Acute Intermittent Porphyria
Acute intermittent porphyria (AIP) is a rare metabolic disorder affecting the production of heme resulting from a deficiency of the porphobilinogen deaminase. It is the most common of the acute porphyrias.
Signs and symptoms
The clinical presentation of AIP is highly variable and non-specific. The patients are typically asymptomatic, with most gene carriers having no family history because the condition had remained latent for several generations. The syndrome marked by acute attacks affects only 10% of gene carriers. The mean age at diagnosis is 33 years old. Like other porphyrias, AIP is more likely to present in women. A distinguishing feature of AIP that separates it from other porphyrias is the absence of photosensitive cutaneous symptoms that occur in addition to acute attacks.
Acute attacks
AIP is one of the four porphyrias that presents as an acute attack. 90% of affected individuals never experience an acute attack and are asymptomatic, while an estimated 5% of affected individuals experience repeat attacks. Attacks are most common in young adult women and are rare before puberty or after menopause. Severe acute attacks may require hospitalization. Patients usually experience symptoms in attacks that last from several hours to a few days. Between attacks, patients are asymptomatic.
The most frequent presenting symptoms are abdominal pain and tachycardia. The abdominal pain is typically severe, colicky, poorly localized, and often associated with pain in back and legs. Patients may also present with vomiting and constipation, but diarrhea is unusual. The onset of back and leg pain is characterized by severe pain and stiffness in back and thighs followed by loss of tendon reflexes and paralysis. Psychiatric symptoms are present, such as paranoid schizophrenia-like features but rarely psychosis and hallucinations. The acute attacks classically present with dark-red photosensitive urine (often called port-wine urine), but this is a nonspecific symptom. Physical examination often shows no abnormalities.
Hyponatremia is the most common electrolyte abnormality during acute attacks, occurring in 40% of patients and presenting as SIADH. Hypomagnesemia is also common. There are no pathognomonic signs or symptoms.
The most common identified triggers for acute attacks are medications, weight loss diets, and surgery. Many medications have been associated with AIP including antibiotics, hormonal contraceptives, seizure medications, anesthetics, and HIV treatment drugs.
Pathophysiology
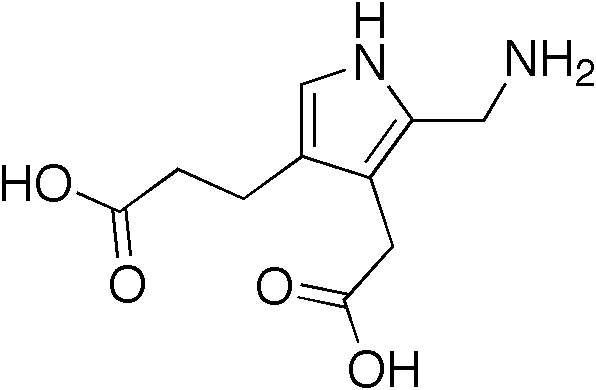
Porphyrias are caused by mutations in genes that encode enzymes in heme synthesis. In normal physiology, heme synthesis begins in the mitochondrion, proceeds into the cytoplasm, and finishes back in the mitochondrion. Heme is produced in all cells, but 80% of all heme is produced in erythropoietic cells in bone marrow and 15% in parenchymal cells in the liver, where turnover of hemoproteins is high. In AIP, over 100 mutations have been identified on the long arm of chromosome 11 at the HMBS gene, which codes for the cytoplasmic enzyme porphobilinogen deaminase. This deficiency prevents heme synthesis, which can not be completed and the metabolite porphobilinogen accumulates in the cytoplasm.
AIP is an autosomal dominant porphyria resulting in about 50% normal activity of the affected enzyme. The penetrance of AIP is incomplete with only 10% of gene carriers experiencing acute attacks suggesting role for other modifying genes or environment.
The exact mechanism of acute attacks is not clear. The most favored hypothesis is that porpholobilinogen buildup causes a toxic effects on neurons. The autonomic and peripheral nervous system are more vulnerable than the central nervous system because they are not protected by the blood-brain barrier. This explains findings such as abdominal pain and tachycardia. Some individuals may be more likely to develop paresis based on increased susceptibility of neurons to toxins.
Diagnosis
The initial diagnosis of acute porphyria is confirmed by urinalysis, including the common method, the Watson-Schwartz test. Elevated urine porphobilinogen confirms diagnosis of AIP, hereditary coproporphyria (HCP), or variegate porphyria (VP). A positive test should be indicated with an increase of five times normal, not just a slight increase which can occur with dehydration. To distinguish between AIP from HCP and VP, fecal porphyrin levels are normal in AIP but elevated in HCP and VP.
Rapid, accurate diagnosis is important. Delays in diagnosis may result in permanent neurological damage or death.
Treatment
If drugs have caused the attack, discontinuing the offending substances is essential. A high-carbohydrate (10% glucose) infusion is recommended, which may aid in recovery.

Hematin and heme arginate is the treatment of choice during an acute attack. Heme is not a curative treatment, but can shorten attacks and reduce the intensity of an attack. Side-effects are rare but can be serious. Pain is extremely severe and almost always requires the use of opiates to reduce it to tolerable levels. Pain should be treated as early as medically possible due to its severity.
Nausea can be severe; it may respond to phenothiazine drugs but is sometimes intractable. Hot water baths or showers may lessen nausea temporarily, but can present a risk of burns or falls.
Seizures often accompany this disease. Most seizure medications exacerbate this condition due to their induction of cytochrome P450. Treatment can be problematic: Barbiturates and primidone must be avoided as they commonly precipitate symptoms. Some benzodiazepines are safe, and, when used in conjunction with newer anti-seizure medications such as gabapentin, offer a possible regimen for seizure control.
Society
One of the many hypothesized diagnoses of the artist Vincent van Gogh is that he and his siblings, in particular his brother Theo, suffered from AIP and syphilis. Another theorized sufferer was King George III of the United Kingdom who even had a medallion struck to commemorate his "curing". His descendant Prince William of Gloucester was reliably diagnosed with variegate porphyria in 1968. It is probable that the philosopher Jean-Jacques Rousseau suffered from porphyria. It has even been suggested that Vlad III, Prince of Wallachia, more commonly known by his surname Dracula, suffered from porphyria.