Ovarian Cancer

Ovarian cancer is a cancer that forms in or on an ovary. It results in abnormal cells that have the ability to invade or spread to other parts of the body. When this process begins, there may be no or only vague symptoms. Symptoms become more noticeable as the cancer progresses. These symptoms may include bloating, pelvic pain, abdominal swelling, and loss of appetite, among others. Common areas to which the cancer may spread include the lining of the abdomen, lymph nodes, lungs, and liver.
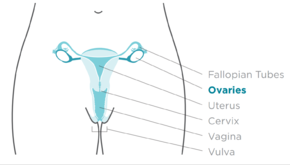
The risk of ovarian cancer increases in women who have ovulated more over their lifetime. This includes those who have never had children, those who begin ovulation at a younger age and those who reach menopause at an older age. Other risk factors include hormone therapy after menopause, fertility medication, and obesity. Factors that decrease risk include hormonal birth control, tubal ligation, and breast feeding. About 10% of cases are related to inherited genetic risk; women with mutations in the genes BRCA1 or BRCA2 have about a 50% chance of developing the disease. Ovarian carcinoma is the most common type of ovarian cancer, comprising more than 95% of cases. There are five main subtypes of ovarian carcinoma, of which high-grade serous carcinoma (HGSC) is the most common. These ovarian tumors are believed to start in the cells covering the ovaries, though some may form at the Fallopian tubes. Less common types of ovarian cancer include germ cell tumorsand sex cord stromal tumors. A diagnosis of ovarian cancer is confirmed through a biopsy of tissue, usually removed during surgery.
Screening is not recommended in women who are at average risk, as evidence does not support a reduction in death and the high rate of false positive tests may lead to unneeded surgery, which is accompanied by its own risks. Those at very high risk may have their ovaries removed as a preventive measure. If caught and treated in an early stage, ovarian cancer is often curable. Treatment usually includes some combination of surgery, radiation therapy, and chemotherapy. Outcomes depend on the extent of the disease, the subtype of cancer present, and other medical conditions. The overall five-year survival rate in the United States is 49%. Outcomes are worse in the developing world.
In 2012, new cases occurred in approximately 239,000 women. In 2015 it was present in 1.2 million women and resulted in 161,100 deaths worldwide. Among women it is the seventh-most common cancer and the eighth-most common cause of death from cancer. The typical age of diagnosis is 63. Death from ovarian cancer is more common in North America and Europe than in Africa and Asia.
Signs and symptoms
Early symptoms
Early signs and symptoms of ovarian cancer may be absent or subtle. In most cases, symptoms exist for several months before being recognized and diagnosed. Symptoms can be misdiagnosed as irritable bowel syndrome. The early stages of ovarian cancer tend to be painless. Symptoms can vary based on the subtype. Ovarian borderline tumors, also known as low malignant potential (LMP) ovarian tumors, do not cause an increase in CA125 levels and are not identifiable with an ultrasound. The typical symptoms of an LMP tumor can include abdominal distension or pelvic pain. Particularly large masses tend to be benign or borderline.
The most typical symptoms of ovarian cancer include bloating, abdominal or pelvic pain or discomfort, back pain, irregular menstruation or postmenopausal vaginal bleeding, pain or bleeding after or during sexual intercourse, loss of appetite, fatigue, diarrhea, indigestion, heartburn, constipation, nausea, feeling full, and possibly urinary symptoms (including frequent urination and urgent urination).
Later symptoms
The growing mass may cause pain if ovarian torsion develops. Symptoms can be caused by a mass pressing on the other abdominopelvic organs or from metastases. If these symptoms start to occur more often or more severely than usual, especially after no significant history of such symptoms, ovarian cancer is considered. Metastases may cause a Sister Mary Joseph nodule. Rarely, teratomas can cause growing teratoma syndrome or peritoneal gliomatosis. Some experience menometrorrhagia and abnormal vaginal bleeding after menopause in most cases. Other common symptoms include hirsutism, abdominal pain, virilization, and an adnexal mass.
Children
In adolescents or children with ovarian tumors, symptoms can include severe abdominal pain, irritation of the peritoneum, or bleeding. Symptoms of sex cord-stromal tumors produce hormones that can affect the development of secondary sex characteristics. Sex cord-stromal tumors in prepubertal children may be manifested by early puberty; abdominal pain and distension are also common. Adolescents with sex cord-stromal tumors may experience amenorrhea. As the cancer becomes more advanced, it can cause an accumulation of fluid in the abdomen. If the malignancy has not been diagnosed by the time it causes ascites, it is typically diagnosed shortly thereafter. Advanced cancers can also cause abdominal masses, lymph node masses, or pleural effusion.
