Endometrial Cancer
Endometrial cancer is a cancer that arises from the endometrium (the lining of the uterus or womb). It is the result of the abnormal growth of cells that have the ability to invade or spread to other parts of the body. The first sign is most often vaginal bleeding not associated with a menstrual period. Other symptoms include pain with urination, pain during sexual intercourse, or pelvic pain. Endometrial cancer occurs most commonly after menopause.
Approximately 40% of cases are related to obesity. Endometrial cancer is also associated with excessive estrogen exposure, high blood pressure and diabetes. Whereas taking estrogen alone increases the risk of endometrial cancer, taking both estrogen and a progestogen in combination, as in most birth control pills, decreases the risk. Between two and five percent of cases are related to genes inherited from the parents. Endometrial cancer is sometimes loosely referred to as "uterine cancer", although it is distinct from other forms of uterine cancer such as cervical cancer, uterine sarcoma, and trophoblastic disease. The most frequent type of endometrial cancer is endometrioid carcinoma, which accounts for more than 80% of cases. Endometrial cancer is commonly diagnosed by endometrial biopsy or by taking samples during a procedure known as dilation and curettage. A pap smear is not typically sufficient to show endometrial cancer. Regular screening in those at normal risk is not called for.
The leading treatment option for endometrial cancer is abdominal hysterectomy (the total removal by surgery of the uterus), together with removal of the Fallopian tubes and ovaries on both sides, called a bilateral salpingo-oophorectomy. In more advanced cases, radiation therapy, chemotherapy or hormone therapy may also be recommended. If the disease is diagnosed at an early stage, the outcome is favorable, and the overall five-year survival rate in the United States is greater than 80%.
In 2012, endometrial cancers newly occurred in 320,000 women and caused 76,000 deaths. This makes it the third most common cause of death in cancers which only affect women, behind ovarian and cervical cancer. It is more common in the developed world and is the most common cancer of the female reproductive tract in developed countries. Rates of endometrial cancer have risen in a number of countries between the 1980s and 2010. This is believed to be due to the increasing number of elderly people and increasing rates of obesity.
 Play media
Play mediaSigns and symptoms
Vaginal bleeding or spotting in women after menopause occurs in 90% of endometrial cancer. Bleeding is especially common with adenocarcinoma, occurring in two-thirds of all cases. Abnormal menstrual cycles or extremely long, heavy, or frequent episodes of bleeding in women before menopause may also be a sign of endometrial cancer.
Symptoms other than bleeding are not common. Other symptoms include thin white or clear vaginal discharge in postmenopausal women. More advanced disease shows more obvious symptoms or signs that can be detected on a physical examination. The uterus may become enlarged or the cancer may spread, causing lower abdominal pain or pelvic cramping. Painful sexual intercourse or painful or difficult urination are less common signs of endometrial cancer. The uterus may also fill with pus (pyometrea). Of women with these less common symptoms (vaginal discharge, pelvic pain, and pus), 10–15% have cancer.
Risk factors
Risk factors for endometrial cancer include obesity, diabetes mellitus, breast cancer, use of tamoxifen, never having had a child, late menopause, high levels of estrogen, and increasing age. Immigration studies (migration studies), which examine the change in cancer risk in populations moving between countries with different rates of cancer, show that there is some environmental component to endometrial cancer. These environmental risk factors are not well characterized.
Hormones
Most of the risk factors for endometrial cancer involve high levels of estrogens. An estimated 40% of cases are thought to be related to obesity. In obesity, the excess of adipose tissue increases conversion of androstenedione into estrone, an estrogen. Higher levels of estrone in the blood causes less or no ovulation and exposes the endometrium to continuously high levels of estrogens. Obesity also causes less estrogen to be removed from the blood. Polycystic ovary syndrome (PCOS), which also causes irregular or no ovulation, is associated with higher rates of endometrial cancer for the same reasons as obesity. Specifically, obesity, type II diabetes, and insulin resistance are risk factors for Type I endometrial cancer. Obesity increases the risk for endometrial cancer by 300–400%.
