rhythmic Movement Disorder
Wikipedia
This may be due to RMD’s comorbidity with sleep apnea, which has been observed in some patients [6] . ... Other sleep related disorders like sleep apnea are ruled out by examining the patients’ respiratory effort, air flow, and oxygen saturation. ... In some patients who also experience sleep apnea, episodes of apnea can be followed immediately by RMD-like symptoms, suggesting that the apnea episodes may trigger an RMD episode. ... Infantile and adolescent RMD respond well to low doses of clonazepam . [19] Prescription medications such as ropinirole or pramipexole given to restless legs syndrome patients do not show any clinical improvement in many patients with RMD. [6] Non-medication [ edit ] Treatment of sleep apnea via a continuous positive airway pressure ( CPAP ) device has shown dramatic improvement in apnea and nearly complete resolution of RMD symptoms. [7] Behavioral interventions may alleviate some RMD symptoms and movements. ... "Rhythmic movement disorder associated with respiratory arousals and improved by CPAP titration in a patient with restless legs syndrome and sleep apnea". Sleep Med . 10 (4): 501–3. doi : 10.1016/j.sleep.2009.03.003 .
-
Carotid Artery Disease
Mayo_clinic
Excess weight increases the chances of high blood pressure, atherosclerosis and diabetes. Sleep apnea. Spells of stopping breathing at night might increase the risk of stroke. ... Being overweight increases other risk factors, such as high blood pressure, cardiovascular disease, diabetes and sleep apnea. Eat a healthy diet. Focus on fruits and vegetables, whole grains and fish, nuts and legumes. ... What do you eat in a typical day? Do you have symptoms of sleep apnea?APOE, CCL2, HMOX1, GSTP1, TP53, PODXL, AGT, FASLG, MRAS, CD163, PLAU, AGER, LTB4R, PON1, IL6, LPA, PLTP, PLG, TNFSF4, NOS3, MTHFR, SLC39A2, SHOC1, MMP9, HGF, CRP, IL1RN, CCL18, SELE, SREBF2, TNF, ACE, CYP27A1, TNFRSF4, VLDLR, PTGES, REN, TOMM40, CD14, MMRN1, APOB, EGFL7, BTNL2, PSRC1, ALOX5, NANOS3, EDN1, PTGS2, IGF1, HSPD1, IL10, IL10RA, INS, LIPC, ICAM1, LRP1, MET, MMP3, MPO, PPARG, NFKB1, NFKBIA, GSTT1, GNB3, FGB, F5, F3, CELSR2, MIR126
-
Exploding Head Syndrome
Wikipedia
External links [ edit ] Classification D ICD - 10 : G47.59 v t e Sleep and sleep disorders Stages of sleep cycles Rapid eye movement (REM) Non-rapid eye movement Slow-wave Brain waves Alpha wave Beta wave Delta wave Gamma wave K-complex Mu rhythm PGO waves Sensorimotor rhythm Sleep spindle Theta wave Sleep disorders Dyssomnia Excessive daytime sleepiness Hypersomnia Insomnia Kleine–Levin syndrome Narcolepsy Night eating syndrome Nocturia Sleep apnea Catathrenia Central hypoventilation syndrome Obesity hypoventilation syndrome Obstructive sleep apnea Periodic breathing Sleep state misperception Circadian rhythm disorders Advanced sleep phase disorder Cyclic alternating pattern Delayed sleep phase disorder Irregular sleep–wake rhythm Jet lag Non-24-hour sleep–wake disorder Shift work sleep disorder Parasomnia Bruxism Nightmare disorder Night terror Periodic limb movement disorder Rapid eye movement sleep behavior disorder Sleepwalking Somniloquy Benign phenomena Dreams Exploding head syndrome Hypnic jerk Hypnagogia / Sleep onset Hypnopompic state Sleep paralysis Sleep inertia Somnolence Nocturnal clitoral tumescence Nocturnal penile tumescence Nocturnal emission Treatment Sleep diary Sleep hygiene Sleep induction Hypnosis Lullaby Somnology Polysomnography Other Sleep medicine Behavioral sleep medicine Sleep study Daily life Bed Bunk bed Daybed Four-poster bed Futon Hammock Mattress Sleeping bag Bed bug Bedding Bedroom Bedtime Bedtime story Bedtime toy Biphasic and polyphasic sleep Chronotype Dream diary Microsleep Mouth breathing Nap Nightwear Power nap Second wind Siesta Sleep and creativity Sleep and learning Sleep deprivation / Sleep debt Sleeping while on duty Sleepover Snoring
-
Pure Autonomic Failure
Wikipedia
More pervasive autonomic dysfunction involving any of the following: night sweats or abnormal lack of sweating, urogenital problems (frequent UTIs, incontinence, frequency, urgency), gastrointestinal problems (chronic constipation, chronic constipation alternating with diarrhea, poor gastric motility), or esophageal/respiratory problems ( sleep apnea , abnormal breath sounds during sleep or while awake) indicate possible autoimmune autonomic ganglionopathy or multiple system atrophy .
-
Mucopolysaccharidosis Type Ii
Gene_reviews
Additional studies may include: sleep study for obstructive apnea; nerve conduction velocity to assess for carpal tunnel syndrome; head/neck MRI to document ventricular size and cervicomedullary narrowing; opening pressure on lumbar puncture; and orthopedic evaluation to monitor hip disease. ... Retinal degeneration leads to poor peripheral vision and night blindness, which occur frequently in individuals with MPS II, while central visual impairment due to retinal degeneration is rare [Suppiej et al 2013]. ... Ear, Nose, Throat Common oral findings in boys with MPS II include macroglossia, hypertrophic adenoids and tonsils, and ankylosis of the temporomandibular joint, which limits opening of the mouth. ... The progression of airway obstruction is relentless and usually results in sleep apnea and the need for positive pressure assistance and eventually tracheostomy. ... Visualization of the vocal cords is compromised by the large tongue, GAG-infiltrated soft tissues, and large tonsils and adenoids. Care must be taken to avoid hyperextension of the neck secondary to atlantoaxial instability and cervicomedullary compression that may be present.
