Traumatic Brain Injury
Overview
Traumatic brain injury usually results from a violent blow or jolt to the head or body. An object that goes through brain tissue, such as a bullet or shattered piece of skull, also can cause traumatic brain injury.
Mild traumatic brain injury may affect your brain cells temporarily. More-serious traumatic brain injury can result in bruising, torn tissues, bleeding and other physical damage to the brain. These injuries can result in long-term complications or death.
Symptoms
Traumatic brain injury can have wide-ranging physical and psychological effects. Some signs or symptoms may appear immediately after the traumatic event, while others may appear days or weeks later.
Mild traumatic brain injury
The signs and symptoms of mild traumatic brain injury may include:
- Physical symptoms
-
- Headache
- Nausea or vomiting
- Fatigue or drowsiness
- Problems with speech
- Dizziness or loss of balance
- Sensory symptoms
-
- Sensory problems, such as blurred vision, ringing in the ears, a bad taste in the mouth or changes in the ability to smell
- Sensitivity to light or sound
- Cognitive, behavioral or mental symptoms
-
- Loss of consciousness for a few seconds to a few minutes
- No loss of consciousness, but a state of being dazed, confused or disoriented
- Memory or concentration problems
- Mood changes or mood swings
- Feeling depressed or anxious
- Difficulty sleeping
- Sleeping more than usual
Moderate to severe traumatic brain injuries
Moderate to severe traumatic brain injuries can include any of the signs and symptoms of mild injury, as well as these symptoms that may appear within the first hours to days after a head injury:
- Physical symptoms
-
- Loss of consciousness from several minutes to hours
- Persistent headache or headache that worsens
- Repeated vomiting or nausea
- Convulsions or seizures
- Dilation of one or both pupils of the eyes
- Clear fluids draining from the nose or ears
- Inability to awaken from sleep
- Weakness or numbness in fingers and toes
- Loss of coordination
- Cognitive or mental symptoms
-
- Profound confusion
- Agitation, combativeness or other unusual behavior
- Slurred speech
- Coma and other disorders of consciousness
Children's symptoms
Infants and young children with brain injuries might not be able to communicate headaches, sensory problems, confusion and similar symptoms. In a child with traumatic brain injury, you may observe:
- Change in eating or nursing habits
- Unusual or easy irritability
- Persistent crying and inability to be consoled
- Change in ability to pay attention
- Change in sleep habits
- Seizures
- Sad or depressed mood
- Drowsiness
- Loss of interest in favorite toys or activities
When to see a doctor
Always see your doctor if you or your child has received a blow to the head or body that concerns you or causes behavioral changes. Seek emergency medical care if there are any signs or symptoms of traumatic brain injury following a recent blow or other traumatic injury to the head.
The terms "mild," "moderate" and "severe" are used to describe the effect of the injury on brain function. A mild injury to the brain is still a serious injury that requires prompt attention and an accurate diagnosis.
Causes
Traumatic brain injury is usually caused by a blow or other traumatic injury to the head or body. The degree of damage can depend on several factors, including the nature of the injury and the force of impact.
Common events causing traumatic brain injury include the following:
- Falls. Falls from bed or a ladder, down stairs, in the bath, and other falls are the most common cause of traumatic brain injury overall, particularly in older adults and young children.
- Vehicle-related collisions. Collisions involving cars, motorcycles or bicycles — and pedestrians involved in such accidents — are a common cause of traumatic brain injury.
- Violence. Gunshot wounds, domestic violence, child abuse and other assaults are common causes. Shaken baby syndrome is a traumatic brain injury in infants caused by violent shaking.
- Sports injuries. Traumatic brain injuries may be caused by injuries from a number of sports, including soccer, boxing, football, baseball, lacrosse, skateboarding, hockey, and other high-impact or extreme sports. These are particularly common in youth.
Explosive blasts and other combat injuries. Explosive blasts are a common cause of traumatic brain injury in active-duty military personnel. Although how the damage occurs isn't yet well understood, many researchers believe that the pressure wave passing through the brain significantly disrupts brain function.
Traumatic brain injury also results from penetrating wounds, severe blows to the head with shrapnel or debris, and falls or bodily collisions with objects following a blast.
Risk factors
The people most at risk of traumatic brain injury include:
- Children, especially newborns to 4-year-olds
- Young adults, especially those between ages 15 and 24
- Adults age 60 and older
- Males in any age group
Complications
Several complications can occur immediately or soon after a traumatic brain injury. Severe injuries increase the risk of a greater number of and more-severe complications.
Altered consciousness
Moderate to severe traumatic brain injury can result in prolonged or permanent changes in a person's state of consciousness, awareness or responsiveness. Different states of consciousness include:
- Coma. A person in a coma is unconscious, unaware of anything and unable to respond to any stimulus. This results from widespread damage to all parts of the brain. After a few days to a few weeks, a person may emerge from a coma or enter a vegetative state.