Estrogen replacement therapy during menopause when not balanced (or "opposed") with progestin is another risk factor. Higher doses or longer periods of estrogen therapy have higher risks of endometrial cancer. Women of lower weight are at greater risk from unopposed estrogen. A longer period of fertility—either from an early first menstrual period or late menopause—is also a risk factor. Unopposed estrogen raises an individual's risk of endometrial cancer by 2–10 fold, depending on weight and length of therapy. In trans men who take testosterone and have not had a hysterectomy, the conversion of testosterone into estrogen via androstenedione may lead to a higher risk of endometrial cancer.
Genetics

Genetic disorders can also cause endometrial cancer. Overall, hereditary causes contribute to 2–10% of endometrial cancer cases. Lynch syndrome, an autosomal dominant genetic disorder that mainly causes colorectal cancer, also causes endometrial cancer, especially before menopause. Women with Lynch syndrome have a 40–60% risk of developing endometrial cancer, higher than their risk of developing colorectal (bowel) or ovarian cancer. Ovarian and endometrial cancer develop simultaneously in 20% of people. Endometrial cancer nearly always develops before colon cancer, on average, 11 years before. Carcinogenesis in Lynch syndrome comes from a mutation in MLH1 or MLH2: genes that participate in the process of mismatch repair, which allows a cell to correct mistakes in the DNA. Other genes mutated in Lynch syndrome include MSH2, MSH6, and PMS2, which are also mismatch repair genes. Women with Lynch syndrome represent 2–3% of endometrial cancer cases; some sources place this as high as 5%. Depending on the gene mutation, women with Lynch syndrome have different risks of endometrial cancer. With MLH1 mutations, the risk is 54%; with MSH2, 21%; and with MSH6, 16%.
Women with a family history of endometrial cancer are at higher risk. Two genes most commonly associated with some other women's cancers, BRCA1 and BRCA2, do not cause endometrial cancer. There is an apparent link with these genes but it is attributable to the use of tamoxifen, a drug that itself can cause endometrial cancer, in breast and ovarian cancers. The inherited genetic condition Cowden syndrome can also cause endometrial cancer. Women with this disorder have a 5–10% lifetime risk of developing endometrial cancer, compared to the 2–3% risk for unaffected women.
Common genetic variation has also been found to affect endometrial cancer risk in large-scale genome-wide association studies. Sixteen genomic regions have been associated with endometrial cancer and the common variants explain up to 7% of the familial relative risk.
Other health problems
Some therapies for other forms of cancer increase the lifetime risk of endometrial cancer, which is a baseline 2–3%. Tamoxifen, a drug used to treat estrogen-positive breast cancers, has been associated with endometrial cancer in approximately 0.1% of users, particularly older women, but the benefits for survival from tamoxifen generally outweigh the risk of endometrial cancer. A one to two-year course of tamoxifen approximately doubles the risk of endometrial cancer, and a five-year course of therapy quadruples that risk. Raloxifene, a similar drug, did not raise the risk of endometrial cancer. Previously having ovarian cancer is a risk factor for endometrial cancer, as is having had previous radiotherapy to the pelvis. Specifically, ovarian granulosa cell tumors and thecomas are tumors associated with endometrial cancer.
Low immune function has also been implicated in endometrial cancer. High blood pressure is also a risk factor, but this may be because of its association with obesity. Sitting regularly for prolonged periods is associated with higher mortality from endometrial cancer. The risk is not negated by regular exercise, though it is lowered.
