Neuronal Ceroid Lipofuscinosis
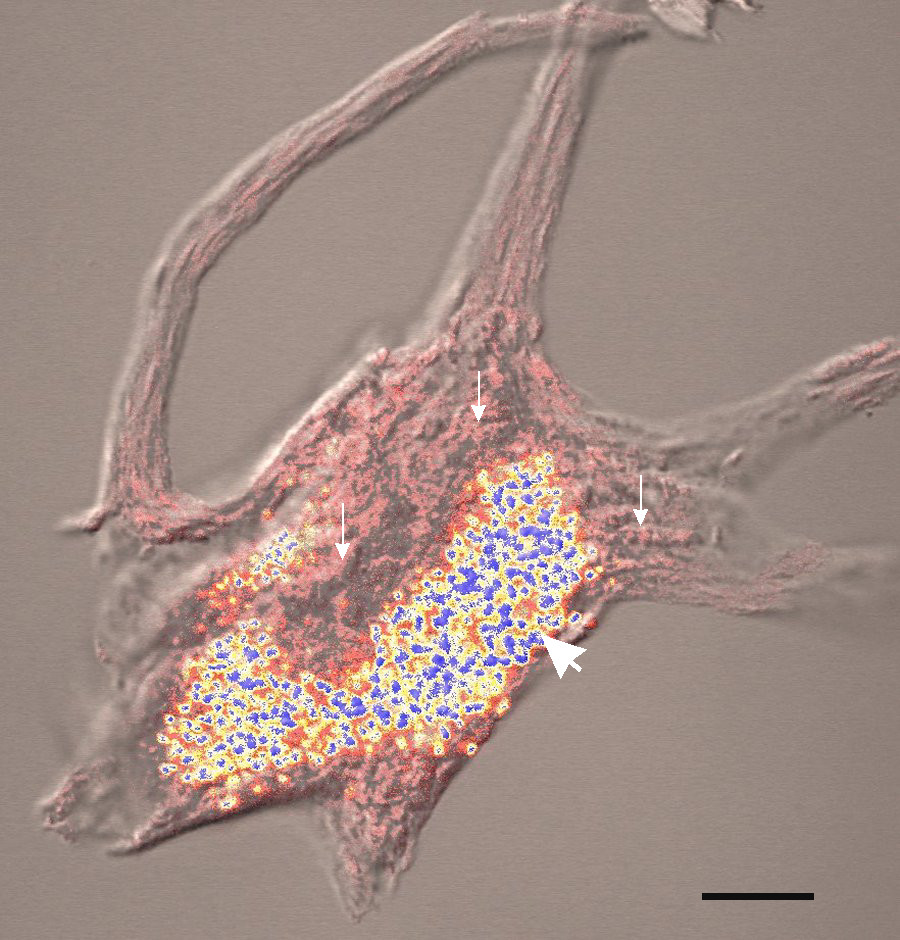
Neuronal ceroid lipofuscinoses (NCLs) are a group of inherited progressive degenerative brain diseases characterized clinically by a decline of mental and other capacities, epilepsy, and vision loss through retinal degeneration, and histopathologically by intracellular accumulation of an autofluorescent material, ceroid lipofuscin, in the neuronal cells in the brain and in the retina.
Epidemiology
The exact prevalence and incidence of this group of disorders are unknown.
Clinical description
The clinical presentation varies widely between forms but the clinical hallmark is a combination of dementia, visual loss, and epilepsy. Manifestations may begin between the neonatal period and young adult age depending on the form, leading to the original classification of NCLs by age at onset into congenital, infantile, late infantile, juvenile and adult NCL subgroups (see these terms). A Northern epilepsy variant (progressive epilepsy-intellectual deficit, Finnish type; see this term), in which the visual problems may be absent or be mild and go unrecognized, has also been described.
Etiology
To date, at least 10 genetic NCL disorders have been reported and are designated as CLN1 to CLN10. The majority of NCLs are inherited in an autosomal recessive manner, however, autosomal dominant inheritance has been reported in one adult-onset form designated as a CLN4 disease.
Diagnostic methods
Diagnosis is based on clinical findings, electron microscopy studies revealing storage material with autofluorescent ceroid lipopigments, and enzymatic testing for deficiencies in palmitoyl-protein thioesterase 1, tripeptidyl-peptidase 1 and cathepsin D, present in patients with the CLN1, CLN2 and CLN10 diseases, respectively. With the exception of the CLN4 and CLN9 diseases (for which the causative genes have not yet been identified), the diagnosis can be confirmed by molecular testing.
Differential diagnosis
The differential diagnoses should include other causes of vision loss, dementia and seizures with an appropriate age of onset (typically mitochondrial disorders, inborn errors of metabolism and other lysosomal storage disorders).
Antenatal diagnosis
Prenatal diagnosis is feasible through molecular testing if the disease-causing mutation in the family has already been identified or through enzymatic analysis in some cases.
Management and treatment
There is no curative treatment for NCLs and management is supportive only.
Prognosis
Although all NCLs lead to severe disability, the prognosis is variable with life expectancy ranging from a few hours or days after birth for the congenital form to survival into the fifth decade for patients with the adult-onset form.