Risk factors
Ovarian cancer is related to the amount of time spent ovulating. Thus not having children is a risk factor for ovarian cancer, likely because ovulation is suppressed via pregnancy. During ovulation, cells are constantly stimulated to divide while ovulatory cycles continue. Therefore, people who have not borne children are at twice the risk of ovarian cancer than those who have. A longer period of ovulation caused by early first menstruation and late menopause is also a risk factor. Both obesity and hormone replacement therapy also raise the risk.
The risk of developing ovarian cancer is less for women who have fewer menstrual cycles, no menstrual cycles, breast feeding, take oral contraceptives, have multiple pregnancies, and have a pregnancy at an early age. The risk of developing ovarian cancer is reduced in women who have had tubal ligation (colloquially known as having one's "tubes tied"), both ovaries removed, or hysterectomy (an operation in which the uterus, and sometimes the cervix, is removed). Age is also a risk factor.
Hormones
Use of fertility medication may contribute to ovarian borderline tumor formation, but the link between the two is disputed and difficult to study. Fertility drugs may be associated with a higher risk of borderline tumors. Those who have been treated for infertility but remain nulliparous are at higher risk for epithelial ovarian cancer; however, those who are successfully treated for infertility and subsequently give birth are at no higher risk. This may be due to shedding of precancerous cells during pregnancy but the cause remains unclear. The risk factor may instead be infertility itself, not the treatment.
Hormonal conditions such as polycystic ovary syndrome and endometriosis are associated with ovarian cancer, but the link is not completely confirmed. Postmenopausal hormone replacement therapy (HRT) with estrogen likely increases the risk of ovarian cancer. The association has not been confirmed in a large-scale study, but notable studies including the Million Women Study have supported this link. Postmenopausal HRT with combined estrogen and progesterone may increase contemporaneous risk if used for over 5 years, but this risk returns to normal after cessation of therapy. Estrogen HRT with or without progestins increases the risk of endometrioid and serous tumors but lowers the risk of mucinous tumors. Higher doses of estrogen increase this risk. Endometriosis is another risk factor for ovarian cancer, as is pain with menstruation. Endometriosis is associated with clear-cell and endometrioid subtypes, low-grade serous tumors, stage I and II tumors, grade 1 tumors, and lower mortality.
Before menopause, obesity can increase a person's risk of ovarian cancer, but this risk is not present after menopause. This risk is also relevant in those who are both obese and have never used HRT. A similar association with ovarian cancer appears in taller people.
Genetics
 3/31/PedigreechartC.png/290px-PedigreechartC.png" decoding="async" width="290" height="215" class="thumbimage" srcset="//upload.wikimedia.org/wikipedia/en/thumb/3/31/PedigreechartC.png/435px-PedigreechartC.png 1.5x, //upload.wikimedia.org/wikipedia/en/thumb/3/31/PedigreechartC.png/580px-PedigreechartC.png 2x" data-file-width="700" data-file-height="518">
3/31/PedigreechartC.png/290px-PedigreechartC.png" decoding="async" width="290" height="215" class="thumbimage" srcset="//upload.wikimedia.org/wikipedia/en/thumb/3/31/PedigreechartC.png/435px-PedigreechartC.png 1.5x, //upload.wikimedia.org/wikipedia/en/thumb/3/31/PedigreechartC.png/580px-PedigreechartC.png 2x" data-file-width="700" data-file-height="518"> A family history of ovarian cancer is a risk factor for ovarian cancer. People with hereditary nonpolyposis colon cancer (Lynch syndrome), and those with BRCA-1 and BRCA-2 genetic abnormalities are at increased risk.
The major genetic risk factor for ovarian cancer is a mutation in BRCA1 or BRCA2 genes, or in DNA mismatch repair genes, which is present in 10% of ovarian cancer cases. Only one allele need be mutated to place a person at high risk. The gene can be inherited through either the maternal or paternal line, but has variable penetrance. Though mutations in these genes are usually associated with increased risk of breast cancer, they also carry a substantial lifetime risk of ovarian cancer, a risk that peaks in a person's 40s and 50s. The lowest risk cited is 30% and the highest 60%. Mutations in BRCA1 have a lifetime risk of developing ovarian cancer of 15–45%. Mutations in BRCA2 are less risky than those with BRCA1, with a lifetime risk of 10% (lowest risk cited) to 40% (highest risk cited). On average, BRCA-associated cancers develop 15 years before their sporadic counterparts because people who inherit the mutations on one copy of their gene only need one mutation to start the process of carcinogenesis, whereas people with two normal genes would need to acquire two mutations.