-
Vegetative state. Widespread damage to the brain can result in a vegetative state. Although the person is unaware of surroundings, he or she may open his or her eyes, make sounds, respond to reflexes, or move.
It's possible that a vegetative state can become permanent, but often individuals progress to a minimally conscious state.
- Minimally conscious state. A minimally conscious state is a condition of severely altered consciousness but with some signs of self-awareness or awareness of one's environment. It is sometimes a transitional state from a coma or vegetative condition to greater recovery.
- Brain death. When there is no measurable activity in the brain and the brainstem, this is called brain death. In a person who has been declared brain dead, removal of breathing devices will result in cessation of breathing and eventual heart failure. Brain death is considered irreversible.
Physical complications
- Seizures. Some people with traumatic brain injury will develop seizures. The seizures may occur only in the early stages, or years after the injury. Recurrent seizures are called post-traumatic epilepsy.
- Fluid buildup in the brain (hydrocephalus). Cerebrospinal fluid may build up in the spaces in the brain (cerebral ventricles) of some people who have had traumatic brain injuries, causing increased pressure and swelling in the brain.
- Infections. Skull fractures or penetrating wounds can tear the layers of protective tissues (meninges) that surround the brain. This can enable bacteria to enter the brain and cause infections. An infection of the meninges (meningitis) could spread to the rest of the nervous system if not treated.
- Blood vessel damage. Several small or large blood vessels in the brain may be damaged in a traumatic brain injury. This damage could lead to a stroke, blood clots or other problems.
- Headaches. Frequent headaches are very common after a traumatic brain injury. They may begin within a week after the injury and could persist for as long as several months.
- Vertigo. Many people experience vertigo, a condition characterized by dizziness, after a traumatic brain injury.
Sometimes, any or several of these symptoms might linger for a few weeks to a few months after a traumatic brain injury. When a combination of these symptoms lasts for an extended period of time, this is generally referred to as persistent post-concussive symptoms.
Traumatic brain injuries at the base of the skull can cause nerve damage to the nerves that emerge directly from the brain (cranial nerves). Cranial nerve damage may result in:
- Paralysis of facial muscles or losing sensation in the face
- Loss of or altered sense of smell or taste
- Loss of vision or double vision
- Swallowing problems
- Dizziness
- Ringing in the ear
- Hearing loss
Intellectual problems
Many people who have had a significant brain injury will experience changes in their thinking (cognitive) skills. It may be more difficult to focus and take longer to process your thoughts. Traumatic brain injury can result in problems with many skills, including:
- Cognitive problems
-
- Memory
- Learning
- Reasoning
- Judgment
- Attention or concentration
- Executive functioning problems
-
- Problem-solving
- Multitasking
- Organization
- Planning
- Decision-making
- Beginning or completing tasks
Communication problems
Language and communications problems are common following traumatic brain injuries. These problems can cause frustration, conflict and misunderstanding for people with a traumatic brain injury, as well as family members, friends and care providers.
Communication problems may include:
- Difficulty understanding speech or writing
- Difficulty speaking or writing
- Inability to organize thoughts and ideas
- Trouble following and participating in conversations
Communication problems that affect social skills may include:
- Trouble with turn taking or topic selection in conversations
- Problems with changes in tone, pitch or emphasis to express emotions, attitudes or subtle differences in meaning
- Difficulty understanding nonverbal signals
- Trouble reading cues from listeners
- Trouble starting or stopping conversations
- Inability to use the muscles needed to form words (dysarthria)
Behavioral changes
People who've experienced brain injury may experience changes in behaviors. These may include:
- Difficulty with self-control
- Lack of awareness of abilities
- Risky behavior
- Difficulty in social situations
- Verbal or physical outbursts
Emotional changes
Emotional changes may include:
- Depression
- Anxiety
- Mood swings
- Irritability
- Lack of empathy for others
- Anger
- Insomnia
Sensory problems
Problems involving senses may include:
- Persistent ringing in the ears
- Difficulty recognizing objects
- Impaired hand-eye coordination
- Blind spots or double vision
- A bitter taste, a bad smell or difficulty smelling
- Skin tingling, pain or itching
- Trouble with balance or dizziness
Degenerative brain diseases
The relationship between degenerative brain diseases and brain injuries is still unclear. But some research suggests that repeated or severe traumatic brain injuries might increase the risk of degenerative brain diseases. But this risk can't be predicted for an individual — and researchers are still investigating if, why and how traumatic brain injuries might be related to degenerative brain diseases.
