Pyridoxine-Dependent Epilepsy
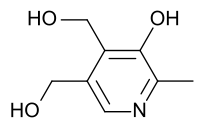
Summary
Clinical characteristics.
Pyridoxine-dependent epilepsy is characterized by intractable seizures within the first weeks to months of life that are not controlled with antiepileptic drugs but respond both clinically and electrographically to large daily supplements of pyridoxine (vitamin B6). Multiple types of clinical seizures have been reported in individuals with pyridoxine-dependent epilepsy. Dramatic presentations consisting of prolonged seizures and recurrent episodes of status epilepticus are typical; recurrent self-limited events including partial seizures, generalized seizures, atonic seizures, myoclonic events, and infantile spasms also occur. Affected individuals may have electrographic seizures without clinical correlates. Infants with the classic neonatal presentation begin to experience seizures soon after birth. Atypical features include: late-onset seizures (seizures that begin from late infancy up until age 3 years); seizures that initially respond to antiepileptic drugs and then become intractable; seizures during early life that do not respond to pyridoxine but are then controlled with pyridoxine several months later; and prolonged seizure-free intervals (≤5.5 months) that occur after discontinuation of pyridoxine. Intellectual disability is common.
Elevated concentration of α-aminoadipic semialdehyde (α-AASA) in urine and plasma is a strong biomarker of the disorder; pipecolic acid may also be elevated in plasma and cerebrospinal fluid.
Diagnosis/testing.
The diagnosis of pyridoxine-dependent epilepsy is established in a proband: (a) showing a clinical response to pyridoxine administration followed by biochemical testing showing the presence of biomarkers; and/or (b) by the identification of biallelic pathogenic variants in ALDH7A1. Clinical diagnosis may be made in individuals experiencing status epilepticus or repetitive clinical seizures that are not controlled with antiepileptic drugs by concurrently administering 100 mg of pyridoxine intravenously while monitoring the EEG, oxygen saturation, and vital signs. In individuals with pyridoxine-dependent epilepsy, clinical seizures generally cease over several minutes. If a clinical response is not demonstrated, the dose should be repeated up to a maximum of 500 mg. A corresponding change should be observed in the EEG, although it may be delayed by several hours. Alternatively, in children who experience frequent antiepileptic drug-resistant self-limited seizures, oral pyridoxine at a dose of 30 mg/kg/day may be initiated. Children who are pyridoxine dependent should have a resolution of their clinical seizures within three to seven days.
Management.
Treatment of manifestations: Pyridoxine-dependent epilepsy is initially controlled with the addition of daily supplements of pyridoxine; subsequently, in the majority of affected individuals all antiepileptic drugs can be withdrawn and seizure control continued with daily pyridoxine monotherapy in pharmacologic doses. To prevent exacerbation of clinical seizures and/or encephalopathy during an acute illness, the daily dose of pyridoxine may be doubled for several days. Special education programs are offered to affected individuals.
Prevention of secondary complications: Overuse of pyridoxine can cause a reversible sensory neuropathy.
Surveillance: Monitoring for development of clinical signs of a sensory neuropathy and regular assessments of intellectual function.
Evaluation of relatives at risk:
- If the pathogenic variants in the family are known, molecular genetic testing of at-risk newborn sibs of a proband for early diagnosis and treatment to reduce morbidity and mortality.
- If the pathogenic variants in the family are not known and the at-risk sib is experiencing clinical seizures or encephalopathy, administration of pyridoxine acutely (under EEG monitoring) for diagnostic and therapeutic purposes.
Pregnancy management: Supplemental maternal pyridoxine at a dose of 50-100 mg per day throughout the last half of pregnancy and after birth may be considered if the fetus is known to be affected or, if diagnostic prenatal testing is not pursued, in an at-risk fetus and neonate, until the diagnosis has been ruled out.
Genetic counseling.
Pyridoxine-dependent epilepsy is inherited in an autosomal recessive manner. At conception, each sib of an affected individual has a 25% chance of being affected, a 50% chance of being an asymptomatic carrier, and a 25% chance of being unaffected and not a carrier. Carrier testing for at-risk relatives, prenatal testing for a pregnancy at increased risk, and preimplantation genetic testing are possible if both pathogenic variants in a family are known.
Diagnosis
Suggestive Findings
Pyridoxine-dependent epilepsy should be suspected in individuals with the following clinical, family history, and supportive laboratory findings.