Protective factors
Smoking and the use of progestin are both protective against endometrial cancer. Smoking provides protection by altering the metabolism of estrogen and promoting weight loss and early menopause. This protective effect lasts long after smoking is stopped. Progestin is present in the combined oral contraceptive pill and the hormonal intrauterine device (IUD). Combined oral contraceptives reduce risk more the longer they are taken: by 56% after four years, 67% after eight years, and 72% after twelve years. This risk reduction continues for at least fifteen years after contraceptive use has been stopped. Obese women may need higher doses of progestin to be protected. Having had more than five infants (grand multiparity) is also a protective factor, and having at least one child reduces the risk by 35%. Breastfeeding for more than 18 months reduces risk by 23%. Increased physical activity reduces an individual's risk by 38–46%. There is preliminary evidence that consumption of soy is protective.
Pathophysiology
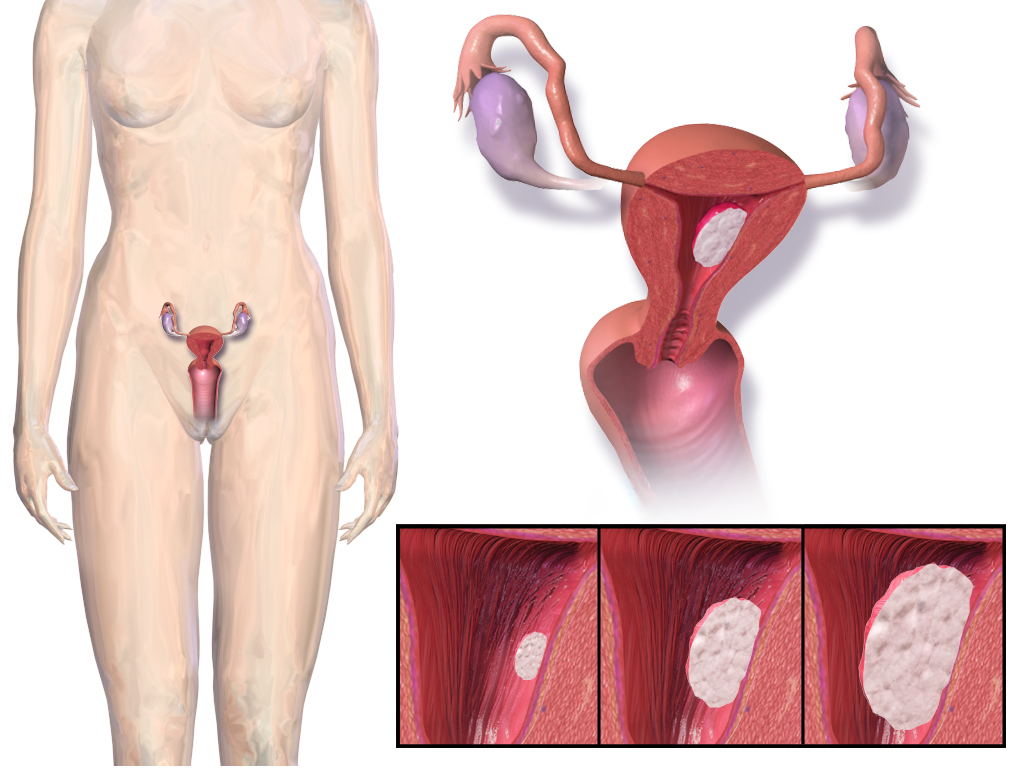
 A diagram showing the female reproductive tract with the uterine wall enlarged and normal endometrium visible | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
Endometrial cancer forms when there are errors in normal endometrial cell growth. Usually, when cells grow old or get damaged, they die, and new cells take their place. Cancer starts when new cells form unneeded, and old or damaged cells do not die as they should. The buildup of extra cells often forms a mass of tissue called a growth or tumor. These abnormal cancer cells have many genetic abnormalities that cause them to grow excessively.
