Mitochondrial Myopathy, Encephalopathy, Lactic Acidosis, And Stroke-Like Episodes
A number sign (#) is used with this entry because MELAS syndrome can be caused by mutation in several genes, including MTTL1 (590050), MTTQ (590030), MTTH (590040), MTTK (590060), MTTC (590020), MTTS1 (590080), MTND1 (516000), MTND5 (516005), MTND6 (516006), and MTTS2 (590085). The most common mutation causing MELAS is a c.3243A-G transition in the MTTL1 gene (590050.0001) (summary by Malfatti et al., 2013).
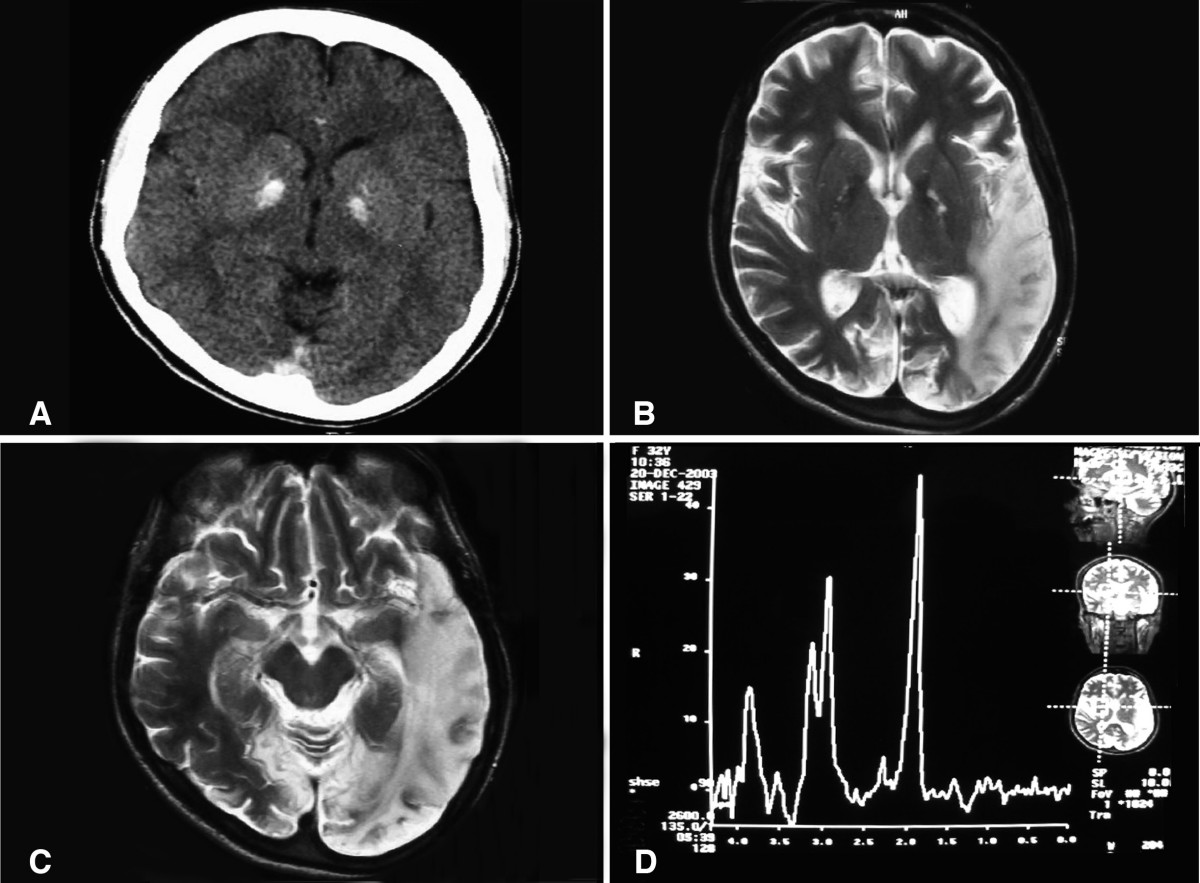
DescriptionMELAS syndrome, comprising mitochondrial myopathy, encephalopathy, lactic acidosis, and stroke-like episodes, is a genetically heterogeneous mitochondrial disorder with a variable clinical phenotype. The disorder is accompanied by features of central nervous system involvement, including seizures, hemiparesis, hemianopsia, cortical blindness, and episodic vomiting (Pavlakis et al., 1984; Montagna et al., 1988).
