Capillary Malformation-Arteriovenous Malformation 2
A number sign (#) is used with this entry because of evidence that capillary malformation-arteriovenous malformation-2 (CMAVM2) is caused by heterozygous mutation in the EPHB4 gene (600011) on chromosome 7q22.
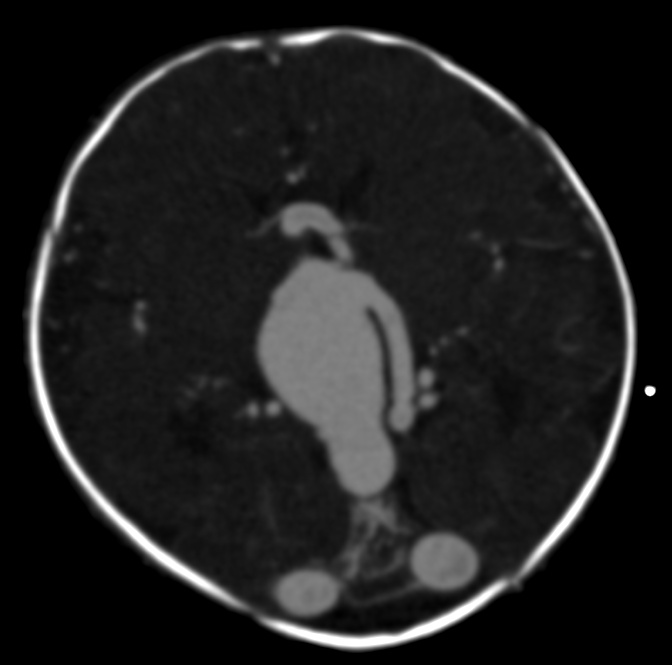
DescriptionCapillary malformation-arteriovenous malformation-2 (CMAVM2) is an autosomal dominant disorder with variable expressivity. Patients have small multifocal cutaneous capillary malformations (CMs) on the head, neck, trunk, and/or extremities, sometimes in association with arteriovenous malformations (AVMs), which are typically located in the brain, face, or extremities. Some affected individuals also exhibit Parkes Weber lesions of the extremities, and vein of Galen aneurysmal malformations (VGAMs) are present in some patients (Amyere et al., 2017).
For a discussion of genetic heterogeneity of CMAVM, see 608354.
Clinical FeaturesYu et al. (2017) reported an 8-year-old white boy who had multiple capillary malformations since infancy. Clinical examination showed round and oval vascular macules and patches, most of which had a peripheral blanched halo and were located on the head, neck, trunk, and extremities. MRI and angiography of the brain, neck, spine, chest, abdomen, and pelvis did not reveal any arteriovenous malformations or arteriovenous fistulas (AVFs).
Amyere et al. (2017) analyzed clinical data from 110 individuals with a mutation in the EPHB4 gene, including 54 CMAVM probands and 56 relatives. Penetrance was 93%, with 8 unaffected mutation carriers. Isolated multifocal CMs were observed in 34 (63%) of the families. In the remaining families, 1 or more individuals had an AVM in addition to CMs. All 102 affected individuals showed pink-to-red cutaneous CMs, usually multifocal, that were present at birth or appeared later during childhood or adolescence, and were localized on the extremities, trunk, or head and neck. Size varied from pinpoint to large lesions, up to 15 cm in diameter; the borders were usually geographic. The stains were homogeneous or telangiectatic, sometimes with a pale central zone. Bier spots were noted in 13 (12%) of the patients, and 16 (15%) had telangiectases, especially on upper thorax and lips or periorally. Only a few patients had recurrent epistaxis. Fast-flow lesions were present in 20 affected individuals (18%), and included 12 AVMs, 8 Parkes Weber lesions, and 1 AVF. There were 3 central nervous system lesions, including 2 VGAMs and 1 intraspinal AVF; 1 additional VGAM was identified in a fetus whose father carried an EPHB4 mutation, but fetal DNA was not available for analysis. The other AVMs were located in the face in 8 patients and in the extremities in 1. One patient had 2 AVMs. Four Parkes Weber lesions were found in the arms and 4 in the legs.
Vivanti et al. (2018) studied 5 families in which the proband presented with VGAM and was heterozygous for a mutation in the EPHB4 gene. Associated CMs were observed in 2 of the patients. In 4 patients, the head circumference at birth was in the 90th to 97th percentile; only 1 had cardiac failure, which was stable with medical treatment. Reduced penetrance was demonstrated in 3 families, in which carrier parents were unaffected.
MappingIn a large 5-generation family (CM-13-OH) with CMAVM, Amyere et al. (2017) performed genomewide linkage analysis and detected 2 peaks with maximum lod scores of 2.5 and 2.8, on chromosomes 5 and 7, spanning 74.2 Mb and 59.1 Mb, respectively.
Molecular GeneticsIn an 8-year-old white boy with multiple capillary malformations (CMs), who was negative for mutation in the RASA1 gene (139150), Yu et al. (2017) performed whole-exome sequencing (WES) and identified heterozygosity for a de novo missense mutation in the EPHB4 gene (D802G; 600011.0003).
From a cohort of 365 index patients with CMAVM, Amyere et al. (2017) identified heterozygosity for 47 distinct mutations in the EPHB4 gene in 54 probands (see, e.g., 600011.0004-600011.0008). The mutations were scattered all along the EPHB4 gene, and there was no genotype/phenotype correlation according to position or type of mutation; thus, the authors concluded that all of the mutations resulted in haploinsufficiency.
In a cohort of 19 probands with VGAM, negative for mutation in 5 vascular malformation-associated genes, Vivanti et al. (2018) performed WES and identified heterozygous mutations in the EPHB4 gene in 3 probands (600011.0009-600011.0011), 2 of whom also exhibited cutaneous CMs. Targeted exome sequencing or Sanger sequencing of EPHB4 in 32 additional probands with VGAM identified 2 more unrelated patients with heterozygous mutations (see, e.g., 600011.0012). In 1 of the 5 families, the mutation was shown to have arisen de novo; in 1 family, the carrier mother exhibited only CMs; and in the remaining 3 families, the carrier parent was unaffected. The authors suggested that other genes play a role in the clinical expression of the disease phenotype.