In the United States, five of 100 women with a first-degree relative with ovarian cancer will eventually get ovarian cancer themselves, placing those with affected family members at triple the risk of women with unaffected family members. Seven of 100 women with two or more relatives with ovarian cancer will eventually get ovarian cancer. In general, 5–10% of ovarian cancer cases have a genetic cause. BRCA mutations are associated with high-grade serous nonmucinous epithelial ovarian cancer.
A strong family history of endometrial cancer, colon cancer, or other gastrointestinal cancers may indicate the presence of a syndrome known as hereditary nonpolyposis colorectal cancer (also known as Lynch syndrome), which confers a higher risk for developing a number of cancers, including ovarian cancer. Lynch syndrome is caused by mutations in mismatch repair genes, including MSH2, MLH1, MLH6, PMS1, and PMS2. The risk of ovarian cancer for an individual with Lynch syndrome is between 10 and 12 percent. People of Icelandic descent, European Jewish descent/Ashkenazi Jewish descent, and Hungarian descent are at higher risk for epithelial ovarian cancer. Estrogen receptor beta gene (ESR2) seems to be a key to pathogenesis and response to therapy. Other genes that have been associated with ovarian cancer are BRIP1, MSH6, RAD51C and RAD51D. CDH1, CHEK2, PALB2 and RAD50 have also been associated with ovarian cancer.
Several rare genetic disorders are associated with specific subtypes of ovarian cancer. Peutz–Jeghers syndrome, a rare genetic disorder, also predisposes people to sex cord tumour with annular tubules. Ollier disease and Maffucci syndrome are associated with granulosa cell tumors in children and may also be associated with Sertoli-Leydig tumors. Benign fibromas are associated with nevoid basal cell carcinoma syndrome.
Environmental factors
Industrialized nations, with the exception of Japan, have high rates of epithelial ovarian cancer, which may be due to diet in those countries. Caucasian are at a 30–40% higher risk for ovarian cancer when compared to Black and Hispanic people, likely due to socioeconomic factors; white women tend to have fewer children and different rates of gynecologic surgeries that affect risk for ovarian cancer.
Cohort studies have found a correlation between dairy consumption and ovarian cancer, but case-control studies do not show this correlation. There is mixed evidence regarding the effect of red meat and processed meat in ovarian cancer.
Tentative evidence suggests that talc, pesticides, and herbicides increase the risk of ovarian cancer. The American Cancer Society notes that as of now, no study has been able to accurately link any single chemical in the environment, or in the human diet, directly to mutations that cause ovarian cancer.
Other
Alcohol consumption does not appear to be related to ovarian cancer. Other factors that have been investigated, such as smoking, low levels of vitamin D in the blood, presence of inclusion ovarian cysts, and infection with human papilloma virus (the cause of some cases of cervical cancer), have been disproven as risk factors for ovarian cancer. The carcinogenicity of perineal talc is controversial, because it can act as an irritant if it travels through the reproductive tract to the ovaries. Case-control studies have shown that use of perineal talc does increase the risk of ovarian cancer, but using talc more often does not create a greater risk. Use of talc elsewhere on the body is unrelated to ovarian cancer. Sitting regularly for prolonged periods is associated with higher mortality from epithelial ovarian cancer. The risk is not negated by regular exercise, though it is lowered.
Increased age (up to the 70s) is a risk factor for epithelial ovarian cancer because more mutations in cells can accumulate and eventually cause cancer. Those over 80 are at slightly lower risk.
Smoking tobacco is associated with a higher risk of mucinous ovarian cancer; after smoking cessation, the risk eventually returns to normal. A diet high in animal fats may be associated with ovarian cancer, but the connection is unclear. Diet seems to play a very small role, if any, in ovarian cancer risk. Higher levels of C-reactive protein are associated with a higher risk of developing ovarian cancer.
Protective factors
Suppression of ovulation, which would otherwise cause damage to the ovarian epithelium and, consequently, inflammation, is generally protective. This effect can be achieved by having children, taking combined oral contraceptives, and breast feeding, all of which are protective factors. A longer period of breastfeeding correlates with a larger decrease in the risk of ovarian cancer. Each birth decreases risk of ovarian cancer more, and this effect is seen with up to five births. Combined oral contraceptives reduce the risk of ovarian cancer by up to 50%, and the protective effect of combined oral contraceptives can last 25–30 years after they are discontinued. Regular use of aspirin or acetaminophen (paracetamol) may be associated with a lower risk of ovarian cancer; other NSAIDs do not seem to have a similar protective effect.
Tubal ligation is protective because carcinogens are unable to reach the ovary and fimbriae via the vagina, uterus, and Fallopian tubes. Tubal ligation is also protective in women with the BRCA1 mutation, but not the BRCA2 mutation. Hysterectomy reduces the risk, and removal of both Fallopian tubes and ovaries (bilateral salpingo-oophorectomy) dramatically reduces the risk of not only ovarian cancer but breast cancer as well. This is still a topic of research, as the link between hysterectomy and lower ovarian cancer risk is controversial. The reasons that hysterectomy may be protective have not been elucidated as of 2015.