-
Laryngospasm
Wikipedia
., "Laryngospam -The Best Treatment", Anesthesiology , 11 1998, Vol.89, 1293–1294 v t e Diseases of the respiratory system Upper RT (including URTIs , common cold ) Head sinuses Sinusitis nose Rhinitis Vasomotor rhinitis Atrophic rhinitis Hay fever Nasal polyp Rhinorrhea nasal septum Nasal septum deviation Nasal septum perforation Nasal septal hematoma tonsil Tonsillitis Adenoid hypertrophy Peritonsillar abscess Neck pharynx Pharyngitis Strep throat Laryngopharyngeal reflux (LPR) Retropharyngeal abscess larynx Croup Laryngomalacia Laryngeal cyst Laryngitis Laryngopharyngeal reflux (LPR) Laryngospasm vocal cords Laryngopharyngeal reflux (LPR) Vocal fold nodule Vocal fold paresis Vocal cord dysfunction epiglottis Epiglottitis trachea Tracheitis Laryngotracheal stenosis Lower RT / lung disease (including LRTIs ) Bronchial / obstructive acute Acute bronchitis chronic COPD Chronic bronchitis Acute exacerbation of COPD ) Asthma ( Status asthmaticus Aspirin-induced Exercise-induced Bronchiectasis Cystic fibrosis unspecified Bronchitis Bronchiolitis Bronchiolitis obliterans Diffuse panbronchiolitis Interstitial / restrictive ( fibrosis ) External agents/ occupational lung disease Pneumoconiosis Aluminosis Asbestosis Baritosis Bauxite fibrosis Berylliosis Caplan's syndrome Chalicosis Coalworker's pneumoconiosis Siderosis Silicosis Talcosis Byssinosis Hypersensitivity pneumonitis Bagassosis Bird fancier's lung Farmer's lung Lycoperdonosis Other ARDS Combined pulmonary fibrosis and emphysema Pulmonary edema Löffler's syndrome / Eosinophilic pneumonia Respiratory hypersensitivity Allergic bronchopulmonary aspergillosis Hamman-Rich syndrome Idiopathic pulmonary fibrosis Sarcoidosis Vaping-associated pulmonary injury Obstructive / Restrictive Pneumonia / pneumonitis By pathogen Viral Bacterial Pneumococcal Klebsiella Atypical bacterial Mycoplasma Legionnaires' disease Chlamydiae Fungal Pneumocystis Parasitic noninfectious Chemical / Mendelson's syndrome Aspiration / Lipid By vector/route Community-acquired Healthcare-associated Hospital-acquired By distribution Broncho- Lobar IIP UIP DIP BOOP-COP NSIP RB Other Atelectasis circulatory Pulmonary hypertension Pulmonary embolism Lung abscess Pleural cavity / mediastinum Pleural disease Pleuritis/pleurisy Pneumothorax / Hemopneumothorax Pleural effusion Hemothorax Hydrothorax Chylothorax Empyema/pyothorax Malignant Fibrothorax Mediastinal disease Mediastinitis Mediastinal emphysema Other/general Respiratory failure Influenza Common cold SARS Coronavirus disease 2019 Idiopathic pulmonary haemosiderosis Pulmonary alveolar proteinosis v t e Underwater diving Diving modes Atmospheric pressure diving Freediving Saturation diving Scuba diving Snorkeling Surface oriented diving Surface-supplied diving Unmanned diving Diving equipment Cleaning and disinfection of personal diving equipment Human factors in diving equipment design Basic equipment Diving mask Snorkel Swimfin Breathing gas Bailout gas Bottom gas Breathing air Decompression gas Emergency gas supply Heliox Nitrox Oxygen Travel gas Trimix Buoyancy and trim equipment Buoyancy compensator Power inflator Dump valve Diving weighting system Ankle weights Integrated weights Trim weights Weight belt Decompression equipment Decompression buoy Decompression cylinder Decompression trapeze Dive computer Diving shot Jersey upline Jonline Diving suit Atmospheric diving suit Dry suit Sladen suit Standard diving suit Rash vest Wetsuit Dive skins Hot-water suit Helmets and masks Anti-fog Diving helmet Free-flow helmet Lightweight demand helmet Orinasal mask Reclaim helmet Shallow water helmet Standard diving helmet Diving mask Band mask Full-face mask Half mask Instrumentation Bottom timer Depth gauge Dive computer Dive timer Diving watch Helium release valve Pneumofathometer Submersible pressure gauge Mobility equipment Diving bell Closed bell Wet bell Diving stage Swimfin Monofin PowerSwim Towboard Diver propulsion vehicle Advanced SEAL Delivery System Cosmos CE2F series Dry Combat Submersible Human torpedo Motorised Submersible Canoe Necker Nymph R-2 Mala-class swimmer delivery vehicle SEAL Delivery Vehicle Shallow Water Combat Submersible Siluro San Bartolomeo Wet Nellie Wet sub Safety equipment Alternative air source Octopus regulator Pony bottle Bolt snap Buddy line Dive light Diver's cutting tool Diver's knife Diver's telephone Through-water communications Diving bell Diving safety harness Emergency gas supply Bailout block Bailout bottle Lifeline Screw gate carabiner Emergency locator beacon Rescue tether Safety helmet Shark-proof cage Snoopy loop Navigation equipment Distance line Diving compass Dive reel Line marker Surface marker buoy Silt screw Underwater breathing apparatus Atmospheric diving suit Diving cylinder Burst disc Diving cylinder valve Diving helmet Reclaim helmet Diving regulator Mechanism of diving regulators Regulator malfunction Regulator freeze Single-hose regulator Twin-hose regulator Full face diving mask Open-circuit scuba Scuba set Bailout bottle Decompression cylinder Independent doubles Manifolded twin set Scuba manifold Pony bottle Scuba configuration Sidemount Sling cylinder Diving rebreathers Carbon dioxide scrubber Carleton CDBA CDLSE Cryogenic rebreather CUMA DSEA Dolphin Electro-galvanic oxygen sensor FROGS Halcyon PVR-BASC Halcyon RB80 IDA71 Interspiro DCSC KISS LAR-5 LAR-6 LAR-V LARU Porpoise Ray Siebe Gorman CDBA Siva Viper Surface-supplied diving equipment Air line Diver's umbilical Diving air compressor Gas panel Hookah Scuba replacement Sea Trek Snuba Standard diving dress Escape set Davis Submerged Escape Apparatus Momsen lung Steinke hood Submarine Escape Immersion Equipment Diving equipment manufacturers AP Diving Apeks Aqua Lung America Aqua Lung/La Spirotechnique Beuchat René Cavalero Cis-Lunar Cressi-Sub Dacor DESCO Dive Xtras Divex Diving Unlimited International Drägerwerk Fenzy Maurice Fernez Technisub Oscar Gugen Heinke HeinrichsWeikamp Johnson Outdoors Mares Morse Diving Nemrod Oceanic Worldwide Porpoise Sub Sea Systems Shearwater Research Siebe Gorman Submarine Products Suunto Diving support equipment Access equipment Boarding stirrup Diver lift Diving bell Diving ladder Diving platform (scuba) Diving stage Downline Jackstay Launch and recovery system Messenger line Moon pool Breathing gas handling Air filtration Activated carbon Hopcalite Molecular sieve Silica gel Booster pump Carbon dioxide scrubber Cascade filling system Diver's pump Diving air compressor Diving air filter Water separator High pressure breathing air compressor Low pressure breathing air compressor Gas blending Gas blending for scuba diving Gas panel Gas reclaim system Gas storage bank Gas storage quad Gas storage tube Helium analyzer Nitrox production Membrane gas separation Pressure swing adsorption Oxygen analyser Oxygen compatibility Decompression equipment Built-in breathing system Decompression tables Diving bell Bell cursor Closed bell Clump weight Launch and recovery system Wet bell Diving chamber Diving stage Recreational Dive Planner Saturation system Platforms Dive boat Canoe and kayak diving Combat Rubber Raiding Craft Liveaboard Subskimmer Diving support vessel HMS Challenger (K07) Underwater habitat Aquarius Reef Base Continental Shelf Station Two Helgoland Habitat