Clinical features
- Seizures in any child under age one year without an apparent brain malformation as the cause of the epilepsy
- Cryptogenic seizures in a previously normal infant without an abnormal gestational or perinatal history
- Neonates with a phenotype suggestive of hypoxic ischemic encephalopathy and with difficult-to-control seizures
- The occurrence of long-lasting focal or unilateral seizures, often with partial preservation of consciousness
- Infants and children with seizures that are partially responsive to antiepileptic drugs, in particular if associated with developmental delay and intellectual disability
- Irritability, restlessness, crying, and vomiting preceding the actual seizures
- Individuals with a history of transient or unclear response of seizures to pyridoxine
- Infants and children with a history of seizures responsive to folinic acid
Family history
- A severe convulsive disorder in a sib, often leading to death during status epilepticus
- Parental consanguinity
Supportive laboratory findings
- Elevated plasma and urinary alpha-aminoadipic semialdehyde (α-AASA)
- Elevated concentrations of pipecolic acid in plasma and cerebral spinal fluidNote: Pipecolic acid concentrations may normalize after many years of therapy [Plecko et al 2005].
- Analysis of cerebrospinal fluid monoamine metabolites via HPLC with electrochemical detection demonstrating:
- A pattern characteristic of pyridoxine-dependent epilepsy containing two peaks of unknown identity [Gallagher et al 2009];
- A characteristic chromatographic pattern of folinic acid-responsive seizures [Hyland et al 1995, Torres et al 1999, Nicolai et al 2006].
- Newborn screening. The biomarker AASA has been shown to be present in blood specimens (newborn blood spots) from neonates subsequently diagnosed with pyridoxine-dependent epilepsy [Jung et al 2013]. However, newborn screening for pyridoxine-dependent epilepsy is currently not available on a clinical basis.
Establishing the Diagnosis
The diagnosis of pyridoxine-dependent epilepsy is established in a proband showing a clinical response to pyridoxine administration, followed by biochemical testing showing the presence of biomarkers; and/or by the identification of biallelic pathogenic variants in ALDH7A1 (see Table 1).
A clinical diagnosis may be made:
- On an acute basis in individuals experiencing clinical seizures by concurrently administering 100 mg of pyridoxine intravenously while monitoring the EEG, oxygen saturation, and vital signs [Baxter 2001, Stockler et al 2011]:
- In individuals with pyridoxine-dependent epilepsy, clinical seizures generally cease over a period of several minutes.
- If a clinical response is not demonstrated, the dose should be repeated up to a maximum of 500 mg.
- A corresponding change should be observed in the EEG; in some circumstances, the change may be delayed by several hours.
- In some individuals with pyridoxine-dependent epilepsy, significant neurologic and cardiorespiratory depression follows this trial, making close systemic monitoring essential.
- By administering 30 mg/kg/day of pyridoxine orally. In individuals with pyridoxine-dependent epilepsy, clinical seizures should cease within three to five days [Baxter 2001, Gospe 2006, Stockler et al 2011].
Note: In the past, the clinical diagnosis of pyridoxine-dependent epilepsy was confirmed by withdrawing antiepileptic drugs, followed by the withdrawal of daily pyridoxine supplementation and then successfully treating a recurrence of seizures with pyridoxine. Now that measurement of biomarkers supportive of a diagnosis of pyridoxine-dependent epilepsy is clinically available, this sequence of therapeutic changes is not necessary. In an individual with a clinical phenotype suggestive of pyridoxine-dependent epilepsy, daily pyridoxine supplementation should be continued while biomarker testing is pursued.
Molecular genetic testing approaches can include single-gene testing and use of a multigene panel:
- Single-gene testing. Sequence analysis of ALDH7A1 is performed first and followed by gene-targeted deletion/duplication analysis if only one or no pathogenic variant is found.
- A multigene panel that includes ALDH7A1 and other genes of interest (see Differential Diagnosis) may also be considered. Note: (1) The genes included in the panel and the diagnostic sensitivity of the testing used for each gene vary by laboratory and are likely to change over time. (2) Some multigene panels may include genes not associated with the condition discussed in this GeneReview; thus, clinicians need to determine which multigene panel is most likely to identify the genetic cause of the condition at the most reasonable cost while limiting identification of variants of uncertain significance and pathogenic variants in genes that do not explain the underlying phenotype. (3) In some laboratories, panel options may include a custom laboratory-designed panel and/or custom phenotype-focused exome analysis that includes genes specified by the clinician. (4) Methods used in a panel may include sequence analysis, deletion/duplication analysis, and/or other non-sequencing-based tests.For an introduction to multigene panels click here. More detailed information for clinicians ordering genetic tests can be found here.