A diet that includes large amounts of carotene, fiber, and vitamins with low amounts of fat—specifically, a diet with non-starchy vegetables (e.g. broccoli and onions)—may be protective, though research is still ongoing in this area. Higher caffeine intake and consumption of more than two cups of tea a day have both been associated with lower ovarian cancer risk. Smoking tobacco is protective for sex cord-stromal tumors.
Pathophysiology
| Gene mutated | Mutation type | Subtype | Prevalence |
|---|---|---|---|
| AKT1 | amplification | 3% | |
| AKT2 | amplification/mutation | 6%, 20% | |
| ARID1A | point mutation | endometrioid and clear cell | |
| BECN1 | deletion | ||
| BRAF | point mutation | low-grade serous | 0.5% |
| BRCA1 | nonsense mutation | high-grade serous | 5% |
| BRCA2 | frameshift mutation | high-grade serous | 3% |
| CCND1 | amplification | 4% | |
| CCND2 | upregulation | 15% | |
| CCNE1 | amplification | 20% | |
| CDK12 | high-grade serous | ||
| CDKN2A | downregulation (30%) and deletion (2%) | 32% | |
| CTNNB1 | clear cell | ||
| DICER1 | missense mutation (somatic) | nonepithelial | 29% |
| DYNLRB1 (km23) | mutation | 42% | |
| EGFR | amplification/overexpression | 20% | |
| ERBB2 (Her2/neu) | amplification/overexpression | mucinous and low-grade serous | 30% |
| FMS | coexpression with CSF-1 | 50% | |
| FOXL2 | point mutation (402 C to G) | adult granulosa cell | ~100% |
| JAG1 | amplification | 2% | |
| JAG2 | amplification | 3% | |
| KRAS | amplification | mucinous and low-grade serous | 11% |
| MAML1 | amplification and point mutation | 2% | |
| MAML2 | amplification and point mutation | 4% | |
| MAML3 | amplification | 2% | |
| MLH1 | 1% | ||
| NF1 | deletion (8%) and point mutation (4%) | high-grade serous | 12% |
| NOTCH3 | amplification and point mutation | 11% | |
| NRAS | low-grade serous | ||
| PIK3C3 (PI3K3) | amplification/mutation | 12–20% | |
| PIK3CA | amplification | endometrioid and clear cell | 18% |
| PPP2R1A | endometrioid and clear cell | ||
| PTEN | deletion | endometrioid and clear cell | 7% |
| RB1 | deletion (8%) and point mutation (2%) | 10% | |
| TGF-β | mutation/overexpression | 12% | |
| TP53 | mutation/overexpression | high-grade serous | 20–50% |
| TβRI | mutation | 33% | |
| TβRII | mutation | 25% | |
| USP36 | overexpression |
Ovarian cancer forms when errors in normal ovarian cell growth occur. Usually, when cells grow old or get damaged, they die, and new cells take their place. Cancer starts when new cells form unneeded, and old or damaged cells do not die as they should. The buildup of extra cells often forms a mass of tissue called an ovarian tumor or growth. These abnormal cancer cells have many genetic abnormalities that cause them to grow excessively. When an ovary releases an egg, the egg follicle bursts open and becomes the corpus luteum. This structure needs to be repaired by dividing cells in the ovary. Continuous ovulation for a long time means more repair of the ovary by dividing cells, which can acquire mutations in each division.
Overall, the most common gene mutations in ovarian cancer occur in NF1, BRCA1, BRCA2, and CDK12. Type I ovarian cancers, which tend to be less aggressive, tend to have microsatellite instability in several genes, including both oncogenes (most notably BRAF and KRAS) and tumor suppressors (most notably PTEN). The most common mutations in Type I cancers are KRAS, BRAF, ERBB2, PTEN, PIK3CA, and ARID1A. Type II cancers, the more aggressive type, have different genes mutated, including p53, BRCA1, and BRCA2. Low-grade cancers tend to have mutations in KRAS, whereas cancers of any grade that develop from low malignant potential tumors tend to have mutations in p53. Type I cancers tend to develop from precursor lesions, whereas Type II cancers can develop from a serous tubal intraepithelial carcinoma. Serous cancers that have BRCA mutations also inevitably have p53 mutations, indicating that the removal of both functional genes is important for cancer to develop.