Jules' Undersea Lodge Scott Carpenter Space Analog Station SEALAB Tektite habitat Remotely operated underwater vehicles 8A4-class ROUV ABISMO Atlantis ROV Team CURV Deep Drone Épaulard Global Explorer ROV Goldfish-class ROUV Kaikō ROV Kaşif ROUV Long-Term Mine Reconnaissance System Mini Rover ROV OpenROV ROV KIEL 6000 ROV PHOCA Scorpio ROV Sea Dragon-class ROV Seabed tractor Seafox drone Seahorse ROUV SeaPerch SJT-class ROUV T1200 Trenching Unit VideoRay UROVs Safety equipment Diver down flag Diving shot Hyperbaric lifeboat Hyperbaric stretcher Jackstay Jonline Reserve gas supply General Diving spread Air spread Saturation spread Hot water system Sonar Underwater acoustic positioning system Underwater acoustic communication Freediving Activities Aquathlon Apnoea finswimming Freediving Haenyeo Pearl hunting Ama Snorkeling Spearfishing Underwater football Underwater hockey Underwater ice hockey Underwater rugby Underwater target shooting Competitions Nordic Deep Vertical Blue Disciplines Constant weight (CWT) Constant weight without fins (CNF) Dynamic apnea (DYN) Dynamic apnea without fins (DNF) Free immersion (FIM) No-limits apnea (NLT) Static apnea (STA) Skandalopetra diving Variable weight apnea (VWT) Variable weight apnea without fins Equipment Diving mask Diving suit Hawaiian sling Polespear Snorkel (swimming) Speargun Swimfins Monofin Water polo cap Freedivers Deborah Andollo Peppo Biscarini Sara Campbell Derya Can Göçen Goran Čolak Carlos Coste Robert Croft Mandy-Rae Cruickshank Yasemin Dalkılıç Leonardo D'Imporzano Flavia Eberhard Şahika Ercümen Emma Farrell Francisco Ferreras Pierre Frolla Flavia Eberhard Mehgan Heaney-Grier Elisabeth Kristoffersen Loïc Leferme Enzo Maiorca Jacques Mayol Audrey Mestre Karol Meyer Stéphane Mifsud Alexey Molchanov Natalia Molchanova Dave Mullins Patrick Musimu Guillaume Néry Herbert Nitsch Umberto Pelizzari Annelie Pompe Michal Risian Stig Severinsen Tom Sietas Aharon Solomons Martin Štěpánek Walter Steyn Tanya Streeter William Trubridge Devrim Cenk Ulusoy Danai Varveri Alessia Zecchini Nataliia Zharkova Hazards Barotrauma Drowning Freediving blackout Deep-water blackout Shallow-water blackout Hypercapnia Hypothermia Historical Ama Octopus wrestling Swimming at the 1900 Summer Olympics – Men's underwater swimming Organisations AIDA International Scuba Schools International Australian Underwater Federation British Freediving Association Confédération Mondiale des Activités Subaquatiques Fédération Française d'Études et de Sports Sous-Marins Performance Freediving International Professional diving Occupations Ama Commercial diver Commercial offshore diver Hazmat diver Divemaster Diving instructor Diving safety officer Diving superintendent Diving supervisor Haenyeo Media diver Police diver Public safety diver Scientific diver Underwater archaeologist Military diving Army engineer diver Clearance diver Frogman List of military diving units Royal Navy ships diver Special Boat Service United States military divers U.S. ... Vandenberg HMS Ghurka Glen Strathallan SAS Good Hope Gothenburg Herzogin Cecilie Hilma Hooker Hispania HMS Hood HMAS Hobart Igara James Eagan Layne Captain Keith Tibbetts King Cruiser SMS Kronprinz Kyarra HMS Laforey USAT Liberty Louis Sheid USS LST-507 SMS Markgraf Mikhail Lermontov HMS M2 Maine Maloja HMS Maori Marguerite SS Mauna Loa USAT Meigs Mendi USCGC Mohawk Mohegan RMS Moldavia HMS Montagu MV RMS Mulheim Nagato Oceana USS Oriskany Oslofjord P29 P31 Pedernales Persier HMAS Perth SAS Pietermaritzburg Piłsudski Pool Fisher HMS Port Napier Preußen President Coolidge PS Queen Victoria Radaas Rainbow Warrior RMS Rhone Rondo Rosehill Rotorua Royal Adelaide Royal Charter Rozi HMS Safari Salem Express USS Saratoga USS Scuffle HMS Scylla HMS Sidon USS Spiegel Grove Stanegarth Stanwood Stella HMAS Swan USS Tarpon Thesis Thistlegorm Toa Maru Torrey Canyon SAS Transvaal U-40 U-352 U-1195 Um El Faroud Varvassi Walter L M Russ Washingtonian (1913) HMNZS Wellington USS Yancey Yongala Zenobia Zealandia Zingara Cave diving sites Blauhöhle Chinhoyi Caves Devil's Throat at Punta Sur Engelbrecht Cave Fossil Cave Jordbrugrotta Piccaninnie Ponds Pluragrotta Pollatoomary Sistema Ox Bel Ha Sistema Sac Actun Sistema Dos Ojos Sistema Nohoch Nah Chich Freshwater dives Dutch Springs Ewens Ponds Little Blue Lake Training sites Capernwray Dive Centre Deepspot National Diving and Activity Centre Stoney Cove Open ocean diving Blue-water diving Black-water diving Diving safety Human factors in diving equipment design Human factors in diving safety Life-support system Safety-critical system Scuba diving fatalities Diving hazards List of diving hazards and precautions Environmental Current Delta-P Entanglement hazard Overhead Silt out Wave action Equipment Freeflow Use of breathing equipment in an underwater environment Failure of diving equipment other than breathing apparatus Single point of failure Physiological Cold shock response Decompression Nitrogen narcosis Oxygen toxicity Seasickness Uncontrolled decompression Diver behaviour and competence Lack of competence Overconfidence effect Panic Task loading Trait anxiety Willful violation Consequences Barotrauma Decompression sickness Drowning Hypothermia Hypoxia Hypercapnia Hyperthermia Diving procedures Ascending and descending Emergency ascent Boat diving Canoe and kayak diving Buddy diving buddy check Decompression Decompression practice Pyle stop Ratio decompression Dive briefing Dive log Dive planning Scuba gas planning Diver communications Diving hand signals Diving line signals Diver voice communications Diver rescue Diver training Doing It Right Drift diving Gas blending for scuba diving Night diving Solo diving Water safety Risk management Checklist Hazard identification and risk assessment Hazard analysis Job safety analysis Risk assessment Risk control Hierarchy of hazard controls Incident pit Lockout–tagout Permit To Work Redundancy Safety data sheet Situation awareness Diving team Bellman Chamber operator Diver medical technician Diver's attendant Diving supervisor Diving systems technician Gas man Life support technician Stand-by diver Equipment safety Breathing gas quality Testing and inspection of diving cylinders Hydrostatic test Sustained load cracking Diving regulator Breathing performance of regulators Occupational safety and health Approaches to safety Job safety analysis Risk assessment Toolbox talk Housekeeping Association of Diving Contractors International Code of practice Contingency plan Diving regulations Emergency procedure Emergency response plan Evacuation plan Hazardous Materials Identification System Hierarchy of hazard controls Administrative controls Engineering controls Hazard elimination Hazard substitution Personal protective equipment International Marine Contractors Association Occupational hazard Biological hazard Chemical hazard Physical hazard Psychosocial hazard Occupational hygiene Exposure assessment Occupational exposure limit Workplace health surveillance Safety culture Code of practice Diving safety officer Diving superintendent Health and safety representative Operations manual Safety meeting Standard operating procedure Diving medicine Diving disorders List of signs and symptoms of diving disorders Cramp Motion sickness Surfer's ear Pressure related Alternobaric vertigo