Table 1.
Molecular Genetic Testing Used in Pyridoxine-Dependent Epilepsy
| Gene 1 | Method | Proportion of Probands with Pathogenic Variants 2 Detectable by Method |
|---|---|---|
| ALDH7A1 | Sequence analysis 3 | 99/100 4 |
| Gene-targeted deletion/duplication analysis 5 | 8 individuals with exon deletions 4 | |
| Unknown 6 | NA |
- 1.
See Table A. Genes and Databases for chromosome locus and protein.
- 2.
See Molecular Genetics for information on allelic variants detected in this gene.
- 3.
Sequence analysis detects variants that are benign, likely benign, of uncertain significance, likely pathogenic, or pathogenic. Variants may include small intragenic deletions/insertions and missense, nonsense, and splice site variants; typically, exon or whole-gene deletions/duplications are not detected. For issues to consider in interpretation of sequence analysis results, click here.
- 4.
99 /100 families with individuals with both clinical and biomarker evidence of pyridoxine-dependent epilepsy had two identifiable pathogenic variants identified by sequence analysis or deletion analysis. Of these 99 kindreds, 91 affected individuals had two pathogenic variants identified by sequence analysis [Mills et al 2006, Kanno et al 2007, Plecko et al 2007, Bennett et al 2009, Mills et al 2010, Scharer et al 2010, Pérez et al 2013]. Seven additional affected individuals had one pathogenic variant identified by sequence analysis with the second variant demonstrated by deletion/deletion analysis [Kanno et al 2007, Plecko et al 2007, Mefford et al 2015]. One affected individual had biallelic large deletions [Pérez et al 2013]. The one final affected individual with confirmed pyridoxine-dependent epilepsy had one pathogenic variant identified by sequence analysis and no second variant identified by either sequence analysis or deletion/duplication analysis [Kluger et al 2008, Mefford et al 2015].
- 5.
Gene-targeted deletion/duplication analysis detects intragenic deletions or duplications. Methods used may include quantitative PCR, long-range PCR, multiplex ligation-dependent probe amplification (MLPA), and a gene-targeted microarray designed to detect single-exon deletions or duplications.
- 6.
Evidence for locus heterogeneity:
a. Assignment to the chromosome 5q31 pyridoxine-dependent epilepsy locus was excluded on the basis of haplotype analysis in one of the six North American pyridoxine-dependent epilepsy pedigrees. The affected children in the family had late-onset infantile spasms responsive to pyridoxine therapy [Bennett et al 2005]. A later study failed to detect ALDH7A1 pathogenic variants in these children and in two additional children presenting with pyridoxine-responsive late-onset infantile spasms [Bennett et al 2009].
b. Very late-onset pyridoxine-dependent epilepsy presented in a female age eight years in whom linkage to the 5q31 locus was excluded by haplotype analysis [Kabakus et al 2008].
c. Individuals with neonatal-onset pyridoxine-dependent epilepsy resulting from biallelic pathogenic variants in PROSC have been described (see Differential Diagnosis) [Darin et al 2016].
Clinical Characteristics
Clinical Description
The one clinical feature characteristic of all individuals with pyridoxine-dependent epilepsy is intractable seizures that are not controlled with antiepileptic drugs but that respond both clinically and electrographically to large daily supplements of pyridoxine.
Classic Pyridoxine-Dependent Epilepsy
Multiple types of clinical seizures have been reported in individuals with pyridoxine-dependent epilepsy. Although dramatic presentations consisting of prolonged seizures and recurrent episodes of status epilepticus are typical, recurrent self-limited events including partial, generalized, and atonic seizures; myoclonic events; and infantile spasms also occur. Affected individuals may have electrographic seizures without clinical correlates.
Newborns with the classic neonatal presentation begin to experience seizures soon after birth.
- In retrospect, many mothers recount unusual intrauterine movements that may have started in the late second trimester and that likely represent fetal seizures [Baxter 2001].