In 50% of high-grade serous cancers, homologous recombination DNA repair is dysfunctional, as are the notch and FOXM1 signaling pathways. They also almost always have p53 mutations. Other than this, mutations in high-grade serous carcinoma are hard to characterize beyond their high degree of genomic instability. BRCA1 and BRCA2 are essential for homologous recombination DNA repair, and germline mutations in these genes are found in about 15% of people with ovarian cancer. The most common mutations in BRCA1 and BRCA2 are the frameshift mutations that originated in a small founding population of Ashkenazi Jews.
Almost 100% of rare mucinous carcinomas have mutations in KRAS and amplifications of ERBB2 (also known as Her2/neu). Overall, 20% of ovarian cancers have mutations in Her2/neu.
Serous carcinomas may develop from serous tubal intraepithelial carcinoma, rather than developing spontaneously from ovarian tissue. Other carcinomas develop from cortical inclusion cysts, which are groups of epithelial ovarian cells inside the stroma.
Diagnosis
Examination

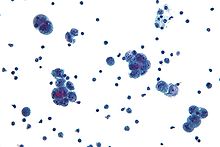
Diagnosis of ovarian cancer starts with a physical examination (including a pelvic examination), a blood test (for CA-125 and sometimes other markers), and transvaginal ultrasound. Sometimes a rectovaginal examination is used to help plan a surgery. The diagnosis must be confirmed with surgery to inspect the abdominal cavity, take biopsies (tissue samples for microscopic analysis), and look for cancer cells in the abdominal fluid. This helps to determine if an ovarian mass is benign or malignant.
Ovarian cancer's early stages (I/II) are difficult to diagnose because most symptoms are nonspecific and thus of little use in diagnosis; as a result, it is rarely diagnosed until it spreads and advances to later stages (III/IV). Additionally, symptoms of ovarian cancer may appear similar to irritable bowel syndrome. In patients in whom pregnancy is a possibility, BHCG level can be measured during the diagnosis process. Serum alpha-fetoprotein, neuron-specific enolase, and lactate dehydrogenase can be measured in young girls and adolescents with suspected ovarian tumors as younger patients are more likely to have malignant germ cell tumors.
A physical examination, including a pelvic examination, and a pelvic ultrasound (transvaginal or otherwise) are both essential for diagnosis: physical examination may reveal increased abdominal girth and/or ascites (fluid within the abdominal cavity), while pelvic examination may reveal an ovarian or abdominal mass. An adnexal mass is a significant finding that often indicates ovarian cancer, especially if it is fixed, nodular, irregular, solid, and/or bilateral. 13–21% of adnexal masses are caused by malignancy; however, there are other benign causes of adnexal masses, including ovarian follicular cyst, leiomyoma, endometriosis, ectopic pregnancy, hydrosalpinx, tuboovarian abscess, ovarian torsion, dermoid cyst, cystadenoma (serous or mucinous), diverticular or appendiceal abscess, nerve sheath tumor, pelvic kidney, ureteral or bladder diverticulum, benign cystic mesothelioma of the peritoneum, peritoneal tuberculosis, or paraovarian cyst. Ovaries that can be felt are also a sign of ovarian cancer in postmenopausal women. Other parts of a physical examination for suspected ovarian cancer can include a breast examination and a digital rectal exam. Palpation of the supraclavicular, axillary, and inguinal lymph nodes may reveal lymphadenopathy, which can be indicative of metastasis. Another indicator may be the presence of a pleural effusion, which can be noted on auscultation.
When an ovarian malignancy is included in a list of diagnostic possibilities, a limited number of laboratory tests are indicated. A complete blood count and serum electrolyte test is usually obtained; when an ovarian cancer is present, these tests often show a high number of platelets (20–25% of people) and low blood sodium levels due to chemical signals secreted by the tumor. A positive test for inhibin A and inhibin B can indicate a granulosa cell tumor.
A blood test for a marker molecule called CA-125 is useful in differential diagnosis and in follow up of the disease, but it by itself has not been shown to be an effective method to screen for early-stage ovarian cancer due to its unacceptable low sensitivity and specificity. CA-125 levels in premenopausal people over 200 U/mL may indicate ovarian cancer, as may any elevation in CA-125 above 35 U/mL in post-menopausal people. CA-125 levels are not accurate in early stage ovarian cancer, as fully half of stage I ovarian cancer patients have a normal CA-125 level. CA-125 may also be elevated in benign (non-cancerous) conditions, including endometriosis, pregnancy, uterine fibroids, menstruation, ovarian cysts, systemic lupus erythematosus, liver disease, inflammatory bowel disease, pelvic inflammatory disease, and leiomyoma. HE4 is another candidate for ovarian cancer testing, though it has not been extensively tested. Other tumor markers for ovarian cancer include CA19-9, CA72-4, CA15-3, immunosuppressive acidic protein, haptoglobin-alpha, OVX1, mesothelin, lysophosphatidic acid, osteopontin, and fibroblast growth factor 23.