Barostriction Barotrauma Air embolism Aerosinusitis Barodontalgia Dental barotrauma Pulmonary barotrauma Compression arthralgia Decompression illness Dysbarism Oxygen Freediving blackout Hyperoxia Hypoxia Oxygen toxicity Inert gases Avascular necrosis Decompression sickness Isobaric counterdiffusion Taravana Dysbaric osteonecrosis High-pressure nervous syndrome Hydrogen narcosis Nitrogen narcosis Carbon dioxide Hypercapnia Hypocapnia Breathing gas contaminants Carbon monoxide poisoning Immersion related Asphyxia Drowning Hypothermia Immersion diuresis Instinctive drowning response Laryngospasm Salt water aspiration syndrome Swimming-induced pulmonary edema Treatment Demand valve oxygen therapy First aid Hyperbaric medicine Hyperbaric treatment schedules In-water recompression Oxygen therapy Therapeutic recompression Personnel Diving Medical Examiner Diving Medical Practitioner Diving Medical Technician Hyperbaric nursing Screening Atrial septal defect Effects of drugs on fitness to dive Fitness to dive Psychological fitness to dive Research Researchers in diving physiology and medicine Arthur J. ... Navy Diving Manual Basic Cave Diving: A Blueprint for Survival Underwater Handbook Bennett and Elliott's physiology and medicine of diving Encyclopedia of Recreational Diving The new science of skin and scuba diving Professional Diver's Handbook Basic Scuba Standards and Codes of Practice Code of Practice for Scientific Diving (UNESCO) DIN 7876 IMCA Code of Practice for Offshore Diving ISO 24801 Recreational diving services — Requirements for the training of recreational scuba divers General non-fiction The Darkness Beckons Goldfinder The Last Dive Shadow Divers The Silent World: A Story of Undersea Discovery and Adventure Research List of Divers Alert Network publications Dive guides Training and registration Diver training Competence and assessment Competency-based learning Refresher training Skill assessment Diver training standard Diving instructor Diving school Occupational diver training Commercial diver training Military diver training Public safety diver training Scientific diver training Recreational diver training Introductory diving Teaching method Muscle memory Overlearning Stress exposure training Skills Combat sidestroke Diver navigation Diver trim Ear clearing Frenzel maneuver Valsalva maneuver Finning techniques Scuba skills Buddy breathing Low impact diving Diamond Reef System Surface-supplied diving skills Underwater searches Recreational scuba certification levels Core diving skills Advanced Open Water Diver Autonomous diver CMAS* scuba diver CMAS** scuba diver Introductory diving Low Impact Diver Master Scuba Diver Open Water Diver Supervised diver Leadership skills Dive leader Divemaster Diving instructor Master Instructor Specialist skills Rescue Diver Solo diver Diver training certification and registration organisations European Underwater Federation (EUF) International Diving Regulators and Certifiers Forum (IDRCF) International Diving Schools Association (IDSA) International Marine Contractors Association (IMCA) List of diver certification organizations National Oceanic and Atmospheric Administration (NOAA) Nautical Archaeology Society Universal Referral Program World Recreational Scuba Training Council (WRSTC) Commercial diver certification authorities Australian Diver Accreditation Scheme (ADAS) Commercial diver registration in South Africa Divers Institute of Technology Health and Safety Executive (HSE) Department of Employment and Labour Commercial diving schools Divers Academy International Norwegian diver school Free-diving certification agencies AIDA International (AIDA) Confédération Mondiale des Activités Subaquatiques (CMAS) Performance Freediving International (PI) Scuba Schools International (SSI) Recreational scuba certification agencies American Canadian Underwater Certifications (ACUC) American Nitrox Divers International (ANDI) Association nationale des moniteurs de plongée (ANMP) British Sub-Aqua Club (BSAC) Comhairle Fo-Thuinn (CFT) Confédération Mondiale des Activités Subaquatiques (CMAS) Federación Española de Actividades Subacuáticas (FEDAS) Fédération Française d'Études et de Sports Sous-Marins (FFESSM) Federazione Italiana Attività Subacquee (FIAS) Global Underwater Explorers (GUE) International Association for Handicapped Divers (IAHD) International Association of Nitrox and Technical Divers (IANTD) International Diving Educators Association (IDEA) Israeli Diving Federation (TIDF) National Academy of Scuba Educators (NASE) National Association of Underwater Instructors (NAUI) Nederlandse Onderwatersport Bond (NOB) Professional Association of Diving Instructors (PADI) Professional Diving Instructors Corporation (PDIC) Sub-Aqua Association (SAA) Scuba Diving International (SDI) Scuba Educators International (SEI) Scottish Sub Aqua Club (ScotSAC) Scuba Schools International (SSI) Türkiye Sualtı Sporları Federasyonu (TSSF) United Diving Instructors (UDI) YMCA SCUBA Program Scientific diver certification authorities American Academy of Underwater Sciences (AAUS) CMAS Scientific Committee Technical certification agencies American Nitrox Divers International (ANDI) British Sub-Aqua Club (BSAC) Confédération Mondiale des Activités Subaquatiques (CMAS) Diving Science and Technology (DSAT) Federazione Italiana Attività Subacquee (FIAS) International Association of Nitrox and Technical Divers (IANTD) Professional Association of Diving Instructors (PADI) Professional Diving Instructors Corporation (PDIC) Trimix Scuba Association (TSA) Technical Extended Range (TXR) Cave diving Cave Divers Association of Australia (CDAA) Cave Diving Group (CDG) Global Underwater Explorers (GUE) National Association for Cave Diving (NACD) National Speleological Society#Cave Diving Group (CDG) National Association of Underwater Instructors (NAUI) Technical Diving International (TDI) Underwater sports Surface snorkeling Finswimming Snorkeling/breath-hold Spearfishing Underwater football Underwater hockey Australia Turkey Underwater rugby Colombia United States Underwater target shooting Breath-hold Aquathlon Apnoea finswimming Freediving Underwater ice hockey Open Circuit Scuba Immersion finswimming Sport diving Underwater cycling Underwater orienteering Underwater photography Rebreather Underwater photography Sports governing organisations and federations International AIDA International Confédération Mondiale des Activités Subaquatiques ) National AIDA Hellas Australian Underwater Federation British Freediving Association British Octopush Association British Underwater Sports Association Comhairle Fo-Thuinn Federación Española de Actividades Subacuáticas Fédération Française d'Études et de Sports Sous-Marins South African Underwater Sports Federation Türkiye Sualtı Sporları Federasyonu Underwater Society of America ) Competitions 14th CMAS Underwater Photography World Championship Underwater divers Pioneers of diving Eduard Admetlla i Lázaro Aquanaut James F. ... Barnette Victor Berge Philippe Diolé Gary Gentile Bret Gilliam Bob Halstead Trevor Jackson Steve Lewis John Mattera Rescuers Craig Challen Richard Harris Rick Stanton John Volanthen Frogmen Lionel Crabb Commercial salvors Keith Jessop Science of underwater diving Diving physics Breathing performance of regulators Buoyancy