Other mitochondrial encephalomyopathies include Leigh syndrome (LS; 256000), Kearns-Sayre syndrome (KSS; 530000), MERRF syndrome (545000), and Leber optic atrophy (535000).
Clinical FeaturesGoto et al. (1992) studied MELAS in 21 males and 19 females to characterize the clinical features and biochemical and muscle biopsy findings related to the 3243A-G transition in the MTTL1 gene (590050.0001). The most frequent symptom was episodic sudden headache with vomiting and convulsions, which in 80% of cases affected patients aged 5 to 15 years. They demonstrated the mtDNA mutation in 32 of the 40 patients but concluded that there were no clinical or pathologic differences between the patients with or without the mutation.
Latkany et al. (1999) reported the ocular findings in 4 family members with MELAS syndrome caused by the 3243A-G MTTL1 mutation (590050.0001). Findings included ophthalmoplegia, neurosensory deafness, reduced photopic and scotopic electroretinogram b-wave amplitudes, myopathy, and macular retinal pigment epithelial atrophy.
De Quick et al. (1991) described MELAS syndrome in 2 sisters in whom detailed workup, including muscle biopsy, was normal in the mother but in the father showed a myopathic pattern on EMG and ragged-red fibers on muscle biopsy. Whether coincidence or true transmission from the father was not clear.
In a sporadic case of MELAS syndrome, Ravn et al. (2001) identified a heteroplasmic mutation in the ND6 gene (14453G-A; 516006.0005). The patient was a 7-year-old girl with normal development until the age of 2 years. Between 2 and 3 years of age, she had episodes of vomiting followed by ketotic acidosis. She developed myoclonic epilepsy, general weakness, and ataxia with intermittent dystonia. Magnetic resonance scans showed cerebellar hypoplasia and multiple infarctions in both hemispheres. A muscle biopsy revealed lipid storage myopathy with normal mitochondria on electron microscopy. The patient developed episodes of lethargy, lactic acidosis, and alternating uniparesis. Ophthalmologic examination revealed no sign of atrophy of the optic nerve but abolished visual evoked potentials (VEP). The mother was healthy, with no history of a mitochondrial disorder. Mitochondrial enzyme analysis in the patient showed a decreased activity of complex I in muscle. Sequencing of the entire mtDNA, except part of the D loop, revealed heteroplasmy for the 14453G-A mutation in 82% of the mtDNA of the patient's muscle and 78% in blood. The mutation was not detected in the blood of the mother nor in 50 healthy controls. In addition to the 14453G-A mutation, Ravn et al. (2001) identified 2 other homoplasmic mutations in the mtDNA of their patient, 5628T-C in the MTTA gene (590000) and 13535A-G in the MTND5 gene (516005), which might have contributed to the observed decrease in activity of complex I and the severe phenotype of the patient.
Bataillard et al. (2001) reported an atypical case of MELAS syndrome associated with a 4332G-A mutation in the MTTQ gene (590030.0003). The patient was a 47-year-old male with sensorineural deafness since age 20 years, who presented with an acute stroke in the absence of cardiovascular disease. Although late onset and some neuroradiographic findings were atypical for MELAS, there were extensive basal ganglia calcifications and muscle COX activity was decreased with severely deficient fibers. The 4332G-A mutation was present in 81% of the patient's muscle mtDNA molecules, and absent from his mtDNA blood and skin cells. The mutation was not found in mtDNA blood cells from his mother and brother or in 300 controls. The authors emphasized the genetic heterogeneity of the MELAS syndrome.
In several affected members of 3-generation Sardinian kindred with a maternally inherited syndrome characterized by features of both MERRF and MELAS, Zeviani et al. (1993) identified a mutation in the MTTK gene (590060.0002). The relative amount of mutant mtDNA in muscle correlated with the severity of the clinical presentation. Clinical features included myoclonic epilepsy, neural deafness, ataxia, and stroke-like episodes.
