Osteopenia

Osteopenia, preferably known as "low bone mass" or "low bone density", is a condition in which bone mineral density is low. Because their bones are weaker, people with osteopenia may have a higher risk of fractures, and some people may go on to develop osteoporosis. In 2010, 43 million older adults in the US had osteopenia. Unlike osteoporosis, osteopenia does not usually cause symptoms, and losing bone density in itself does not cause pain.
There is no single cause for osteopenia, although there are several risk factors, including modifiable (behavioral, including dietary and use of certain drugs) and non-modifiable (for instance, loss of bone mass with age). For people with risk factors, screening via a DXA scanner may help to detect the development and progression of low bone density. Prevention of low bone density may begin early in life and includes a healthy diet and weight-bearing exercise, as well as avoidance of tobacco and alcohol. The treatment of osteopenia is controversial: non-pharmaceutical treatment involves preserving existing bone mass via healthy behaviors (dietary modification, weight-bearing exercise, avoidance or cessation of smoking or heavy alcohol use). Pharmaceutical treatment for osteopenia, including bisphosphonates and other medications, may be considered in certain cases but is not without risks. Overall, treatment decisions should be guided by considering each patient's constellation of risk factors for fractures.

Risk factors
Many divide risk factors for osteopenia into fixed (non-changeable) and modifiable factors. Osteopenia can also be secondary to other diseases. An incomplete list of risk factors:
Fixed
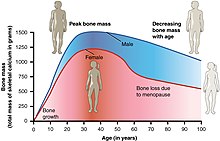
- Age: bone density peaks at age 35, and then decreases. Bone density loss occurs in both men and women
- Ethnicity: European and Asian people have increased risk
- Sex: women are at higher risk, particularly those with early menopause
- Family history: low bone mass in the family increases risk
Modifiable / behavioral
- Tobacco use
- Alcohol use
- Inactivity – particularly lack of weight-bearing or resistance activities
- Insufficient caloric intake - osteopenia can be connected to female athlete triad syndrome, which occurs in female athletes as a combination of energy deficiency, menstrual irregularities, and low bone mineral density.
- Low nutrient diet (particularly calcium, Vitamin D)
Other diseases
- Celiac disease, via poor absorption of calcium and vitamin D
- Hyperthyroidism
- Anorexia nervosa
Medications
- Steroid
- Anticonvulsants
Screening and diagnosis
The ISCD (International Society for Clinical Densitometry) and the National Osteoporosis Foundation recommend that older adults (women over 65 and men over 70) and adults with risk factors for low bone mass, or previous fragility fractures, undergo DXA testing. The DXA (dual X-ray absorptiometry) scan uses a form of X-ray technology, and offers accurate bone mineral density results with low radiation exposure.
The United States Preventive Task Force recommends osteoporosis screening for women with increased risk over 65 and states there is insufficient evidence to support screening men. The main purpose of screening is to prevent fractures. Of note, USPSTF screening guidelines are for osteoporosis, not specifically osteopenia.

The National Osteoporosis Foundation recommends use of central (hip and spine) DXA testing for accurate measure of bone density, emphasizing that peripheral or "screening" scanners should not be used to make clinically meaningful diagnoses, and that peripheral and central DXA scans cannot be compared to each other.
DXA scanners can be used to diagnose osteopenia or osteoporosis as well as to measure bone density over time as people age or undergo medical treatment or lifestyle changes.
Information from the DXA scanner creates a bone mineral density T-score by comparing a patient's density to the bone density of a healthy young person. Bone density between 1 and 2.5 standard deviations below the reference, or a T-score between −1.0 and −2.5, indicates osteopenia (a T-score greater than or equal to −2.5 indicates osteoporosis). Calculation of the T-score itself may not be standardized. The ISCD recommends using Caucasian women between 20 and 29 years old as the baseline for bone density for ALL patients, but not all facilities follow this recommendation.
The ISCD recommends that Z-scores, not T-scores, be used to classify bone density in premenopausal women and men under 50.
Prevention
Prevention of low bone density can start early in life by maximizing peak bone density. Once a person loses bone density, the loss is usually irreversible, so preventing (greater than normal) bone loss is important.
Actions to maximize bone density and stabilize loss include:
- Exercise, particularly weight-bearing exercise and resistance exercises
- Adequate caloric intake
- Sufficient calcium in diet: older adults may have increased calcium needs—of note, medical conditions such as Celiac and hyperthyroidism can affect absorption of calcium
- Sufficient Vitamin D in diet
- Estrogen replacement
- Avoidance of steroid medications
- Limit alcohol use and smoking
Pharmaceutical treatment
The pharmaceutical treatment of osteopenia is controversial and more nuanced than well-supported recommendations for improved nutrition and weight-bearing exercise. The diagnosis of osteopenia in and of itself does not always warrant pharmaceutical treatment. Many people with osteopenia may be advised to follow risk prevention measures (as above).
Risk of fracture guides clinical treatment decisions: the World Health Organization (WHO) Fracture Risk Assessment Tool (FRAX) estimates the probability of hip fracture and the probability of a major osteoporotic fracture (MOF), which could occur in a bone other than the hip. In addition to bone density (T-score), calculation of the FRAX score involves age, body characteristics, health behaviors, and other medical history.
As of 2014, The National Osteoporosis Foundation (NOF) recommends pharmaceutical treatment for osteopenic postmenopausal women and men over 50 with FRAX hip fracture probability of >3% or FRAX MOF probability >20%. As of 2016, the American Association of Clinical Endocrinologists and the American College of Endocrinology agree. In 2017, the American College of Physicians recommended that clinicians use individual judgment and knowledge of patients' particular risk factors for fractures, as well as patient preferences, to decide whether to pursue pharmaceutical treatment for women with osteopenia over 65.
Pharmaceutical treatment for low bone density includes a range of medications. Commonly used drugs include bisphosphonates (alendronate, risedronate, and ibandronate)—some studies show that decreased fracture risk and increased bone density after bisphosphonate treatment for osteopenia. Other medications include selective estrogen receptor modulators (SERMs) (e.g., raloxifene), estrogens (e.g., estradiol), calcitonin, and parathyroid hormone-related protein analogues (e.g., abaloparatide, teriparatide).
These drugs are not without risks. In this complex landscape, many argue that clinicians must consider a patient's individual risk of fracture, not simply treat those with osteopenia as equally at risk. A 2005 editorial in the Annals of Internal Medicine states "The objective of using osteoporosis drugs is to prevent fractures. This can be accomplished only by treating patients who are likely to have a fracture, not by simply treating T-scores."
History
Osteopenia, from Greek ὀστέον (ostéon), "bone" and πενία (penía), "poverty", is a condition of sub-normally mineralized bone, usually the result of a rate of bone lysis that exceeds the rate of bone matrix synthesis. See also osteoporosis.
In June 1992, the World Health Organization defined osteopenia. An osteoporosis epidemiologist at the Mayo Clinic who participated in setting the criterion in 1992 said "It was just meant to indicate the emergence of a problem", and noted that "It didn't have any particular diagnostic or therapeutic significance. It was just meant to show a huge group who looked like they might be at risk."
See also
- Bone mineral density
- Osteoporosis