Use of blood test panels may help in diagnosis. The OVA1 panel includes CA-125, beta-2 microglobulin, transferrin, apolipoprotein A1, and transthyretin. OVA1 above 5.0 in premenopausal people and 4.4 in postmenopausal people indicates a high risk for cancer. A different set of laboratory tests is used for detecting sex cord-stromal tumors. High levels of testosterone or dehydroepiandrosterone sulfate, combined with other symptoms and high levels of inhibin A and inhibin B can be indicative of an SCST of any type.
Current research is looking at ways to consider tumor marker proteomics in combination with other indicators of disease (i.e. radiology and/or symptoms) to improve diagnostic accuracy. The challenge in such an approach is that the disparate prevalence of ovarian cancer means that even testing with very high sensitivity and specificity will still lead to a number of false positive results, which in turn may lead to issues such as performing surgical procedures in which cancer is not found intraoperatively. Genomics approaches have not yet been developed for ovarian cancer.
CT scanning is preferred to assess the extent of the tumor in the abdominopelvic cavity, though magnetic resonance imaging can also be used. CT scanning can also be useful for finding omental caking or differentiating fluid from solid tumor in the abdomen, especially in low malignant potential tumors. However, it may not detect smaller tumors. Sometimes, a chest x-ray is used to detect metastases in the chest or pleural effusion. Another test for metastatic disease, though it is infrequently used, is a barium enema, which can show if the rectosigmoid colon is involved in the disease. Positron emission tomography, bone scans, and paracentesis are of limited use; in fact, paracentesis can cause metastases to form at the needle insertion site and may not provide useful results. However, paracentesis can be used in cases where there is no pelvic mass and ascites is still present. A physician suspecting ovarian cancer may also perform mammography or an endometrial biopsy (in the case of abnormal bleeding) to assess the possibility of breast malignancies and endometrial malignancy, respectively. Vaginal ultrasonography is often the first-line imaging study performed when an adnexal mass is found. Several characteristics of an adnexal mass indicate ovarian malignancy; they usually are solid, irregular, multilocular, and/or large; and they typically have papillary features, central vessels, and/or irregular internal septations. However, SCST has no definitive characteristics on radiographic study.
To definitively diagnose ovarian cancer, a surgical procedure to inspect the abdomen is required. This can be an open procedure (laparotomy, incision through the abdominal wall) or keyhole surgery (laparoscopy). During this procedure, suspicious tissue is removed and sent for microscopic analysis. Usually, this includes a unilateral salpingo-oophorectomy, removal of a single affected ovary and Fallopian tube. Fluid from the abdominal cavity can also be analyzed for cancerous cells. If cancer is found, this procedure can also be used to determine the extent of its spread (which is a form of tumor staging).
Risk scoring
A widely recognized method of estimating the risk of malignant ovarian cancer is the risk of malignancy index (RMI), calculated based on an initial workup. An RMI score of over 200 or 250 is generally felt to indicate high risk for ovarian cancer.
The RMI is calculated as:
- RMI = ultrasound score × menopausal score x CA-125 level in U/ml.
Two methods can be used to determine the ultrasound score and menopausal score, with the resultant scores being referred to as RMI 1 and RMI 2, respectively, depending on what method is used.
| Feature | RMI 1 | RMI 2 |
|---|---|---|
|
Ultrasound abnormalities:
|
|
|
| Menopausal score |
|
|
| CA-125 | Quantity in U/ml | Quantity in U/ml |
Another method for quantifying risk of ovarian cancer is the Risk of Ovarian Cancer Algorithm (ROCA), observes levels over time and determines if they are increasing rapidly enough to warrant transvaginal ultrasound. The Risk of Ovarian Malignancy algorithm uses CA-125 levels and HE4 levels to calculate the risk of ovarian cancer; it may be more effective than RMI. The IOTA models can be used to estimate the probability that an adnexal tumor is malignant. They include LR2 risk model, The Simple Rules risk (SRrisk) calculation and Assessment of Different Neoplasias in the Adnexa (ADNEX) model that can be used to assess risk of malignancy in an adnexal mass, based on its characteristics and risk factors. The QCancer (Ovary) algorithm is used to predict likelihood of ovarian cancer from risk factors.