In a mother and daughter with MERRF/MELAS overlap syndrome, Nakamura et al. (1995) identified a heteroplasmic mutation in the MTTS1 gene (590080.0001). The proband in their study was a mentally retarded 26-year-old woman who had had epileptic attacks since the age of 15 years. At the age of 20 years, clear symptoms of MERRF syndrome developed, including myoclonic seizures, generalized tonic-clonic seizures, and paroxysmal hearing disturbance. She also showed mental deterioration, muscle atrophy weakness, and truncal ataxia. Lactate levels in both blood and cerebrospinal fluid were elevated. The brain CT scan showed cerebral atrophy and bilateral calcification of the basal ganglia. Muscle biopsies showed many ragged-red fibers and abnormal mitochondria with concentric cristae. The mother was a 55-year-old woman who had myoclonic jerks of the arms and generalized seizures since the age of 37 years. At age 47 years, she was moderately demented. Muscle weakness and ataxia were not apparent. The brain CT scan revealed calcification of the basal ganglia and bilateral occipital lobe atrophy. At age 55 years, she developed blindness after an episode of generalized seizure, and thereafter was bedridden and severely demented; the phenotype suggested stroke-like episodes consistent with MELAS syndrome.
Melone et al. (2004) reported a 20-year-old man who experienced sudden migrainous headache and vomiting, followed by left hemiparesis and lateral homonymous hemianopia. Seizures also occurred. The clinical picture was consistent with MELAS syndrome. At age 25 years, he developed myoclonus and ataxia, suggesting MERRF syndrome. His mother had shown similar stroke-like episodes and had died at age 36 years. Muscle biopsy of the proband showed abnormal mitochondrial proliferation and COX-negative fibers. Genetic analysis identified a heteroplasmic mutation in the MTTH gene (590040.0003).
Kirby et al. (2004) reported 3 unrelated patients with MELAS syndrome in whom the common 3243A-G mutation of the MTTL1 gene (590050.0001) could not be detected, but who expressed a specific deficiency of complex I activity in both skeletal muscle and cultured fibroblasts. Targeted sequencing of the mitochondrial tRNA and MTND genes showed that each patient harbored a different mutation in the MTND1 subunit gene of complex I (590050.0012-590050.0014, respectively).
Kisanuki et al. (2006) identified the common 3243A-G mutation in a 50-year-old man with onset of headaches and seizures associated with bitemporal lesions identified on brain MRI. Other clinical features included long-standing thin habitus, deafness, and diabetes. The authors noted the late onset of classic MELAS symptoms in this patient and suggested a low mitochondrial mutation load in the brain.
Kaufmann et al. (2006) found that 23 (77%) of 30 MELAS patients ranging in age from 10 to 60 years had abnormal peripheral nerve conduction measures. All patients had the common MTTL1 3243A-G mutation (590050.0001). Although only 15 (50%) had outright clinical symptoms of peripheral neuropathy such as imbalance, paresthesias, and numbness, almost all (29 of 30) had abnormal findings on neurologic exam, including reflex testing, sensory exam, distal muscle strength testing, and gait. Nerve conduction tests showed pure sensory anomalies in 10 patients, pure motor anomalies in 5, and a mixed pattern in 8. Twelve patients had axonal neuropathy, 4 demyelinating, and 7 mixed. Lower extremities were more commonly affected (19 of 23) than upper extremities. Twelve patients with abnormal conduction studies had either abnormal fasting glucose levels or increased thyrotropin levels. Kaufmann et al. (2006) concluded that peripheral nerve abnormalities in patients with MELAS are common and likely reflect the high energy demand of the nervous system.
In a questionnaire-based survey, Parsons et al. (2010) found that 28 (80%) of 35 patients with MELAS due to the 3243A-G mutation (590050.0001) and 33 (62%) of 53 carrier relatives reported autonomic symptoms compared to 2 (12%) of 16 controls. Gastrointestinal symptoms, orthostatic dizziness, and cold or discolored hands and feet were the most common complaints among mutation carriers.