- Affected neonates frequently have periods of encephalopathy (irritability, crying, fluctuating tone, poor feeding) that precede the onset of clinical seizures. Low Apgar scores, abnormal cord blood gases, and other abnormalities of blood chemistries may also be observed. For this reason, it is not uncommon for these newborns to be diagnosed with hypoxic-ischemic encephalopathy [Baxter 1999, Mills et al 2010, van Karnebeek et al 2016].
- Clinical seizures may be associated with facial grimacing and abnormal eye movements [Schmitt et al 2010].
Similar periods of encephalopathy may be seen in older infants with pyridoxine-dependent epilepsy, particularly prior to recurrence of clinical seizures, which occur in children treated with pyridoxine whose vitamin requirement may have increased because of growth or intercurrent infection, particularly gastroenteritis.
Intellectual disability, particularly with expressive language, is common in individuals with pyridoxine-dependent epilepsy.
- It has been suggested that an earlier onset of clinical seizures corresponds to a worse prognosis for cognitive function, and the length of the delay in diagnosis and initiation of effective pyridoxine treatment correlates with increased handicaps [Baxter 2001, Kluger et al 2008, Basura et al 2009].
- Seizures in some individuals with molecularly confirmed pyridoxine-dependent epilepsy are incompletely controlled with pyridoxine, and concurrent treatment with one or more antiepileptic drugs is required. Significant intellectual disability is present in these individuals [Basura et al 2009, Scharer et al 2010].
- Some affected individuals with normal intellectual function have been reported [Ohtsuka et al 1999, Basura et al 2009, Bok et al 2012, van Karnebeek et al 2016].
- Few formal psychometric assessments in individuals with pyridoxine-dependent epilepsy have been performed. These limited studies have inconsistent findings. Two earlier studies indicate that verbal skills are more impaired than nonverbal skills [Baxter et al 1996, Baynes et al 2003] while a more recent report suggests that verbal IQ is slightly (but not significantly) higher than performance IQ [Bok et al 2012].
Atypical Pyridoxine-Dependent Epilepsy
Late-onset and other atypical features of this phenotypically heterogeneous disorder have been described [Goutières & Aicardi 1985, Coker 1992, Basura et al 2009, van Karnebeek et al 2016]. These include:
- Late-onset seizures (seizures that begin during late infancy up until age 3 years)
- Seizures that initially respond to antiepileptic drugs and then become intractable
- Seizures during early life that do not respond to pyridoxine but that are then controlled with pyridoxine several months later
- Prolonged seizure-free intervals (age ≤5.5 months) that occur after pyridoxine discontinuation
EEG/Neuroimaging
While a variety of EEG abnormalities have been described in individuals with pyridoxine-dependent epilepsy, none is pathognomonic for this condition [Mikati et al 1991, Nabbout et al 1999, Naasan et al 2009, Bok et al 2010b, Mills et al 2010, Schmitt et al 2010].
Several imaging abnormalities have been reported in individuals with pyridoxine-dependent epilepsy:
- Thinning of the corpus callosum (greatest in the isthmus and more rostral callosum) is universally seen [Friedman et al 2014, Poliachik et al 2016].
- Mega cisterna magma has been reported in a number of instances [Baxter et al 1996, Mills et al 2010, Friedman et al 2014].
Genotype-Phenotype Correlations
More than 80 ALDH7A1 sequence alterations have been documented in both neonatal-onset and late-onset cases; however, no firm genotype-phenotype correlations are known [Mills et al 2006, Kanno et al 2007, Plecko et al 2007, Rankin et al 2007, Salomons et al 2007, Bennett et al 2009, Striano et al 2009, Mills et al 2010, Scharer et al 2010, Stockler et al 2011, Bok et al 2012, Pérez et al 2013, Tlili et al 2013, van Karnebeek & Gospe 2015, Mefford et al 2015, van Karnebeek et al 2016].
The "common" p.Glu399Gln pathogenic variant in exon 14 (see Molecular Genetics, Pathogenic variants) is responsible for approximately 30% of the mutated alleles. This pathogenic missense variant has been observed in both neonatal- and late-onset cases [Bennett et al 2009].
Pathogenic missense variants that result in residual enzyme activity may be associated with a more favorable developmental phenotype [Scharer et al 2010].