Archimedes' principle Neutral buoyancy Concentration Diffusion Molecular diffusion Force Oxygen fraction Permeation Psychrometric constant Solubility Henry's law Saturation Solution Supersaturation Surface tension Hydrophobe Surfactant Temperature Torricellian chamber Underwater acoustics Modulated ultrasound Underwater vision Snell's law Underwater computer vision Weight Apparent weight Gas laws Amontons's law Boyle's law Charles's law Combined gas law Dalton's law Gay-Lussac's law Ideal gas law Pressure Absolute pressure Ambient pressure Atmospheric pressure Gauge pressure Hydrostatic pressure Metre sea water Partial pressure Diving physiology Artificial gills Cold shock response Diving reflex Equivalent narcotic depth Lipid Maximum operating depth Metabolism Physiological response to water immersion Tissue Underwater vision Circulatory system Blood shift Patent foramen ovale Perfusion Pulmonary circulation Systemic circulation Decompression theory Decompression models: Bühlmann decompression algorithm Haldane's decompression model Reduced gradient bubble model Thalmann algorithm Thermodynamic model of decompression Varying Permeability Model Equivalent air depth Equivalent narcotic depth Oxygen window in diving decompression Physiology of decompression Respiration Blood–air barrier Breathing CO₂ retention Dead space Gas exchange Hypocapnia Respiratory exchange ratio Respiratory quotient Respiratory system Work of breathing Diving environment Classification List of diving environments by type Altitude diving Benign water diving Confined water diving Deep diving Inland diving Inshore diving Muck diving Night diving Open-water diving Black-water diving Blue-water diving Penetration diving Cave diving Ice diving Wreck diving Recreational dive sites Underwater environment Impact Environmental impact of recreational diving Low impact diving Environmental factors Algal bloom Currents: Current Longshore drift Ocean current Rip current Tidal race Undertow Upwelling Ekman transport Halocline Reef Coral reef Stratification Thermocline Tides Turbidity Wind wave Breaking wave Surf Surge Wave shoaling Other Bathysphere Defense against swimmer incursions Diver detection sonar Offshore survey Underwater domain awareness Awards and events Hans Hass Award International Scuba Diving Hall of Fame London Diving Chamber Dive Lectures NOGI Awards Deep-submergence vehicle Aluminaut DSV Alvin American submarine NR-1 Bathyscaphe Archimède FNRS-2 FNRS-3 FNRS-4 Harmony class bathyscaphe Sea Pole -class bathyscaphe Trieste II Deepsea Challenger Ictineu 3 JAGO Jiaolong Konsul -class submersible DSV Limiting Factor Russian submarine Losharik Mir Nautile Pisces -class deep submergence vehicle DSV Sea Cliff DSV Shinkai DSV Shinkai 2000 DSV Shinkai 6500 DSV Turtle DSV-5 Nemo Deep-submergence rescue vehicle LR5 LR7 MSM-1 Mystic -class deep-submergence rescue vehicle DSRV-1 Mystic DSRV-2 Avalon NATO Submarine Rescue System Priz -class deep-submergence rescue vehicle Russian deep submergence rescue vehicle AS-28 Russian submarine AS-34 ASRV Remora SRV-300 Submarine Rescue Diving Recompression System Type 7103 DSRV URF (Swedish Navy) Special interest groups Artificial Reef Society of British Columbia CMAS Europe Coral Reef Alliance Diving Equipment and Marketing Association Divers Alert Network Green Fins Historical Diving Society Karst Underwater Research Nautical Archaeology Program Nautical Archaeology Society Naval Air Command Sub Aqua Club Project AWARE Reef Check Reef Life Survey Rubicon Foundation Save Ontario Shipwrecks SeaKeys Sea Research Society Society for Underwater Historical Research Society for Underwater Technology Underwater Archaeology Branch, Naval History & Heritage Command Submarine escape and rescue Escape trunk International Submarine Escape and Rescue Liaison Office McCann Rescue Chamber Submarine Escape and Rescue system (Royal Swedish Navy) Submarine escape training facility Submarine Escape Training Facility (Australia) Submarine rescue ship Neutral buoyancy facilities for Astronaut training Neutral Buoyancy Laboratory Neutral buoyancy pool Neutral buoyancy simulation as a training aid Neutral Buoyancy Simulator Space Systems Laboratory Yuri Gagarin Cosmonaut Training Center Other Nautilus Productions Category Commons Glossary Indexes: dive sites divers diving Outline PortalSCN4A, ANXA11, SOD1, TAF1, TSPYL1, VCP, TAF15, SQSTM1, VAPB, MATR3, FIG4, OPTN, ANG, UNC13A, TARDBP, CHMP2B, SRPX2, TBK1, UBQLN2, TREM2, GLT8D1, UBE3B, C9orf72, PPARGC1A, ATXN2, PRPH, GLE1, BTD, CFAP410, CCNF, DAO, DCTN1, EPHA4, ERBB4, FUS, GABRG2, GRIN2A, PON3, HNRNPA1, LAMA3, LAMB3, LAMC2, NEFH, NEK1, PFN1, PON1, PON2, CHCHD10
-
Restless Legs Syndrome
Mayo_clinic
Worsening of symptoms in the evening. Symptoms occur mainly at night. Nighttime leg twitching. RLS may be associated with another, more common condition called periodic limb movement of sleep, which causes the legs to twitch and kick, possibly throughout the night, while you sleep. ... Your symptoms are partially or temporarily relieved by activity, such as walking or stretching. Your symptoms are worse at night. Symptoms can't be explained solely by another medical or behavioral condition. ... This may involve an overnight stay and a study at a sleep clinic if another sleep disorder such as sleep apnea is suspected. However, a diagnosis of RLS usually doesn't require a sleep study. ... These drugs help you sleep better at night, but they don't eliminate the leg sensations, and they may cause daytime drowsiness. ... Do your symptoms start while you're sitting or lying down? Are your symptoms worse at night? Does movement make you feel better?BTBD9, MEIS1, PTPRD, TF, POMC, DRD3, MAP2K5, SNCA, PRKN, MFN2, LRRK2, PARK7, FTL, HTRA2, VPS13C, DNAJC6, ATXN7, LINC02086, PINK1, UCHL1, RLS1, CASC16, PODXL, MYT1, LINC02520, LINC01478, CCDC148, SKOR1, HMOX1, TOX3, DRD2, VDR, MAOA, RLS3, CHM, FXYD1, TH, CHMP2B, SLC11A2, ATXN1, HAMP, GABRR3, RLS4, RLS6, NTS, ADH1B, HMOX2, CRP, GABRA4, FXN, EEF1A2, DMRT1, KNG1, IL1B, HFE, MPZ, MAOB, NOS1, ATXN3, ZC4H2, MIXL1, REEP1, AVP, PCDHA3, MOCOS, FAT2, GABRR2, NANS, SLC25A37, ATL1, PYCARD, GCH1, FMR1, C3, TRAPPC6B, CAD, TMPRSS6, DRD4, GLO1, C9orf72, DBP, MIR122, LINC00423, MIR330, RLS2, CPT1B, CHKB, RLS5, KCTD18, NPAS2, SPATS2L, MCF2L, NKX2-1, TFRC, IL17A, TRA, AFP, SLC6A3, SLC1A2, L1CAM, ATXN2, LRP2, TSPAN31, REN, LY6E, SMCP, SERPINA1, TNF, TYMS, IGLC2, SCAF11, CNTN3, HNMT, ZEB2, IGHA1, LITAF, SLC9A3R2, APLN, UTRN, RNMT, GEMIN2, ATRN, FGF23, NR4A3, IGKC, TBP
-
Tonsillitis
Wikipedia
