Tako-Tsubo Cardiomyopathy
A rare cardiac disease characterized by acute occurrence of heart failure after an emotional or physical trigger however, recovery of the wall motion abnormalities are observed within months. Symptoms are similar to acute coronary syndrome (ACS).
Epidemiology
Takotsubo syndrome (TTS) is found in about 1-3% of all patients with symptoms of ACS; however, the prevalence is likely underestimated. Around 90% of TTS patients are women, typically postmenopausal but male and younger patients are diagnosed increasingly due to raised awareness of the syndrome.
Clinical description
In the acute phase, clinical presentation, electrocardiography (ECG) and cardiac biomarkers are similar to those of ACS. Typical symptoms are acute chest pain or dyspnea. Further symptoms can arise from complications of TTS, e.g. heart failure, cardiogenic shock, or cardiac arrest. New ECG changes or elevated cardiac biomarkers may or may not be present.
Etiology
The underlying mechanisms of this syndrome remain incompletely understood. Recent findings show that specific alterations in neurological response and sympathetic activation after emotional stimuli are present in TTS. These findings confirm the importance of brain-heart interaction in the development of this process. Microcirculatory constriction is also proposed as an underlying mechanism.
Diagnostic methods
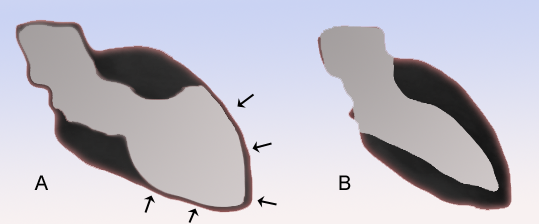
Diagnosis is often challenging due to the similarity with ACS. Coronary angiography with left ventriculography is considered the gold standard diagnostic tool. The InterTAK (international takotsubo) Diagnostic Criteria have been developed to improve diagnosis and include the following: 1) transient left ventricular dysfunction presenting as either apical, midventricular, basal or focal wall motion abnormalities with possible right ventricular involvement, 2) a preceding emotional, physical, or combined trigger (although not obligatory), 3) neurological disorders can be possible triggers, 4) presence of new ECG abnormalities (ST-segment elevation or depression, T-wave inversion, or QTc prolongation), 5) elevated cardiac markers (especially brain natriuretic peptide), 6) significant coronary artery disease can coexist, 7) absence of myocarditis.
Differential diagnosis
Differential diagnoses include AMI, myocarditis, spontaneous coronary artery dissection, or peripartum cardiomyopathy.
Management and treatment
Due to difficulty in distinguishing TTS from ACS, patients should be transferred to a chest pain unit upon presentation and receive guideline based treatment of ACS. There are no randomized clinical trials to support specific acute or long term treatment recommendations in TTS. However, the consensus statement from an international TTS expert panel provides recommendations for optimal treatment of TTS patients. Electrocardiogram monitoring is essential as a prolonged QT-interval may trigger malignant ventricular arrhythmias (torsades de pointes) or atrioventricular-block. Cardiogenic shock or post cardiac arrest requires intensive care with treatment according to the presence or absence of pulmonary edema, low left ventricular ejection fraction, hypotension and bradycardia. In all cases, inotropic substances should be avoided. For long term treatment, angiotensin converting-enzyme inhibitors (ACEi) or angiotensin II receptor blockers (ARB) are recommended as they are associated with improved survival and lower recurrence rates. Echocardiography should be performed during the acute phase to exclude right ventricular involvement, left ventricular outflow tract obstruction or intraventricular thrombus. A follow-up echocardiography should be performed after discharge to confirm recovery.
Prognosis
The spectrum of TTS is wide and ranges from low to very high risk. In-hospital mortality and long-term outcome in TTS are similar compared to ACS. Recovery of the left ventricular regional systolic dysfunction is usually observed after 4-8 weeks. The risk of recurrence is around 5%.