Prevalence
First described by Hunt et al [1954], pyridoxine-dependent epilepsy is generally considered to be a rare cause of intractable neonatal seizures. Prior to the discovery of the biochemical and genetic abnormalities underlying pyridoxine-dependent epilepsy, approximately 100 affected individuals had been reported [Baxter 1999]. Subsequently, ALDH7A1 sequence analysis has been conducted and reported on many of these individuals along with several others.
A few epidemiologic studies of this condition have been conducted.
- In the northern part of the United Kingdom, the prevalence of pyridoxine-dependent epilepsy in children younger than age 16 years was estimated at 1:100,000 [Baxter et al 1996].
- National studies in the United Kingdom and the Republic of Ireland noted a prevalence of approximately 1:700,000 [Baxter 1999].
- A survey conducted in the Netherlands estimated a birth incidence of 1:396,000 [Been et al 2005].
- A study conducted in Germany, where pyridoxine administration is part of a standard treatment protocol for neonatal seizures, reported a birth incidence of probable cases of 1:20,000 [Ebinger et al 1999].
Differential Diagnosis
Pyridoxine-dependent epilepsy should be considered as a cause of intractable seizures presenting in neonates, infants, and children up to the third year of life for which an underlying lesion (i.e., symptomatic epilepsy) has not been identified. In particular, this diagnosis needs to be investigated in any neonate who presents with encephalopathy and seizures and in whom there is no convincing evidence of hypoxic-ischemic encephalopathy or other identifiable underlying metabolic disturbance [Baxter 1999, Stockler et al 2011].
Neonatal and Childhood Epilepsy Conditions
Other causes of intractable neonatal seizures include the following:
- "Folinic acid-responsive seizures" (see Genetically Related Disorders)
- A variety of single gene disorders that result in neonatal/infantile seizures; the products of these genes may underlie the function of ion channels, signaling pathways, and transcription factors, among others [Mastrangelo & Leuzzi 2012]. In particular, affected individuals with pathogenic variants in KCNQ2, which encodes a neuronal potassium channel, may present with a neonatal epilepsy that does respond to treatment with pyridoxine [Mefford et al 2012, Reid et al 2016].
- Epileptic encephalopathies associated with copy number variants resulting in chromosome deletions or duplications [Mefford et al 2011]
- Lissencephaly or other brain malformations that are distinguishable by the presence of structural brain malformations (see Fukuyama Congenital Muscular Dystrophy, DCX-Related Disorders, and LIS1-Associated Lissencephaly/Subcortical Band Heterotopia)
- Other rare inborn errors of metabolism that are identified by elevated ammonia, lactate, or anion gap on laboratory testing
- Severe acquired neurologic disorders such as intracerebral hemorrhage or infectious diseases (meningitis, encephalitis)
Other causes of neonatal seizures in which elevated levels of α-AASA may be present:
- Molybdenum cofactor deficiency (OMIM 252150, 252160, and 615501). This heterogeneous group of conditions can be distinguished from PDE by the presence of increased urinary xanthine, hypoxanthine, and S-sulfocysteine [Mills et al 2012, Struys et al 2012]. Molybdenum cofactor deficiency is caused by biallelic pathogenic variants in MOCS1, MOCS2, or GPHN. Inheritance is autosomal recessive.
- Isolated sulfite oxidase deficiency. This condition can be distinguished from PDE by increased urinary sulfite and decreased urinary sulfate [Mills et al 2012]. It is caused by biallelic pathogenic variants in SUOX; inheritance is autosomal recessive.
Epilepsy, early-onset, vitamin B6-dependent (OMIM 617290) is caused by biallelic pathogenic variants in PROSC (prolone synthetase co-transcribed homolog [bacterial]), which encodes a protein that is involved in the intracellular homeostatic regulation of pyridoxal 5’-phosphate (PLP), the biologically active form of pyridoxine [Darin et al 2016]. Seven individuals with this form of vitamin B6-dependent epilepsy have been reported (3 from 1 kindred) with six of the affected individuals experiencing clinical seizures on the first day of life while the first seizure in the other affected individual occurred at age one month. During intrauterine life, three of the affected individuals were reported to have abnormal intrauterine movements; four showed signs of fetal distress, including metabolic acidosis with increased blood lactate levels noted within the first few days of life. While all seven demonstrated a clinical response to pyridoxine treatment, five of the six surviving affected individuals also require the use of antiepileptic drugs. With the exception of the one person whose seizures developed at age one month, all affected individuals have acquired microcephaly. All of the six surviving affected individuals have some degree of speech, motor, and learning developmental delays.