In 10–20% of endometrial cancers, mostly Grade 3 (the highest histologic grade), mutations are found in a tumor suppressor gene, commonly p53 or PTEN. In 20% of endometrial hyperplasias and 50% of endometrioid cancers, PTEN suffers a loss-of-function mutation or a null mutation, making it less effective or completely ineffective. Loss of PTEN function leads to up-regulation of the PI3k/Akt/mTOR pathway, which causes cell growth. The p53 pathway can either be suppressed or highly activated in endometrial cancer. When a mutant version of p53 is overexpressed, the cancer tends to be particularly aggressive. P53 mutations and chromosome instability are associated with serous carcinomas, which tend to resemble ovarian and Fallopian carcinomas. Serous carcinomas are thought to develop from endometrial intraepithelial carcinoma.
PTEN and p27 loss of function mutations are associated with a good prognosis, particularly in obese women. The Her2/neu oncogene, which indicates a poor prognosis, is expressed in 20% of endometrioid and serous carcinomas. CTNNB1 (beta-catenin; a transcription gene) mutations are found in 14–44% of endometrial cancers and may indicate a good prognosis, but the data is unclear. Beta-catenin mutations are commonly found in endometrial cancers with squamous cells. FGFR2 mutations are found in approximately 10% of endometrial cancers, and their prognostic significance is unclear. SPOP is another tumor suppressor gene found to be mutated in some cases of endometrial cancer: 9% of clear cell endometrial carcinomas and 8% of serous endometrial carcinomas have mutations in this gene.
Type I and Type II cancers (explained below) tend to have different mutations involved. ARID1A, which often carries a point mutation in Type I endometrial cancer, is also mutated in 26% of clear cell carcinomas of the endometrium, and 18% of serous carcinomas. Epigenetic silencing and point mutations of several genes are commonly found in Type I endometrial cancer. Mutations in tumor suppressor genes are common in Type II endometrial cancer. PIK3CA is commonly mutated in both Type I and Type II cancers. In women with Lynch syndrome-associated endometrial cancer, microsatellite instability is common.
Development of an endometrial hyperplasia (overgrowth of endometrial cells) is a significant risk factor because hyperplasias can and often do develop into adenocarcinoma, though cancer can develop without the presence of a hyperplasia. Within ten years, 8–30% of atypical endometrial hyperplasias develop into cancer, whereas 1–3% of non-atypical hyperplasias do so. An atypical hyperplasia is one with visible abnormalities in the nuclei. Pre-cancerous endometrial hyperplasias are also referred to as endometrial intraepithelial neoplasia. Mutations in the KRAS gene can cause endometrial hyperplasia and therefore Type I endometrial cancer. Endometrial hyperplasia typically occurs after the age of 40. Endometrial glandular dysplasia occurs with an overexpression of p53, and develops into a serous carcinoma.
Diagnosis
Diagnosis of endometrial cancer is made first by a physical examination, endometrial biopsy, or dilation and curettage (removal of endometrial tissue; D&C). This tissue is then examined histologically for characteristics of cancer. If cancer is found, medical imaging may be done to see whether the cancer has spread or invaded tissue.
Examination

Routine screening of asymptomatic people is not indicated since the disease is highly curable in its early, symptomatic stages. Instead, women, particularly menopausal women, should be aware of the symptoms and risk factors of endometrial cancer. A cervical screening test, such as a Pap smear, is not a useful diagnostic tool for endometrial cancer because the smear will be normal 50% of the time. A Pap smear can detect disease that has spread to the cervix. Results from a pelvic examination are frequently normal, especially in the early stages of disease. Changes in the size, shape or consistency of the uterus or its surrounding, supporting structures may exist when the disease is more advanced. Cervical stenosis, the narrowing of the cervical opening, is a sign of endometrial cancer when pus or blood is found collected in the uterus (pyometra or hematometra).
Women with Lynch syndrome should begin to have annual biopsy screening at the age of 35. Some women with Lynch syndrome elect to have a prophylactic hysterectomy and salpingo-oophorectomy to greatly reduce the risk of endometrial and ovarian cancer.