Testai and Gorelick (2010) reviewed the pathophysiology of stroke in patients with MELAS. Although the etiology is not completely explained, there is likely a role for mitochondrial angiopathy, vascular dysfunction, and hyperemia, as well as mitochondrial-mediated cytopathic mechanisms, which may result in energy failure. Neuronal hyperexcitability may also play a role.
In a retrospective study, Malfatti et al. (2013) found that 38 of 41 individuals with the MTTL1 c.3243A-G mutation had symptoms consistent with MELAS, whereas 3 were asymptomatic. The symptomatic patients had onset between 24 and 40 years of variable features, including sensorineural deafness, myopathy, cognitive impairment, neuropathy, ophthalmoplegia, diabetes, and stroke-like episodes. Cardiac investigations identified left ventricular hypertrophy and/or left ventricular dysfunction in 18 patients, along with Wolff-Parkinson-White syndrome in 7, conduction system disease in 4, and atrial fibrillation in 1. Over a median 5-year follow-up period, 11 patients died, including 3 due to heart failure. Seven patients had life-threatening adverse events, including 6 hospitalizations for severe heart failure and 1 resuscitated cardiac arrest. One patient had a heart transplant. Malfatti et al. (2013) concluded that, after central neurologic disease, cardiac disease has the greatest impact on prognosis in patients with the c.3243A-G mutation. Left ventricular hypertrophy was the only independent prognostic risk factor for adverse cardiac events, suggesting that these patients should be closely monitored. The severity of cardiac disease and adverse events did not correlate with mutation load in blood or urine or with ragged-red fibers on muscle biopsy.
DiagnosisJanssen et al. (2008) defined the 'mitochondrial energy-generating system' (MEGS) capacity as a measurement encompassing mitochondrial enzymatic reactions from oxidation of pyruvate to the export of ATP, which can be used as an indicator for overall mitochondrial function. In an analysis of muscle tissue from 24 MELAS patients with the MTTL1 3243A-G mutation (590050.0001), MEGS capacity correlated better with mutation load than did analysis of individual respiratory chain enzyme activities, including complex I, III, and IV. The sensitivity and specificity of measurement using MEGS reached 78% and 100%, respectively, for a mitochondriopathy, which was significantly more accurate than measuring individual enzyme activities alone.
Clinical ManagementIn a patient with MELAS due to the 3243A-G mutation (590050.0001), Costello and Sims (2009) reported safe and effective treatment of symptomatic myoclonus with lamotrigine.
Ma et al. (2015) generated genetically corrected pluripotent stem cells (PSCs) from patients with mtDNA disease. Multiple induced pluripotent stem (iPS) cell lines were derived from patients with common heteroplasmic mutations including 3243A-G (590050.0001), causing MELAS, and 8993T-G (516060.0001) and 13513G-A, implicated in Leigh syndrome. Isogenic MELAS and Leigh syndrome iPS cell lines were generated containing exclusively wildtype or mutant mtDNA through spontaneous segregation of heteroplasmic mtDNA in proliferating fibroblasts. Furthermore, somatic cell nuclear transfer (SCNT) enabled replacement of mutant mtDNA from homoplasmic 8993T-G fibroblasts to generate corrected Leigh-NT1 PSCs. Although Leigh-NT1 PSCs contained donor oocyte wildtype mtDNA (human haplotype D4a) that differed from Leigh syndrome patient haplotype (F1a) at a total of 47 nucleotide sites, Leigh-NT1 cells displayed transcriptomic profiles similar to those in embryo-derived PSCs carrying wildtype mtDNA, indicative of normal nuclear-to-mitochondrial interactions. Moreover, genetically rescued patient PSCs displayed normal metabolic function compared to impaired oxygen consumption and ATP production observed in mutant cells. Ma et al. (2015) concluded that both reprogramming approaches offer complementary strategies for derivation of PSCs containing exclusively wildtype mtDNA, through spontaneous segregation of heteroplasmic mtDNA in individual iPS cell lines or mitochondrial replacement by SCNT in homoplasmic mtDNA-based disease.