Pyridoxine-responsive seizures. Some children with intractable seizures may have only partial improvement in seizure control with the addition of pyridoxine. In this situation, or in instances in which seizures recur after antiepileptic drugs are withdrawn and pyridoxine is continued, individuals who have not had molecular confirmation should not be diagnosed with pyridoxine-dependent epilepsy, but rather with "pyridoxine-responsive seizures" [Baxter 1999, Basura et al 2009].
Inborn pyridoxine dependency states. While other inborn pyridoxine dependency states have been described (e.g., pyridoxine-dependent anemia and pyridoxine-dependent forms of homocystinuria, xanthurenic aciduria [OMIM 236800], and cystathioninuria [OMIM 219500]), these conditions are not genetically related to pyridoxine-dependent epilepsy.
Pyridoxal phosphate-responsive epilepsy (PNPO associated) (OMIM 610090), a rare form of autosomal recessive neonatal epileptic encephalopathy, is caused by biallelic pathogenic variants in PNPO (PNPO encodes an enzyme that interconverts the phosphorylated forms of pyridoxine and pyridoxamine to the biologically active pyridoxal 5’-phosphate [PLP]). The initial reports of PNPO deficiency described infants with pharmacoresistant epileptic encephalopathy in whom the seizures responded to PLP but not to pyridoxine, suggesting that this disorder is clinically distinct from pyridoxine-dependent epilepsy [Mills et al 2005, Hoffmann et al 2007, Bagci et al 2008]. However, it was subsequently demonstrated that seizures in some individuals with PNPO deficiency actually responded to pyridoxine rather than to PLP [Pearl et al 2013, Mills et al 2014, Plecko et al 2014]. Therefore, persons with an epileptic encephalopathy responsive to pyridoxine who do not have pathogenic variants in ALDH7A1 or PROSC should have PNPO molecular genetic testing.
Other forms of pyridoxal phosphate-responsive epilepsy. Other children with intractable epilepsy who show a clinical response to pyridoxal phosphate rather than to pyridoxine have been reported [Wang et al 2005]. The biochemical basis of the epileptic condition in these children has not been established [Baxter 2005, Gospe 2006].
Management
Evaluations Following Initial Diagnosis
To establish the extent of disease and needs in an individual diagnosed with pyridoxine-dependent epilepsy, the following are appropriate:
- Developmental assessment
- Consultation with a clinical geneticist and/or genetic counselor
Treatment of Manifestations
In the majority of individuals with pyridoxine-dependent epilepsy, once seizures come under control with the addition of daily supplements of pyridoxine (see Prevention of Primary Manifestations), all antiepileptic drugs can be withdrawn, and seizure control will continue with daily pyridoxine monotherapy in pharmacologic doses.
Special education programs should be offered.
Prevention of Primary Manifestations
The effective treatment of individuals with pyridoxine-dependent epilepsy requires lifelong pharmacologic supplements of pyridoxine; the rarity of the disorder has precluded controlled studies to evaluate the optimal dose.
The recommended daily allowance (RDA) for pyridoxine is 0.5 mg for infants and 2 mg for adults. In general, individuals with pyridoxine-dependent epilepsy have excellent seizure control when treated with 50-100 mg of pyridoxine per day. Seizures in some individuals are controlled on much smaller doses and others require somewhat higher doses [Basura et al 2009, Stockler et al 2011].
Affected individuals may have exacerbations of clinical seizures and/or encephalopathy during an acute illness, such as gastroenteritis or a febrile respiratory infection. To prevent such an exacerbation in these circumstances, the daily dose of pyridoxine may be doubled for several days until the acute illness resolves.
Studies have indicated that higher doses may enhance intellectual development; it has been suggested that a dose of 15-30 mg/kg/day may be optimal [Baxter 2001, Stockler et al 2011] and that the dosage should not exceed 500 mg/day [Stockler et al 2011].
Such therapy is required for life; affected individuals are metabolically dependent on the vitamin, rather than pyridoxine deficient. Compliance with pyridoxine supplementation is critical, as status epilepticus may develop within days of pyridoxine discontinuation.