"Circulating phospholipase-A2 activity in obstructive sleep apnea and recurrent tonsillitis". Int J Pediatr Otorhinolaryngol . 76 (4): 471–4. doi : 10.1016/j.ijporl.2011.12.026 . PMID 22297210 . ^ van Kempen MJ, Rijkers GT, Van Cauwenberge PB (May 2000). "The immune response in adenoids and tonsils". Int. Arch. Allergy Immunol. ... "Tissue fatty acid composition in obstructive sleep apnea and recurrent tonsillitis". Int J Pediatr Otorhinolaryngol . 77 (6): 1008–12. doi : 10.1016/j.ijporl.2013.03.033 . ... Wetmore RF (2007). "Tonsils and adenoids". In Kliegman RM, Behrman RE, Jenson HB, Stanton BF (eds.). ... Classification D ICD - 10 : J03 , J35.0 ICD - 9-CM : 463 MeSH : D014069 DiseasesDB : 13165 External resources MedlinePlus : 001043 eMedicine : article/871977 Patient UK : Tonsillitis v t e Diseases of the respiratory system Upper RT (including URTIs , common cold ) Head sinuses Sinusitis nose Rhinitis Vasomotor rhinitis Atrophic rhinitis Hay fever Nasal polyp Rhinorrhea nasal septum Nasal septum deviation Nasal septum perforation Nasal septal hematoma tonsil Tonsillitis Adenoid hypertrophy Peritonsillar abscess Neck pharynx Pharyngitis Strep throat Laryngopharyngeal reflux (LPR) Retropharyngeal abscess larynx Croup Laryngomalacia Laryngeal cyst Laryngitis Laryngopharyngeal reflux (LPR) Laryngospasm vocal cords Laryngopharyngeal reflux (LPR) Vocal fold nodule Vocal fold paresis Vocal cord dysfunction epiglottis Epiglottitis trachea Tracheitis Laryngotracheal stenosis Lower RT / lung disease (including LRTIs ) Bronchial / obstructive acute Acute bronchitis chronic COPD Chronic bronchitis Acute exacerbation of COPD ) Asthma ( Status asthmaticus Aspirin-induced Exercise-induced Bronchiectasis Cystic fibrosis unspecified Bronchitis Bronchiolitis Bronchiolitis obliterans Diffuse panbronchiolitis Interstitial / restrictive ( fibrosis ) External agents/ occupational lung disease Pneumoconiosis Aluminosis Asbestosis Baritosis Bauxite fibrosis Berylliosis Caplan's syndrome Chalicosis Coalworker's pneumoconiosis Siderosis Silicosis Talcosis Byssinosis Hypersensitivity pneumonitis Bagassosis Bird fancier's lung Farmer's lung Lycoperdonosis Other ARDS Combined pulmonary fibrosis and emphysema Pulmonary edema Löffler's syndrome / Eosinophilic pneumonia Respiratory hypersensitivity Allergic bronchopulmonary aspergillosis Hamman-Rich syndrome Idiopathic pulmonary fibrosis Sarcoidosis Vaping-associated pulmonary injury Obstructive / Restrictive Pneumonia / pneumonitis By pathogen Viral Bacterial Pneumococcal Klebsiella Atypical bacterial Mycoplasma Legionnaires' disease Chlamydiae Fungal Pneumocystis Parasitic noninfectious Chemical / Mendelson's syndrome Aspiration / Lipid By vector/route Community-acquired Healthcare-associated Hospital-acquired By distribution Broncho- Lobar IIP UIP DIP BOOP-COP NSIP RB Other Atelectasis circulatory Pulmonary hypertension Pulmonary embolism Lung abscess Pleural cavity / mediastinum Pleural disease Pleuritis/pleurisy Pneumothorax / Hemopneumothorax Pleural effusion Hemothorax Hydrothorax Chylothorax Empyema/pyothorax Malignant Fibrothorax Mediastinal disease Mediastinitis Mediastinal emphysema Other/general Respiratory failure Influenza Common cold SARS Coronavirus disease 2019 Idiopathic pulmonary haemosiderosis Pulmonary alveolar proteinosis Authority control NDL : 00563120GALNS, PAGR1, GAST, MBL3P, VDR, IFNG, IL1B, MBL2, DEFB1, RXRB, TRBV20OR9-2, S100A7, CCL20, CCL24, SKP1, SOD2, BCL2, TNFSF13, TLR4, PRCP, PDLIM7, ANP32B, CCL27, PART1, TLR9, AICDA, RNASE2, LTF, MTHFR, CCNB1, CDKN2A, EGFR, FANCD2, FCN2, GEM, GPX1, HIF1A, HLA-B, HLA-C, IGHG3, IL6, CXCL8, IL10, KIR2DS1, KIR3DL1, KIR3DL2, LTA, FDCSP
-
Apert Syndrome
Gene_reviews
If airway obstruction is present, temporizing measures may be required. Treatment of sleep apnea by surgical intervention and/or supplemental oxygen via nasal cannula may be required. ... Agents/circumstances to avoid: Contact sports and activities that involve neck hyperflexion or extension for those with cervical spine anomalies; factors that potentiate hearing loss; use of CPAP/BiPAP for long-term treatment of sleep apnea. Pregnancy management: For affected pregnant women: monitoring for signs and symptoms of worsening obstructive sleep apnea and anethesia evaluation prior to initiation of labor to identify any multilevel airway anomalies or vertebral anomalies that would result in additional risk with certain types of anesthesia; fiberoptic intubation could be required. ... Avoid use of CPAP/BiPAP for long-term treatment of sleep apnea when possible because pressure on midface exacerbates midfacial retrusion. Supplemental oxygen via nasal cannula is sometimes beneficial. Reducing sleep apnea & improving sleep quality has the potential to improve learning, cognition, & behavior. ... Use of CPAP/BiPAP for long-term treatment of sleep apnea should be avoided when possible because pressure on the midface will exacerbate midfacial retrusion.
-
Maroteaux–lamy Syndrome
Wikipedia
It may be necessary to remove the tonsils and/or adenoids. Severe tracheomalacia may require surgery. ... Aggressive management of airway secretions is necessary as well. Sleep apnea may be treated with a CPAP or BPAP device. [5] Prognosis [ edit ] A slowly-progressing female patient in her 20s, showing few physical abnormalities The life expectancy of individuals with MPS VI varies depending on the severity of symptoms.
-
Confusional Arousals
Wikipedia
The altered state of consciousness may be explained by a hypersynchronous delta activity (see delta wave ) in network involving the frontoparietal cortices (suggesting to be "asleep"), and higher frequency activities in sensorimotor, orbitofrontal, and temporal lateral cortices (suggesting an "awakening"). [6] [7] Sleep-related violence and abnormal sexual behaviours [ edit ] Confusional arousals have often been linked to sleep-related violence (self-injury or injury to the bed partner). [8] [9] [10] [11] The latter highlights important medical and legal issues when such behaviours are suspected and purported to have caused a criminal offense. [12] The first documented case of homicide as a result of confusional arousal was reported in medieval times by the case of the Silesian woodcutter Bernard Schedmaizig. [13] Sleep-related abnormal sexual behaviours (also called sexsomnia or sleep sex ) are mainly classified as confusional arousals and more rarely associated to sleepwalking (also known as somnambulism). [12] Even if sleep-related violence may occur during an episode of confusional arousal, it remains extremely rare and there are no specific predisposition to aggression during these episodes. [8] Distinction between sleepwalking and night terrors [ edit ] Violent behaviours in confusional arousals slightly differ from those in sleepwalking or night terrors. [8] Above all, during an episode of confusional arousal the patient never leaves the bed unlike sleepwalking. ... Unlike confusional arousals and sleep walking, patients experiencing night terrors seem to react to some type of frightening image. ... NREM parasomnias (or disorders of arousal) also include sleep terrors (see night terror ) and sleepwalking . Confusional arousals are characterised by more or less complex movements without leaving bed with whimpering, sitting up in bed and some articulation without walking or terror. [14] [15] In comparison of other arousal parasomnias the age onset of sleep walking is generally between 5 and 10 years whereas confusional arousals and sleep terror may occur 3 years earlier. ... According to studies, [2] [21] [22] they are shift work, hypnagogic hallucinations (also known as hypnagogia ), excessive daytime sleepiness, insomnia and hypersomnia disorder, circadian rhythm sleep disorder , restless legs syndrome , obstructive sleep apnea syndrome (OSAS), bipolar disorder , daily smoking, and age of 15–24 years. ... G.; Guilleminault, C.; Ohayon, M. M. (April 1999). "Night terrors, sleepwalking, and confusional arousals in the general population: their frequency and relationship to other sleep and mental disorders".