Transvaginal ultrasound to examine the endometrial thickness in women with postmenopausal bleeding is increasingly being used to aid in the diagnosis of endometrial cancer in the United States. In the United Kingdom, both an endometrial biopsy and a transvaginal ultrasound used in conjunction are the standard of care for diagnosing endometrial cancer. The homogeneity of the tissue visible on transvaginal ultrasound can help to indicate whether the thickness is cancerous. Ultrasound findings alone are not conclusive in cases of endometrial cancer, so another screening method (for example endometrial biopsy) must be used in conjunction. Other imaging studies are of limited use. CT scans are used for preoperative imaging of tumors that appear advanced on physical exam or have a high-risk subtype (at high risk of metastasis). They can also be used to investigate extrapelvic disease. An MRI can be of some use in determining if the cancer has spread to the cervix or if it is an endocervical adenocarcinoma. MRI is also useful for examining the nearby lymph nodes.
Dilation and curettage or an endometrial biopsy are used to obtain a tissue sample for histological examination. Endometrial biopsy is the less invasive option, but it may not give conclusive results every time. Hysteroscopy only shows the gross anatomy of the endometrium, which is often not indicative of cancer, and is therefore not used, unless in conjunction with a biopsy. Hysteroscopy can be used to confirm a diagnosis of cancer. New evidence shows that D&C has a higher false negative rate than endometrial biopsy.
Before treatment is begun, several other investigations are recommended. These include a chest x-ray, liver function tests, kidney function tests, and a test for levels of CA-125, a tumor marker that can be elevated in endometrial cancer.
Classification
Endometrial cancers may be tumors derived from epithelial cells (carcinomas), mixed epithelial and mesenchymal tumors (carcinosarcomas), or mesenchymal tumors.

Traditional classification of endometrial carcinomas is based either on clinical and endocrine features (Type I and Type II), or histopathological characteristics (endometrioid, serous, and clear-cell). Some tumors are difficult to classify and have features overlapping more than one category. High grade endometrioid tumors, in particular, tend to have both type I and type II features.
Carcinoma
The vast majority of endometrial cancers are carcinomas (usually adenocarcinomas), meaning that they originate from the single layer of epithelial cells that line the endometrium and form the endometrial glands. There are many microscopic subtypes of endometrial carcinoma, but they are broadly organized into two categories, Type I and Type II, based on clinical features and pathogenesis. The two subtypes are genetically distinct.
Type I endometrial carcinomas occur most commonly before and around the time of menopause. In the United States, they are more common in white women, particularly those with a history of endometrial hyperplasia. Type I endometrial cancers are often low-grade, minimally invasive into the underlying uterine wall (myometrium), estrogen-dependent, and have a good outcome with treatment. Type I carcinomas represent 75–90% of endometrial cancer.
Type II endometrial carcinomas usually occur in older, post-menopausal people, in the United States are more common in black women, and are not associated with increased exposure to estrogen or a history of endometrial hyperplasia. Type II endometrial cancers are often high-grade, with deep invasion into the underlying uterine wall (myometrium), are of the serous or clear cell type, and carry a poorer prognosis. They can appear to be epithelial ovarian cancer on evaluation of symptoms. They tend to present later than Type I tumors and are more aggressive, with a greater risk of relapse and/or metastasis.
Endometrioid adenocarcinoma


In endometrioid adenocarcinoma, the cancer cells grow in patterns reminiscent of normal endometrium, with many new glands formed from columnar epithelium with some abnormal nuclei. Low-grade endometrioid adenocarcinomas have well differentiated cells, have not invaded the myometrium, and are seen alongside endometrial hyperplasia. The tumor's glands form very close together, without the stromal tissue that normally separates them. Higher-grade endometrioid adenocarcinomas have less well-differentiated cells, have more solid sheets of tumor cells no longer organized into glands, and are associated with an atrophied endometrium. There are several subtypes of endometrioid adenocarcinoma with similar prognoses, including villoglandular, secretory, and ciliated cell variants. There is also a subtype characterized by squamous differentiation. Some endometrioid adenocarcinomas have foci of mucinous carcinoma.