Pathology

Ovarian cancers are classified according to the microscopic appearance of their structures (histology or histopathology). Histology dictates many aspects of clinical treatment, management, and prognosis. The gross pathology of ovarian cancers is very similar regardless of histologic type: ovarian tumors have solid and cystic masses. According to SEER, the types of ovarian cancers in women age 20 and over are:
| Percent of ovarian cancers in women age 20+ |
Percent of ovarian cancers in women age 20+ by subdivision |
Histology | Five-year RSR |
|---|---|---|---|
| 89.7 | Surface epithelial-stromal tumor (adenocarcinoma) | 54.4 | |
| 26.4 | Papillary serous cystadenocarcinoma | 21.0 | |
| 15.9 | Borderline adenocarcinoma (underestimated - short data collection interval) |
98.2 | |
| 12.6 | Adenocarcinoma, not otherwise specified | 18.3 | |
| 9.8 | Endometrioid tumor | 70.9 | |
| 5.8 | Serous cystadenocarcinoma | 44.2 | |
| 5.5 | Papillary | 21.0 | |
| 4.2 | Mucinous cystadenocarcinoma | 77.7 | |
| 4.0 | Clear-cell ovarian tumor | 61.5 | |
| 3.4 | Mucinous adenocarcinoma | 49.1 | |
| 1.3 | Cystadenocarcinoma | 50.7 | |
| 5.5 | Carcinoma | ||
| 4.1 | Carcinoma not otherwise specified | 26.8 | |
| 1.1 | Sex cord-stromal tumor | 87.8 | |
| 0.3 | Other carcinomas, specified | 37.3 | |
| 1.7 | Mullerian tumor | 29.8 | |
| 1.5 | Germ cell tumor | 91.0 | |
| 0.8 | Teratoma | 89.1 | |
| 0.5 | Dysgerminoma | 96.8 | |
| 0.3 | Other, specified | 85.1 | |
| 0.6 | Not otherwise specified | 23.0 | |
| 0.5 | Epidermoid (squamous cell carcinoma) | 51.3 | |
| 0.2 | Brenner tumor | 67.9 | |
| 0.2 | Other, specified | 71.7 |
Ovarian cancers are histologically and genetically divided into type I or type II. Type I cancers are of low histological grade and include endometrioid, mucinous, and clear-cell carcinomas. Type II cancers are of higher histological grade and include serous carcinoma and carcinosarcoma.
Epithelial carcinoma

Surface epithelial-stromal tumour, also known as ovarian epithelial carcinoma, is the most common type of ovarian cancer, representing approximately 90% of ovarian cancers. It includes serous tumor, endometrioid tumor, and mucinous cystadenocarcinoma. Less common tumors are malignant Endometrioid ovarian cancer, Clear cell ovarian cancer, and Brenner tumor (transitional cell carcinoma of the ovary). Epithelial ovarian cancers develop from the epithelium, a layer of cells that covers the ovary.
Serous carcinoma
Most people with epithelial ovarian carcinoma, about two-thirds, have a serous carcinoma, though this proportion is estimated as high as 80%. Low-grade serous carcinoma is less aggressive than high-grade serous carcinomas, though it does not typically respond well to chemotherapy or hormonal treatments. Serous carcinomas are thought to begin in the Fallopian tube. Histologically, serous adenocarcinomas have psammoma bodies. Low-grade serous adenocarcinomas resemble Fallopian tube epithelium, whereas high-grade serous adenocarcinomas show anaplasia and nuclear atypia.
50% of the time, serous carcinomas are bilateral, and in 85% of cases, they have spread beyond the ovary at the time of diagnosis. Most have a diameter over 15 cm.
Serous Tubal Intraepithelial Carcinoma (STIC) is now recognized to be the precursor lesion of most so-called ovarian high-grade serous carcinomas. STIC is characterised by
- Abnormal p53 staining
- Ki67 proliferation index in excess of 10%
- Positive WT1 (to exclude metastases)
Small-cell carcinoma
Small-cell ovarian carcinoma is rare and aggressive, with two main subtypes: hypercalcemic and pulmonary. It is typically fatal within 2 years of diagnosis. Hypercalcemic small cell ovarian carcinoma overwhelmingly affects those in their 20s, causes high blood calcium levels, and affects one ovary. Pulmonary small cell ovarian cancer usually affects both ovaries of older women and looks like oat-cell carcinoma of the lung.
Primary peritoneal carcinoma
Primary peritoneal carcinomas develop from the peritoneum, a membrane that covers the abdominal cavity that has the same embryonic origin as the ovary. They are often discussed and classified with ovarian cancers when they affect the ovary. They can develop even after the ovaries have been removed and may appear similar to mesothelioma.
Clear-cell carcinoma
Clear-cell ovarian carcinomas do not typically respond well to chemotherapy and may be related to endometriosis. They represent approximately 5% of all endometrial cancers. Japanese women develop clear-cell ovarian cancer more frequently than other groups of women.