A degenerative brain disorder can cause gradual loss of brain functions, including:
- Alzheimer's disease, which primarily causes the progressive loss of memory and other thinking skills
- Parkinson's disease, a progressive condition that causes movement problems, such as tremors, rigidity and slow movements
- Dementia pugilistica — most often associated with repetitive blows to the head in career boxing — which causes symptoms of dementia and movement problems
Prevention
Follow these tips to reduce the risk of brain injury:
- Seat belts and airbags. Always wear a seat belt in a motor vehicle. A small child should always sit in the back seat of a car secured in a child safety seat or booster seat that is appropriate for his or her size and weight.
- Alcohol and drug use. Don't drive under the influence of alcohol or drugs, including prescription medications that can impair the ability to drive.
- Helmets. Wear a helmet while riding a bicycle, skateboard, motorcycle, snowmobile or all-terrain vehicle. Also wear appropriate head protection when playing baseball or contact sports, skiing, skating, snowboarding or riding a horse.
- Pay attention to your surroundings. Don't drive, walk or cross the street while using your phone, tablet or any smart device. These distractions can lead to accidents or falls.
Preventing falls
The following tips can help older adults avoid falls around the house:
- Install handrails in bathrooms
- Put a nonslip mat in the bathtub or shower
- Remove area rugs
- Install handrails on both sides of staircases
- Improve lighting in the home, especially around stairs
- Keep stairs and floors clear of clutter
- Get regular vision checkups
- Get regular exercise
Preventing head injuries in children
The following tips can help children avoid head injuries:
- Install safety gates at the top of a stairway
- Keep stairs clear of clutter
- Install window guards to prevent falls
- Put a nonslip mat in the bathtub or shower
- Use playgrounds that have shock-absorbing materials on the ground
- Make sure area rugs are secure
- Don't let children play on fire escapes or balconies
Diagnosis
Traumatic brain injuries may be emergencies. In the case of more-severe traumatic brain injuries (TBIs), consequences can worsen rapidly without treatment. Doctors or first responders need to assess the situation quickly.
Glasgow Coma Scale
This 15-point test helps a doctor or other emergency medical personnel assess the initial severity of a brain injury by checking a person's ability to follow directions and move their eyes and limbs. The coherence of speech also provides important clues.
Abilities are scored from three to 15 in the Glasgow Coma Scale. Higher scores mean less severe injuries.
Information about the injury and symptoms
If you saw someone sustain an injury or arrived immediately after an injury, you may be able to provide medical personnel with information that's useful in assessing the injured person's condition.
Answers to the following questions may be beneficial in judging the severity of injury:
- How did the injury occur?
- Did the person lose consciousness?
- How long was the person unconscious?
- Did you observe any other changes in alertness, speaking, coordination or other signs of injury?
- Where was the head or other parts of the body struck?
- Can you provide any information about the force of the injury? For example, what hit the person's head, how far did he or she fall, or was the person thrown from a vehicle?
- Was the person's body whipped around or severely jarred?
Imaging tests
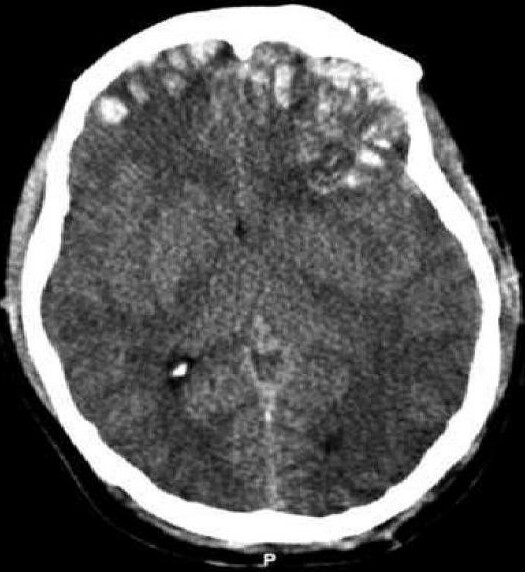
- Computerized tomography (CT) scan. This test is usually the first performed in an emergency room for a suspected traumatic brain injury. A computed tomography (CT) scan uses a series of X-rays to create a detailed view of the brain. A CT scan can quickly visualize fractures and uncover evidence of bleeding in the brain (hemorrhage), blood clots (hematomas), bruised brain tissue (contusions), and brain tissue swelling.
- Magnetic resonance imaging (MRI). An Magnetic resonance imaging (MRI) uses powerful radio waves and magnets to create a detailed view of the brain. This test may be used after the person's condition stabilizes, or if symptoms don't improve soon after the injury.
Intracranial pressure monitor
Tissue swelling from a traumatic brain injury can increase pressure inside the skull and cause additional damage to the brain. Doctors may insert a probe through the skull to monitor this pressure.
Treatment
Treatment is based on the severity of the injury.
Mild injury
Mild traumatic brain injuries usually require no treatment other than rest and over-the-counter pain relievers to treat a headache. However, a person with a mild traumatic brain injury usually needs to be monitored closely at home for any persistent, worsening or new symptoms. He or she may also have follow-up doctor appointments.
