Rheumatic Fever
Rheumatic fever (RF) is a multisystem inflammatory disease occurring as a post-infectious, nonsuppurative sequela of untreated streptococcus pyogenes (Group A streptococcus [GAS]) pharyngitis, and mainly occurs in individuals aged 5 to 15 years. The most common presenting signs are fever, migratory polyarthritis and carditis.
Epidemiology
The incidence of RF in industrialized countries, due to sporadic outbreaks, is typically less than 1/20, 000 individuals. In the developing world, the annual incidence is at least 100 times higher with some reports of > 1/200 individuals in select subpopulations, such as Australian Aboriginals. RF remains a major cause of acquired cardiac morbidity and mortality among people under 50 years of age.
Clinical description
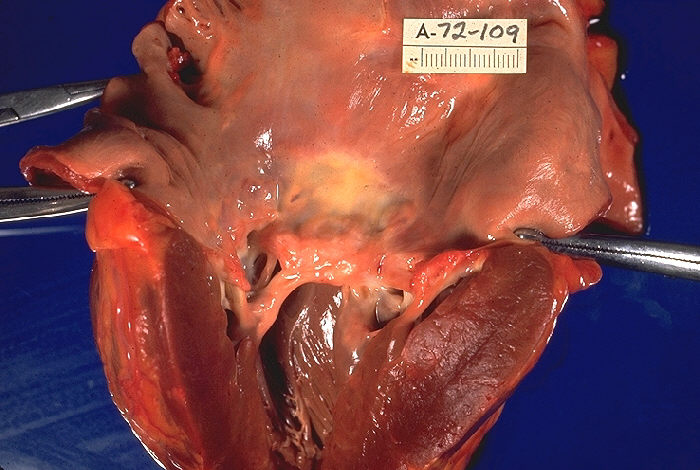
RF usually initially occurs between 5 and 15 years of age, and involves the heart, large joints and skin and is a delayed sequela of untreated GAS pharyngitis. The major diagnostic criteria include migratory polyarthritis (46-66% of cases), most commonly in the knee, ankle, elbow and wrists; carditis (53-68% clinical and additional ''subclinical'' diagnosed by echocardiogram), which is typically inflammation of the mitral (90%) or aortic valve (10%) in isolation, but any combination of all 4 valves have been reported; Sydenham chorea (8-15%); erythema marginatum (1-11%); and subcutaneous nodules on the flexor surfaces (1-8%). Minor criteria include fever (35-75% of cases), arthralgia (35-56%), first degree heart block (prolonged PR interval) (20-29%) and elevated inflammatory markers (53-91%). There is not always a prior clinically apparent GAS infection.
Etiology
There are proposed associations with certain HLA types (most frequently HLA-DR7), but numerous types have been implicated and are not always consistent among different populations. Immunological cross-reactivity is believed to occur through molecular mimicry and has been attributed to the M-protein in the GAS cell membrane. Tumor necrosis factor α and mannose-binding lectin may also be upregulated in individuals with increased RF susceptibility.
Diagnostic methods
The revised Jones criteria require the presence of two major or one major and two minor criteria, as well as evidence of a prior GAS infection. Diagnostic tests include an antistreptolysin O (ASO) titer, erythrocyte sedimentation rate (ESR) or C reactive protein (CRP), electrocardiogram to detect first degree heart block, and echocardiogram to diagnose valvulitis.
Differential diagnosis
The differential diagnosis includes other causes of febrile polyarthritis in children: juvenile idiopathic arthritis, Lyme disease, mixed connective tissue disease, reactive arthritis, sickle cell anemia, systemic lupus erythematosus (see these terms), and septic arthritis.
Management and treatment
Treatment of RF includes: 1) treatment of pharyngitis to eradicate GAS, with penicillin as first line therapy, 2) anti-inflammatory treatment, usually aspirin in the acute phase, although the use of corticosteroids is sometimes suggested, especially with severe carditis, and 3) secondary antibiotic prophylaxis to prevent recurrence of RF, usually with benzathine penicillin every 3 to 4 weeks.
Prognosis
Prognosis is generally good after initial episode of RF and all of the symptoms usually resolve completely with the exception of cardiac valve damage, which can progress over time, especially with subsequent episodes of RF, and require chronic medical management for heart failure and eventual surgical valve replacement.