-
Glaucoma-Sleep Apnea Syndrome
Orphanet
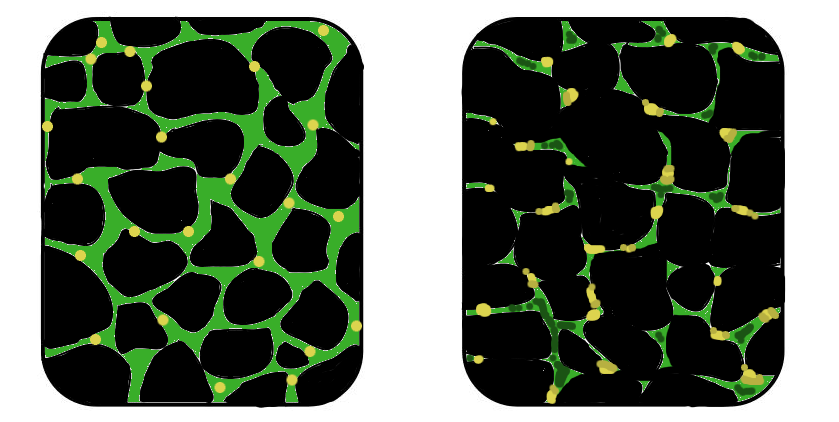
Glaucoma-sleep apnea syndrome is characterized by sleep apnoea associated with glaucoma.
-
Pitt-Hopkins Syndrome
Gene_reviews
Sleep disturbance in childhood is reported in fewer than half of affected individuals [Whalen et al 2012] and includes difficulty falling asleep, problems sleeping through the night, and night terrors [de Winter et al 2016]. ... Episodic hyperventilation often followed by breath-holding/apnea while awake are reported in 40%-60% of individuals [Whalen et al 2012, de Winter et al 2016, Goodspeed et al 2018]. ... However, in most affected individuals breathing abnormalities persist to some degree, though too few adults have been described to make conclusive statements about frequency or severity. Breath-holding/apnea episodes are not typically related to seizure activity [Maini et al 2012]. ... The breathing abnormality in PTHS does not appear to be a manifestation of seizure activity [Maini et al 2012], though in this study, 7/38 individuals with seizures had apnea or hyperventilation shortly before their seizures. ... Polysomnography may be indicated if there is a history of episodic apnea, especially when associated with cyanosis (typically alternating with episodes of hyperventilation).
-
Shift Work Sleep Disorder
Wikipedia
It is believed that the reduction in firing in the SCN stimulates sleep. [30] While day-active individuals produce melatonin at night, night shift workers' production of melatonin is suppressed at night due to light exposure. [31] Circadian misalignment [ edit ] Circadian misalignment plays a major role in shift work sleep disorder. ... A nap before starting a night shift is a logical prophylactic measure. ... "Dark goggles and bright light improve circadian rhythm adaptation to night-shift work" . Sleep . 17 (6): 535–43. doi : 10.1093/sleep/17.6.535 . ... "The effects of caffeine on simulated night-shift work and subsequent daytime sleep" . ... "Sleepiness/alertness on a simulated night shift following sleep at home with triazolam" .
-
Phosphoenolpyruvate Carboxykinase Deficiency, Cytosolic
Omim
He also had frequent attacks of cyanosis and apnea. At age 8 weeks, he showed general retardation and atrophy of the optic nerve. ... He had no signs of infection, but had been very active the night before. Lactate, pyruvate, and ammonia were normal, free fatty acids were elevated, and GPT was slightly elevated. ... INHERITANCE - Autosomal recessive HEAD & NECK Eyes - Optic nerve atrophy RESPIRATORY - Apnea, episodic ABDOMEN Liver - Enlarged liver - Fatty infiltration - Portal inflammation, mild to moderate Portal fibrosis, mild - Patchy to diffuse macrovesicular steatosis - Acute liver failure, transient (in 1 patient) SKIN, NAILS, & HAIR Skin - Cyanosis NEUROLOGIC Central Nervous System - Seizures (in some patients) - Hepatic encephalopathy (in 1 patient) METABOLIC FEATURES - Cytosolic phosphoenolpyruvate carboxykinase deficiency - Impaired gluconeogenesis - Fasting hypoglycemia - Lactic acidemia - Normal to elevated blood ammonia - Elevated blood alanine aminotransferase - Normal to high plasma glutamine - Normal to low plasma citrulline - Normal to low plasma arginine - Ketonuria - Elevated urine lactate - Prominent tricarboxylic acid cycle metabolites in urine (particularly fumarate) MISCELLANEOUS - Onset in infancy ▲ Close
-
Jet Lag
Wikipedia
Cognitive effects include poorer performance on mental tasks and concentration ; dizziness, nausea , insomnia , confusion, anxiety , increased fatigue , headaches , and irritability ; and problems with digestion, including indigestion , changes in the frequency of defecation and consistency of faeces , and reduced interest in and enjoyment of food. [2] The symptoms are caused by a circadian rhythm that is out of sync with the day-night cycle of the destination, [3] as well as the possibility of internal desynchronisation. ... Travel fatigue can occur without crossing time zones, and it often disappears after one day accompanied by a night of good quality sleep. [3] Cause [ edit ] Jet lag is a chronobiological problem, [6] similar to issues often induced by shift work and the circadian rhythm sleep disorders. ... Equally important, the necessary exposure to light to realign the body clock does not tie in with the day/night cycle at the destination. [3] Travelling east by six to nine time zones causes the biggest problems, as it is desirable to avoid light in the mornings. ... Management when travelling west [ edit ] Travelling west causes fewer problems than travelling east, and it is usually sufficient to seek exposure to light during the day and avoid it at night. [3] The advice is to prepare by having late sleep times the days before, and to travel daytime (not so early that early wakeup is needed) and to sleep some on board in order to be less tired at arrival and during ground transfer. ... External links [ edit ] Classification D ICD - 10 : G47.25 ICD - 9-CM : 307.45 , 780.50 327.35 MeSH : D021081 DiseasesDB : 7045 v t e Sleep and sleep disorders Stages of sleep cycles Rapid eye movement (REM) Non-rapid eye movement Slow-wave Brain waves Alpha wave Beta wave Delta wave Gamma wave K-complex Mu rhythm PGO waves Sensorimotor rhythm Sleep spindle Theta wave Sleep disorders Dyssomnia Excessive daytime sleepiness Hypersomnia Insomnia Kleine–Levin syndrome Narcolepsy Night eating syndrome Nocturia Sleep apnea Catathrenia Central hypoventilation syndrome Obesity hypoventilation syndrome Obstructive sleep apnea Periodic breathing Sleep state misperception Circadian rhythm disorders Advanced sleep phase disorder Cyclic alternating pattern Delayed sleep phase disorder Irregular sleep–wake rhythm Jet lag Non-24-hour sleep–wake disorder Shift work sleep disorder Parasomnia Bruxism Nightmare disorder Night terror Periodic limb movement disorder Rapid eye movement sleep behavior disorder Sleepwalking Somniloquy Benign phenomena Dreams Exploding head syndrome Hypnic jerk Hypnagogia / Sleep onset Hypnopompic state Sleep paralysis Sleep inertia Somnolence Nocturnal clitoral tumescence Nocturnal penile tumescence Nocturnal emission Treatment Sleep diary Sleep hygiene Sleep induction Hypnosis Lullaby Somnology Polysomnography Other Sleep medicine Behavioral sleep medicine Sleep study Daily life Bed Bunk bed Daybed Four-poster bed Futon Hammock Mattress Sleeping bag Bed bug Bedding Bedroom Bedtime Bedtime story Bedtime toy Biphasic and polyphasic sleep Chronotype Dream diary Microsleep Mouth breathing Nap Nightwear Power nap Second wind Siesta Sleep and creativity Sleep and learning Sleep deprivation / Sleep debt Sleeping while on duty Sleepover Snoring
-
Binge Eating
Wikipedia
With obesity comes a myriad of health complications: sleep apnea , cancer , heart disease , high blood pressure , type 2 diabetes , arthritis . [6] Effects [ edit ] Typically the eating is done rapidly and a person will feel emotionally numb and unable to stop eating. [7] Most people who have eating binges try to hide this behavior from others, and often feel ashamed about being overweight or depressed about their overeating. ... He also reported that some of these cases unhealthy eating habits were seen during a time period he called “night eating”. After this report, the terminology of “Binge Eating” caught on for diagnosing the episodes of infrequent eating of large amounts of food, whether or not the episode is connected with night eating. [11] 1987: The APA's DSM [ edit ] The American Psychiatric Association (APA) mentioned and listed Binge Eating under the listed criteria and features of Bulimia in the Diagnostic and Statistical Manual of Mental Disorders (DSM) - 3 in 1987.