The doctor will indicate when a return to work, school or recreational activities is appropriate. Relative rest — which means limiting physical or thinking (cognitive) activities that make things worse — is usually recommended for the first few days or until your doctor advises that it's OK to resume regular activities. It isn't recommended that you rest completely from mental and physical activity. Most people return to normal routines gradually.
Immediate emergency care
Emergency care for moderate to severe traumatic brain injuries focuses on making sure the person has enough oxygen and an adequate blood supply, maintaining blood pressure, and preventing any further injury to the head or neck.
People with severe injuries may also have other injuries that need to be addressed. Additional treatments in the emergency room or intensive care unit of a hospital will focus on minimizing secondary damage due to inflammation, bleeding or reduced oxygen supply to the brain.
Medications
Medications to limit secondary damage to the brain immediately after an injury may include:
-
Anti-seizure drugs. People who've had a moderate to severe traumatic brain injury are at risk of having seizures during the first week after their injury.
An anti-seizure drug may be given during the first week to avoid any additional brain damage that might be caused by a seizure. Continued anti-seizure treatments are used only if seizures occur.
- Coma-inducing drugs. Doctors sometimes use drugs to put people into temporary comas because a comatose brain needs less oxygen to function. This is especially helpful if blood vessels, compressed by increased pressure in the brain, are unable to supply brain cells with normal amounts of nutrients and oxygen.
- Diuretics. These drugs reduce the amount of fluid in tissues and increase urine output. Diuretics, given intravenously to people with traumatic brain injury, help reduce pressure inside the brain.
Surgery
Emergency surgery may be needed to minimize additional damage to brain tissues. Surgery may be used to address the following problems:
- Removing clotted blood (hematomas). Bleeding outside or within the brain can result in a collection of clotted blood (hematoma) that puts pressure on the brain and damages brain tissue.
- Repairing skull fractures. Surgery may be needed to repair severe skull fractures or to remove pieces of skull in the brain.
- Bleeding in the brain. Head injuries that cause bleeding in the brain may need surgery to stop the bleeding.
- Opening a window in the skull. Surgery may be used to relieve pressure inside the skull by draining accumulated cerebrospinal fluid or creating a window in the skull that provides more room for swollen tissues.
Rehabilitation
Most people who have had a significant brain injury will require rehabilitation. They may need to relearn basic skills, such as walking or talking. The goal is to improve their abilities to perform daily activities.
Therapy usually begins in the hospital and continues at an inpatient rehabilitation unit, a residential treatment facility or through outpatient services. The type and duration of rehabilitation is different for everyone, depending on the severity of the brain injury and what part of the brain was injured.
Rehabilitation specialists may include:
- Physiatrist, a doctor trained in physical medicine and rehabilitation, who oversees the entire rehabilitation process, manages medical rehabilitation problems and prescribes medication as needed
- Occupational therapist, who helps the person learn, relearn or improve skills to perform everyday activities
- Physical therapist, who helps with mobility and relearning movement patterns, balance and walking
- Speech and language therapist, who helps the person improve communication skills and use assistive communication devices if necessary
- Neuropsychologist, who assesses cognitive impairment and performance, helps the person manage behaviors or learn coping strategies, and provides psychotherapy as needed for emotional and psychological well-being
- Social worker or case manager, who facilitates access to service agencies, assists with care decisions and planning, and facilitates communication among various professionals, care providers and family members
- Rehabilitation nurse, who provides ongoing rehabilitation care and services and who helps with discharge planning from the hospital or rehabilitation facility
- Traumatic brain injury nurse specialist, who helps coordinate care and educates the family about the injury and recovery process
- Recreational therapist, who assists with time management and leisure activities
- Vocational counselor, who assesses the ability to return to work and appropriate vocational opportunities and who provides resources for addressing common challenges in the workplace
Coping and support
A number of strategies can help a person with traumatic brain injury cope with complications that affect everyday activities, communication and interpersonal relationships. Depending on the severity of injury, a family caregiver or friend may need to help implement the following approaches:
- Join a support group. Talk to your doctor or rehabilitation therapist about a support group that can help you talk about issues related to your injury, learn new coping strategies and get emotional support.
- Write things down. Keep a record of important events, people's names, tasks or other things that are difficult to remember.
- Follow a routine. Keep a consistent schedule, keep things in designated places to avoid confusion and take the same routes when going to frequently visited destinations.
- Take breaks. Make arrangements at work or school to take breaks as needed.
- Alter work expectations or tasks. Appropriate changes at work or school may include having instructions read to you, allowing more time to complete tasks or breaking down tasks into smaller steps.
- Avoid distractions. Minimize distractions such as loud background noise from a television or radio.
- Stay focused. Work on one task at a time.