Prevention of Secondary Complications
The overuse of pyridoxine must be avoided, as a reversible sensory neuropathy (ganglionopathy) caused by pyridoxine neurotoxicity can develop. While primarily reported in adults who have received "megavitamin therapy" with pyridoxine, sensory neuropathy has been reported in two persons with pyridoxine-dependent epilepsy [McLachlan & Brown 1995, Rankin et al 2007], one of whom was an adolescent who developed a secondary cause of epilepsy and received a pyridoxine dose of 2 g/day [McLachlan & Brown 1995].
Surveillance
Affected individuals should be followed for the development of clinical signs of a sensory neuropathy, including regular assessments of joint-position sense, ankle jerks, gait, and station [Baxter 2001, Stockler et al 2011].
Regular assessments of intellectual function should be offered.
Agents/Circumstances to Avoid
Overuse of pyridoxine (see Prevention of Secondary Complications) is to be avoided.
Evaluation of Relatives at Risk
Empiric treatment of the affected individual’s newborn sib with pyridoxine supplementation should be offered until testing has been completed.
If the ALDH7A1 pathogenic variants in the family are known, molecular genetic testing is appropriate.
If the pathogenic variants are not known, the following is recommended:
- If a younger sib of a proband presents with encephalopathy or a seizure, pyridoxine should be administered acutely (ideally under EEG monitoring) for both diagnostic and therapeutic purposes.
- α-AASA is a sensitive biomarker for pyridoxine-dependent epilepsy while pipecolic acid is an indirect and less sensitive biomarker. If elevated plasma biomarker concentrations have been demonstrated in the proband, a similar elevation in a younger sib would support a diagnosis of pyridoxine-dependent epilepsy.
Note: It would be unlikely for the proband's older sibs who have not experienced seizures to be pyridoxine dependent.
See Genetic Counseling for issues related to testing of at-risk relatives for genetic counseling purposes.
Pregnancy Management
As recurrence risk for couples who have a child with this disorder is 25%, there is justification to treat the mother empirically with supplemental pyridoxine at a dose of 50-100 mg/day throughout the last half of her subsequent pregnancies and to treat the newborn with supplemental pyridoxine to prevent seizures and reduce the risk of neurodevelopmental disability [Baxter & Aicardi 1999, Bok et al 2010a]. It is important to emphasize, however, that at least one severe phenotype has been described in a family in which prenatal treatment of an at-risk sib did not result in an improved neurodevelopmental outcome [Rankin et al 2007].
Molecular genetic testing of ALDH7A1 can be performed prenatally or after birth; if both pathogenic variants are present, pyridoxine treatment should be continued during pregnancy (if prenatal testing is pursued and reveals the fetus to be affected) and after birth; if not, treatment can be withdrawn.
Therapies Under Investigation
As ALDH7A1 encodes the enzyme α-aminoadipic semialdehyde dehydrogenase (antiquitin), which is involved in cerebral lysine catabolism, it has been proposed that persons with pyridoxine-dependent epilepsy may benefit from a lysine-restricted diet. A small number of individuals have been treated in this fashion; improvements in development and behavior along with decreased biomarker levels have been described [Stockler et al 2011, van Karnebeek et al 2012]. A protocol for controlled therapeutic trials of lysine restriction in pyridoxine-dependent epilepsy has recently been proposed [van Karnebeek et al 2014].
L-arginine competitively inhibits lysine transport and can therefore reduce lysine levels. Some individuals with pyridoxine-dependent epilepsy have difficulty tolerating a lysine-restricted medical diet; in such cases L-arginine supplementation has been offered as an alternative method of lowering lysine levels [Mercimek-Mahmutoglu et al 2014]. The effectiveness of treating pyridoxine-dependent epilepsy with "triple therapy" (a combination of pyridoxine supplementation, lysine restriction, and L-arginine supplementation) has also been studied [Coughlin et al 2015, Mahajnah et al 2016], with promising results in a small number of treated individuals.
A cellular proof of concept for antisense therapy of pyridoxine-dependent epilepsy has been reported [Pérez et al 2013]. Specifically, the silent nucleotide change c.75C>T, a novel splicing variant creating a new donor splice site in exon 1, was rescued in a lymphoblast cell line via antisense therapy.
Search ClinicalTrials.gov in the US and EU Clinical Trials Register in Europe for access to information on clinical studies for a wide range of diseases and conditions.