The genetic mutations most commonly associated with endometrioid adenocarcinoma are in the genes PTEN, a tumor suppressor; PIK3CA, a kinase; KRAS, a GTPase that functions in signal transduction; and CTNNB1, involved in adhesion and cell signaling. The CTNNB1 (beta-catenin) gene is most commonly mutated in the squamous subtype of endometrioid adenocarcinoma.
Serous carcinoma
Serous carcinoma is a Type II endometrial tumor that makes up 5–10% of diagnosed endometrial cancer and is common in postmenopausal women with atrophied endometrium and black women. Serous endometrial carcinoma is aggressive and often invades the myometrium and metastasizes within the peritoneum (seen as omental caking) or the lymphatic system. Histologically, it appears with many atypical nuclei, papillary structures, and, in contrast to endometrioid adenocarcinomas, rounded cells instead of columnar cells. Roughly 30% of endometrial serous carcinomas also have psammoma bodies. Serous carcinomas spread differently than most other endometrial cancers; they can spread outside the uterus without invading the myometrium.
The genetic mutations seen in serous carcinoma are chromosomal instability and mutations in TP53, an important tumor suppressor gene.
Clear cell carcinoma
Clear cell carcinoma is a Type II endometrial tumor that makes up less than 5% of diagnosed endometrial cancer. Like serous cell carcinoma, it is usually aggressive and carries a poor prognosis. Histologically, it is characterized by the features common to all clear cells: the eponymous clear cytoplasm when H&E stained and visible, distinct cell membranes. The p53 cell signaling system is not active in endometrial clear cell carcinoma. This form of endometrial cancer is more common in postmenopausal women.
Mucinous carcinoma
Mucinous carcinomas are a rare form of endometrial cancer, making up less than 1–2% of all diagnosed endometrial cancer. Mucinous endometrial carcinomas are most often stage I and grade I, giving them a good prognosis. They typically have well-differentiated columnar cells organized into glands with the characteristic mucin in the cytoplasm. Mucinous carcinomas must be differentiated from cervical adenocarcinoma.
Mixed or undifferentiated carcinoma
Mixed carcinomas are those that have both Type I and Type II cells, with one making up at least 10% of the tumor. These include the malignant mixed Müllerian tumor, which derives from endometrial epithelium and has a poor prognosis.
Undifferentiated endometrial carcinomas make up less than 1–2% of diagnosed endometrial cancers. They have a worse prognosis than grade III tumors. Histologically, these tumors show sheets of identical epithelial cells with no identifiable pattern.
Other carcinomas
Non-metastatic squamous cell carcinoma and transitional cell carcinoma are very rare in the endometrium. Squamous cell carcinoma of the endometrium has a poor prognosis. It has been reported fewer than 100 times in the medical literature since its characterization in 1892. For primary squamous cell carcinoma of the endometrium (PSCCE) to be diagnosed, there must be no other primary cancer in the endometrium or cervix and it must not be connected to the cervical epithelium. Because of the rarity of this cancer, there are no guidelines for how it should be treated, nor any typical treatment. The common genetic causes remain uncharacterized. Primary transitional cell carcinomas of the endometrium are even more rare; 16 cases had been reported as of 2008[update]. Its pathophysiology and treatments have not been characterized. Histologically, TCCE resembles endometrioid carcinoma and is distinct from other transitional cell carcinomas.