-
Muscular Dystrophy
Mayo_clinic
People with muscular dystrophy might eventually need to use a breathing assistance device (ventilator), initially at night but possibly also during the day. ... As respiratory muscles weaken, a sleep apnea device might help improve oxygen delivery during the night.LAMA2, FKTN, DMD, COL6A1, SELENON, FKRP, SGCA, DYSF, CAPN3, SGCG, ANO5, DAG1, SGCD, TTN, SGCB, TRIM32, PRIMA1, TCAP, BCHE, ACHE, DES, LMNA, PLEC, LDB3, TRIM63, CAV3, CAVIN1, TOR1AIP1, POMGNT1, POMT1, COL6A3, COL6A2, GMPPB, POMT2, LARGE1, BAG3, CHKB, B3GALNT2, DNAJB6, CRPPA, NR0B1, B4GAT1, LIMS2, POMGNT2, INPP5K, RXYLT1, BVES, SYNE2, SYNE1, TNPO3, BEST1, PSAT1, NEB, SIL1, PMM2, RYR1, HSPB8, PIEZO2, PHGDH, HNRNPA2B1, DOK7, RIF1, DPM1, BUB3, DPM3, TRIP13, TRIP4, POMK, CEP57, TMEM43, PNKP, PYROXD1, TTN-AS1, HNRNPA1, BUB1B, COL4A1, CRYAB, AHCY, MSTN, GK, COL12A1, BUB1, EMD, UTRN, SSPN, IGF1, TRIM72, MYOT, SMCHD1, FSHMD1A, LTBP4, DMPK, ANO1, MB, TRPV2, LRRC7, ANPEP, CCN2, TRAF3, HMGCR, FRG1, FLNC, FHL1, HSPA8, MYOF, STAT5A, SPP1, CHKA, SGCE, DTNA, ANXA6, ORAI1, FST, IL6, DUX4, TNFRSF11B, ACTB, KITLG, MIR21, JAG1, ITGA7, NR3C2, LIF, CUX1, MMD, DCN, MIR222, LARGE2, MIR29C, NAT9, MIR188, MIR146A, MIR130B, KIF7, SUN1, DLG4, MIR30C1, DPEP1, DUSP6, CELF1, B3GNT2, GJB6, CCR2, WWP1, MIR486-1, ACE, DNMT3B, DUSP10, DNAH8, MIR340, MIR30C2, ACTN3, HPGDS, ACVR2B, LAMA1, MUL1, HAMP, TRAPPC11, AQP4, AQP1, APRT, EGFLAM, TNFAIP8L2, TOR1A, ANXA2, SETD7, OBSCN, ANXA1, B4GALNT2, TPH2, KIDINS220, BGN, CMD1B, CD38, EFEMP2, PCSK9, TRAT1, SIDT2, ZCCHC17, PARP1, ANO6, POGLUT1, ANO10, COL22A1, MSTO1, RUNX1T1, CBLL2, AGL, MCOLN1, MSC, PPIF, MMP10, MSN, MYOD1, HLA-C, NPC1, NPPA, P2RX7, SERPINE1, PRKN, PEG3, PIK3C2A, PITX2, PLAT, HIVEP1, HCFC1, PNN, PPARD, PPID, PRG2, PKN1, MPZ, MMP9, MATR3, MMP8, IDH2, IL1B, IL2RB, IMPA1, INPP5B, ITPR1, ITPR3, KRT14, LAMB2, LCN2, LGALS3, HLA-E, LMNB1, LPA, SMAD3, MAFD2, MBL2, MCL1, MFAP1, MAP2K6, RAG1, RAG2, PLAAT4, WNT7A, CNBP, PABPN1, GCY, TNFSF11, TNFRSF11A, BANF1, DPM2, SYNJ1, SYNJ2, MGAM, FMR1, HP, KL, ADIPOQ, ESR2, GOSR2, ENO1, HDAC9, GEM, VDAC3, GH1, GJB1, REN, BRD2, ROS1, GPT, S100B, SDC2, GLB1, GJB2, SHOX, TIMP1, SI, SMN1, SNTB1, SOD1, SPN, STIM1, TERF1, TGFB1, ABCA4
-
Ritscher-Schinzel Syndrome
Gene_reviews
Treatment of manifestations: Standard treatment for obesity, obstructive sleep apnea, cleft palate, congenital heart defects, hypercholesterolemia, renal anomalies, immunodeficiency, and developmental delay / intellectual disability. Surveillance : Measurement of growth parameters (particularly weight); assessment of developmental progress, mobility, self-help skills, and educational needs; and monitoring for symptoms of obstructive sleep apnea at each visit; ophthalmology evaluation annually or as clinically indicated; measurement of lipid profile periodically starting in childhood. ... In those w/obesity who have symptoms of sleep apnea Craniofacial Clinical assessment for cleft palate &/or micrognathia Consider referral to craniofacial clinic. ... Treatment of Manifestations in Individuals with Ritscher-Schinzel Syndrome View in own window Manifestation/Concern Treatment Considerations/Other Obesity Standard treatment Incl referral to nutritional specialists to monitor food intake & weight Obstructive sleep apnea Standard treatment May incl weight control, removal of tonsils/adenoids, &/or CPAP Cleft palate Standard surgical treatment, ideally by a specialized craniofacial team Congenital heart defects Standard treatment Hypercholesterolemia Standard treatment incl consideration of oral HMG-CoA reductase inhibitors (statins) 1 Other considerations incl optimizing weight, ↑ physical activity, & optimizing dietary fiber intake Renal anomalies Standard treatment per urologist &/or nephrologist Immunodeficiency Standard treatment per immunologist Family/Community Ensure appropriate social work involvement to connect families w/local resources, respite, & support. ... Recommended Surveillance for Individuals with Ritscher-Schinzel Syndrome View in own window System/Concern Evaluation Frequency Eyes Ophthalmology evaluation Annually or as clinically indicated Cardiovascular Lipid profile 1 Periodically 2 Constitutional Measurement of growth parameters, particularly weight Each visit Respiratory Monitor for symptoms of obstructive sleep apnea. Musculoskeletal Physical medicine, OT/PT assessment of mobility, self-help skills Development Monitor developmental progress & educational needs.