Clear-cell adenocarcinoma

Clear-cell adenocarcinomas are histopathologically similar to other clear cell carcinomas, with clear cells and hobnail cells. They represent approximately 5–10% of epithelial ovarian cancers and are associated with endometriosis in the pelvic cavity. They are typically early-stage and therefore curable by surgery, but advanced clear-cell adenocarcinomas (approximately 20%) have a poor prognosis and are often resistant to platinum chemotherapy.
Endometrioid
Endometrioid adenocarcinomas make up approximately 15–20% of epithelial ovarian cancers. Because they are typically low-grade, endometrioid adenocarcinomas have a good prognosis. These tumors frequently co-occur with endometriosis or endometrial cancer.
29">Malignant mixed müllerian tumor (carcinosarcoma)
Mixed müllerian tumors make up less than 1% of ovarian cancer. They have epithelial and mesenchymal cells visible and tend to have a poor prognosis.
Mucinous
Mucinous tumors include mucinous adenocarcinoma and mucinous cystadenocarcinoma.
Mucinous adenocarcinoma
Mucinous adenocarcinomas make up 5–10% of epithelial ovarian cancers. Histologically, they are similar to intestinal or cervical adenocarcinomas and are often actually metastases of appendiceal or colon cancers. Advanced mucinous adenocarcinomas have a poor prognosis, generally worse than serous tumors, and are often resistant to platinum chemotherapy, though they are rare.
Pseudomyxoma peritonei
Pseudomyxoma peritonei refers to a collection of encapsulated mucous or gelatinous material in the abdominopelvic cavity, which is very rarely caused by a primary mucinous ovarian tumor. More commonly, it is associated with ovarian metastases of intestinal cancer.
Undifferentiated epithelial
Undifferentiated cancers - those where the cell type cannot be determined - make up about 10% of epithelial ovarian cancers and have a comparatively poor prognosis. When examined under the microscope, these tumors have very abnormal cells that are arranged in clumps or sheets. Usually there are recognizable clumps of serous cells inside the tumor.
Malignant Brenner tumor
Malignant Brenner tumors are rare. Histologically, they have dense fibrous stroma with areas of transitional epithelium, and some squamous differentiation. To be classified as a malignant Brenner tumor, it must have Brenner tumor foci and transitional cell carcinoma. The transitional cell carcinoma component is typically poorly differentiated and resembles urinary tract cancer.
Transitional cell carcinoma
Transitional cell carcinomas represent less than 5% of ovarian cancers. Histologically, they appear similar to bladder carcinoma. The prognosis is intermediate - better than most epithelial cancers but worse than malignant Brenner tumors.
Sex cord-stromal tumor
Sex cord-stromal tumor, including estrogen-producing granulosa cell tumor, the benign thecoma, and virilizing Sertoli-Leydig cell tumor or arrhenoblastoma, accounts for 7% of ovarian cancers. They occur most frequently in women between 50 and 69 years of age but can occur in women of any age, including young girls. They are not typically aggressive and are usually unilateral; they are therefore usually treated with surgery alone. Sex cord-stromal tumors are the main hormone-producing ovarian tumors.
Several different cells from the mesenchyme can give rise to sex-cord or stromal tumors. These include fibroblasts and endocrine cells. The symptoms of a sex-cord or stromal ovarian tumor can differ from other types of ovarian cancer. Common signs and symptoms include ovarian torsion, hemorrhage from or rupture of the tumor, an abdominal mass, and hormonal disruption. In children, isosexual precocious pseudopuberty may occur with granulosa cell tumors since they produce estrogen. These tumors cause abnormalities in menstruation (excessive bleeding, infrequent menstruation, or no menstruation) or postmenopausal bleeding. Because these tumors produce estrogen, they can cause or occur at the same time as endometrial cancer or breast cancer. Other sex-cord/stromal tumors present with distinct symptoms. Sertoli-Leydig cell tumors cause virilization and excessive hair growth due to the production of testosterone and androstenedione, which can also cause Cushing's syndrome in rare cases. Also, sex-cord stromal tumors occur that do not cause a hormonal imbalance, including benign fibromas, which cause ascites and hydrothorax. With germ cell tumors, sex cord-stromal tumors are the most common ovarian cancer diagnosed in women under 20.
Granulosa cell tumor
Granulosa cell tumors are the most common sex-cord stromal tumors, making up 70% of cases, and are divided into two histologic subtypes: adult granulosa cell tumors, which develop in women over 50, and juvenile granulosa tumors, which develop before puberty or before the age of 30. Both develop in the ovarian follicle from a population of cells that surrounds germinal cells.
Adult granulosa cell tumor
Adult granulosa cell tumors are characterized by later onset (30+ years, 50 on average). These tumors produce high levels of estrogen, which causes its characteristic symptoms: menometrorrhagia; endometrial hyperplasia; tender