Sarcoma

In contrast to endometrial carcinomas, the uncommon endometrial stromal sarcomas are cancers that originate in the non-glandular connective tissue of the endometrium. They are generally non-aggressive and, if they recur, can take decades. Metastases to the lungs and pelvic or peritoneal cavities are the most frequent. They typically have estrogen and/or progesterone receptors. The prognosis for low-grade endometrial stromal sarcoma is good, with 60–90% five-year survival. High-grade undifferentiated endometrial sarcoma (HGUS) has a worse prognosis, with high rates of recurrence and 25% five-year survival. HGUS prognosis is dictated by whether or not the cancer has invaded the arteries and veins. Without vascular invasion, the five-year survival is 83%; it drops to 17% when vascular invasion is observed. Stage I ESS has the best prognosis, with five-year survival of 98% and ten-year survival of 89%. ESS makes up 0.2% of uterine cancers.
Metastasis
Endometrial cancer frequently metastasizes to the ovaries and Fallopian tubes when the cancer is located in the upper part of the uterus, and the cervix when the cancer is in the lower part of the uterus. The cancer usually first spreads into the myometrium and the serosa, then into other reproductive and pelvic structures. When the lymphatic system is involved, the pelvic and para-aortic nodes are usually first to become involved, but in no specific pattern, unlike cervical cancer. More distant metastases are spread by the blood and often occur in the lungs, as well as the liver, brain, and bone. Endometrial cancer metastasizes to the lungs 20–25% of the time, more than any other gynecologic cancer.
Histopathology



There is a three-tiered system for histologically classifying endometrial cancers, ranging from cancers with well-differentiated cells (grade I), to very poorly-differentiated cells (grade III). Grade I cancers are the least aggressive and have the best prognosis, while grade III tumors are the most aggressive and likely to recur. Grade II cancers are intermediate between grades I and III in terms of cell differentiation and aggressiveness of disease.
The histopathology of endometrial cancers is highly diverse. The most common finding is a well-differentiated endometrioid adenocarcinoma, which is composed of numerous, small, crowded glands with varying degrees of nuclear atypia, mitotic activity, and stratification. This often appears on a background of endometrial hyperplasia. Frank adenocarcinoma may be distinguished from atypical hyperplasia by the finding of clear stromal invasion, or "back-to-back" glands which represent nondestructive replacement of the endometrial stroma by the cancer. With progression of the disease, the myometrium is infiltrated.
Staging
Endometrial carcinoma is surgically staged using the FIGO cancer staging system. The 2009 FIGO staging system is as follows:
| Stage | Description |
|---|---|
| IA | Tumor is confined to the uterus with less than half myometrial invasion |
| IB | Tumor is confined to the uterus with more than half myometrial invasion |
| II | Tumor involves the uterus and the cervical stroma |
| IIIA | Tumor invades serosa or adnexa |
| IIIB | Vaginal and/or parametrial involvement |
| IIIC1 | Pelvic lymph node involvement |
| IIIC2 | Para-aortic lymph node involvement, with or without pelvic node involvement |
| IVA | Tumor invades bladder mucosa and/or bowel mucosa |
| IVB | Distant metastases including abdominal metastases and/or inguinal lymph nodes |
Myometrial invasion and involvement of the pelvic and para-aortic lymph nodes are the most commonly seen patterns of spread. A Stage 0 is sometimes included, in this case it is referred to as "carcinoma in situ". In 26% of presumably early-stage cancers, intraoperative staging revealed pelvic and distant metastases, making comprehensive surgical staging necessary.

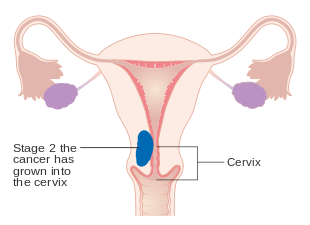
Stage IA and IB endometrial cancer
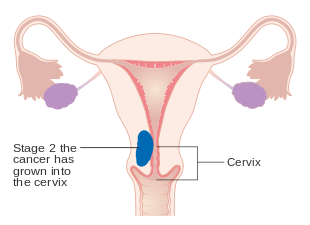
Stage II endometrial cancer